06 May Unclear Cap, Ambiguous Course RCA CTO: A Step-by-Step IVUS-Guided Approach
In the complex world of interventional cardiology, managing chronic total occlusions (CTO) with unclear proximal caps and ambiguous vessel courses presents a formidable challenge. This detailed walkthrough shares insights into tackling an RCA mid-RCA CTO with a JCTO score of 2, which borders on 3 due to the ambiguous anatomy. Guided by intravascular ultrasound (IVUS) and a strategic wire escalation approach, this case exemplifies the nuanced techniques needed to navigate difficult CTOs effectively.
Drawing from the expertise of Interventional Strategies, this article unpacks the procedural steps, decision-making processes, and technical nuances involved in overcoming ambiguous proximal caps and vessel pathways. Whether you are an interventional cardiologist or a fellow in training, this comprehensive guide will enrich your understanding of IVUS-guided cap puncture, wire handling, and knuckle wire techniques.
Table of Contents
- Understanding the Case: RCA Mid-RCA CTO with Ambiguous Cap and Course
- Step 1: Localizing the Proximal Cap Using IVUS
- Step 2: Confirming Wire Position and Initial Advancement
- Step 3: Managing Ambiguous Vessel Course with Wire Escalation and Knuckle Technique
- Step 4: Reaching True Lumen and Confirmation
- Step 5: Balloon Dilations and Stent Deployment
- Step 6: Managing Side Branch Complications: Protecting the RV Branch
- Step 7: Final Assessment and Outcome
- Key Takeaways and Lessons Learned
- Frequently Asked Questions (FAQ)
- Conclusion
Understanding the Case: RCA Mid-RCA CTO with Ambiguous Cap and Course
The patient presented with a mid-right coronary artery (RCA) chronic total occlusion. The JCTO (Japanese CTO) score was assessed as 2, but the complexity felt closer to 3 due to the ambiguous proximal cap and unclear vessel trajectory. This ambiguity complicates the initial wiring strategy and increases procedural difficulty.
Key challenges identified were:
- Ambiguous proximal cap: The exact entry point into the occlusion was uncertain, making wire puncture risky.
- Unclear vessel course: The CTO segment’s path was not clearly visible, increasing the chance of subintimal dissection or misdirection.
- Long lesion length: The occlusion spanned a significant length, adding procedural complexity.
Given these factors, the plan was to use IVUS (intravascular ultrasound) to localize the proximal cap precisely, followed by careful cap puncture and wire escalation. IVUS allows visualization beyond angiography, identifying vessel architecture and true lumen location.
Step 1: Localizing the Proximal Cap Using IVUS
The first step involved performing an IVUS run to identify the ambiguous proximal cap. The angiogram showed a size jump and the disappearance of the media layer at approximately 12:00 on the vessel clock face, indicating the probable cap location.
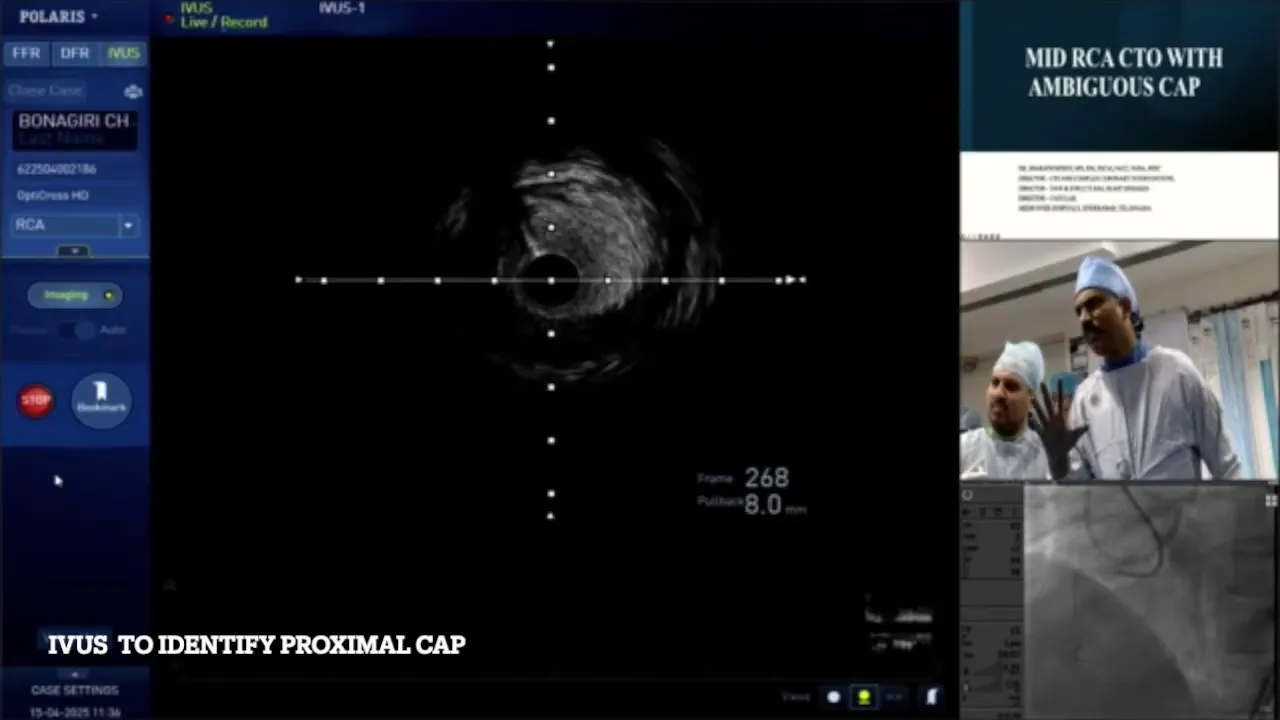
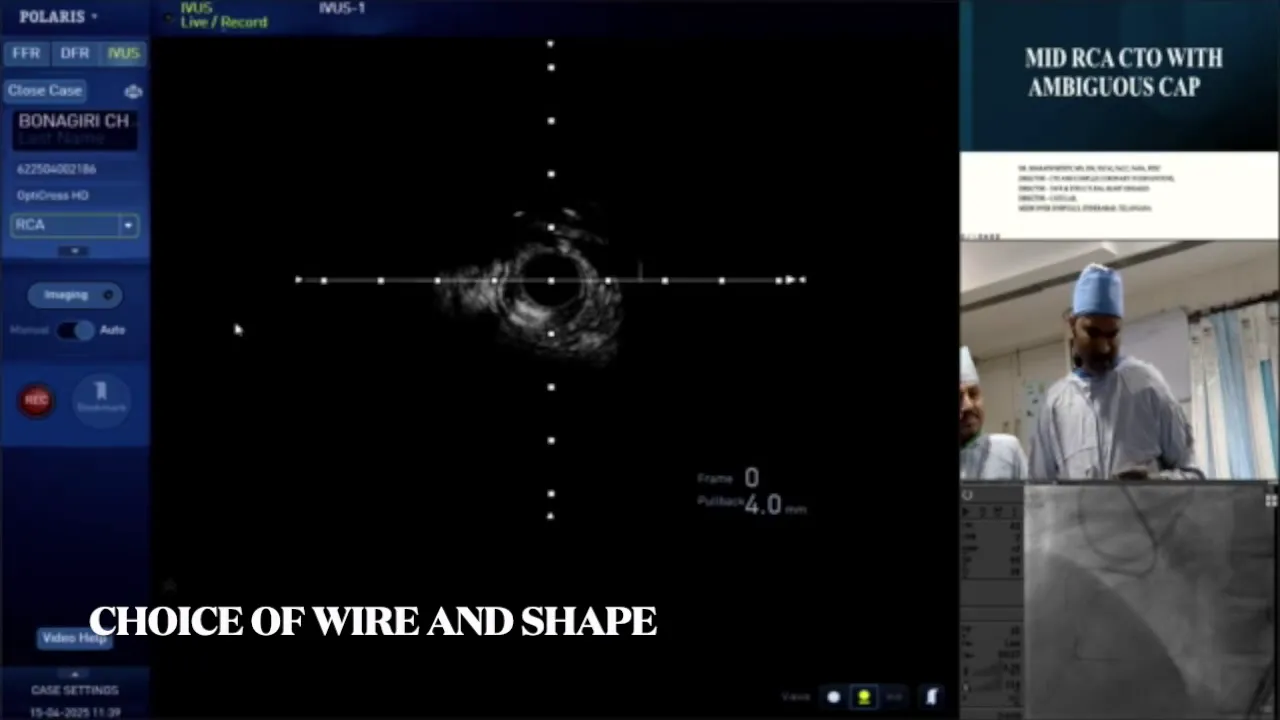
Using a fine cross catheter and a stiff wire (Hornet 14), the proximal cap was targeted. The Hornet wire is favored for proximal cap puncture due to its stiffness and penetration ability, especially when bent with two distinct angles to facilitate directional control.
Important technical notes during this step:
- Wire shaping: Two bends were applied to the Hornet wire for precise navigation.
- Catheter manipulation: The microcatheter was pulled back and advanced carefully to differentiate the second wire and confirm its position.
- Flushing protocol: Flushing was done only if resistance or issues were felt, avoiding unnecessary flushing to maintain wire control.
Step 2: Confirming Wire Position and Initial Advancement
Once the Hornet wire punctured the proximal cap, the microcatheter was advanced carefully. The operator emphasized not pushing the wire aggressively but rather rotating it and allowing it to follow the vessel’s natural course. This approach minimizes the risk of creating false lumens or vessel perforation.
Wire position was confirmed via multiple angiographic views, including RAO (right anterior oblique) and cranial projections, which helped ascertain whether the wire remained within the vessel architecture.

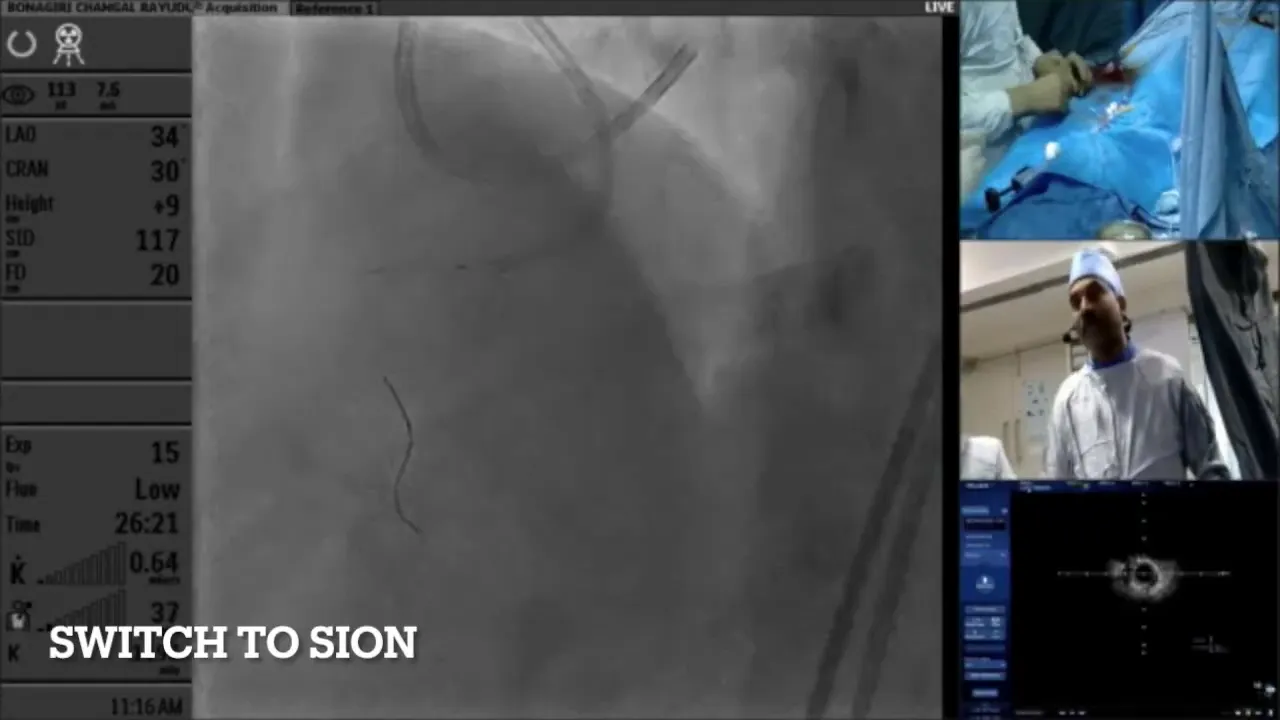
At this stage, a challenge arose: the distal wire position was ambiguous, and the course was unclear. To manage this, the wire was de-escalated to a GIA wire, which is softer, allowing safer navigation when the vessel path is uncertain.
Step 3: Managing Ambiguous Vessel Course with Wire Escalation and Knuckle Technique
Despite de-escalating to the GIA wire, the course of the CTO remained unclear, with the wire tending to enter side branches or subintimal spaces. The operator then escalated to a Pilot 200 wire, but ambiguity persisted.
At this juncture, the knuckle wire technique was employed. This involves creating a loop or “knuckle” in the wire to safely navigate longer occlusions and ambiguous courses by advancing through the subintimal space while minimizing vessel trauma.
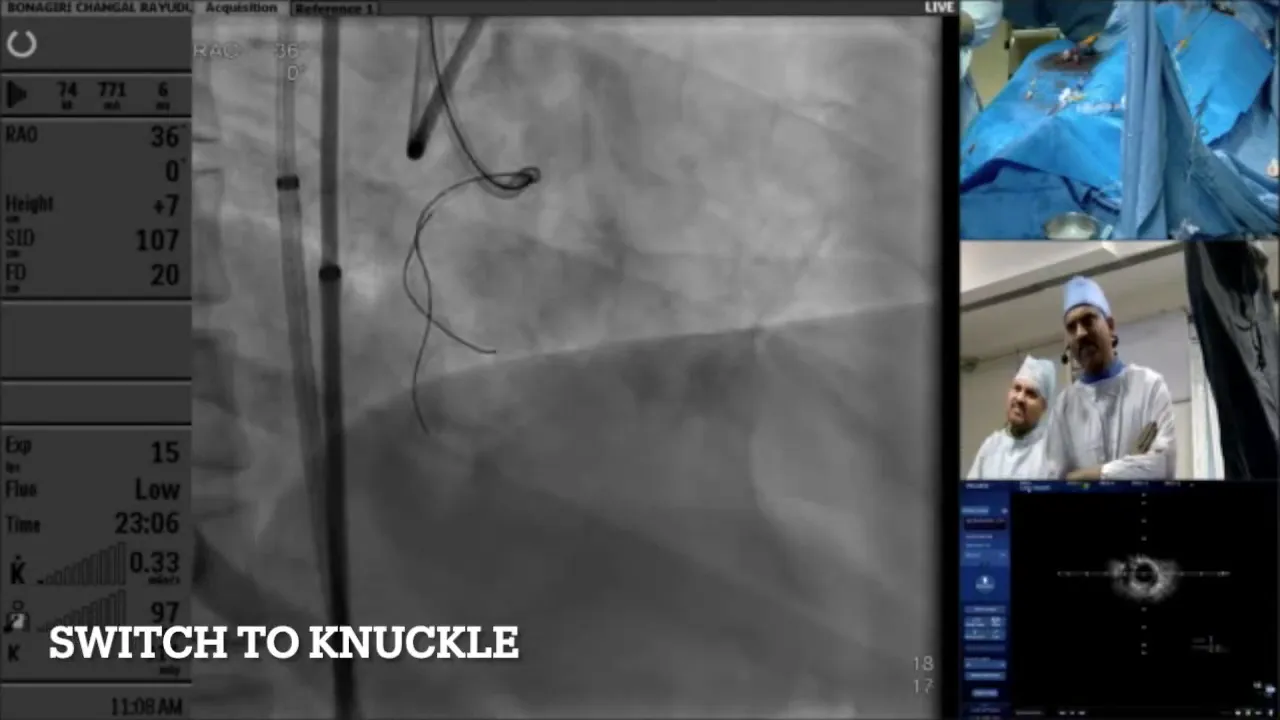
The knuckle wire was advanced with the support of a microcatheter and a proximal balloon, which was inflated to trap the microcatheter and provide stability. The balloon also ensured that the subintimal space did not expand excessively.
Key points about the knuckle wire technique:
- Creating the knuckle wire loop after space was created with previous wire attempts.
- Using balloon trapping to provide support and prevent microcatheter dislodgement.
- Advancing slowly and confirming position with fluoroscopy and IVUS.

Step 4: Reaching True Lumen and Confirmation
After advancing the knuckle wire, the operator used a low-tip-load Scion wire to confirm true lumen entry. This wire buckles if it encounters subintimal space, serving as a safety check.
Multiple branches were probed to ensure the wire was within the true lumen. Retrograde injections were performed to confirm wire position before proceeding further.
Once confirmed, the balloon was deflated, and further balloon dilations were performed to prepare the vessel for stenting. The operator used balloons of varying sizes—starting with 2.5mm and progressing to 3.5mm non-compliant (NC) balloons.
Step 5: Balloon Dilations and Stent Deployment
Balloon dilations were performed cautiously with gradual pressure escalation. Negative pressure techniques were employed to reduce the risk of vessel dissection and ensure optimal balloon apposition.
Following adequate preparation, stenting was performed, with care taken to avoid complications such as malposition or side branch occlusion.

The operator noted the importance of defining wire position—intimal versus subintimal—before stenting to avoid complications. IVUS imaging was used to assess stent apposition and vessel status post-deployment.
Step 6: Managing Side Branch Complications: Protecting the RV Branch
During the procedure, the patient developed hypotension, likely due to occlusion of the single right ventricular (RV) branch. To prevent permanent occlusion, the RV branch was rewired and protected.
A kissing balloon technique was employed to dilate both the main vessel and the RV branch simultaneously, maintaining patency and restoring flow.
Step 7: Final Assessment and Outcome
After stent deployment and side branch protection, final angiographic and IVUS assessments showed:
- Good stent expansion with minimal malposition corrected by high-pressure ballooning.
- Restored flow in the main RCA and preserved RV branch patency.
- Only a small area of false lumen noted, with the majority of the vessel in true lumen.
The operator concluded that despite the ambiguous cap and course, the IVUS-guided cap puncture combined with wire escalation and knuckle wire technique allowed successful crossing and revascularization of the RCA CTO.
Key Takeaways and Lessons Learned
This case highlights several important principles when dealing with ambiguous cap and vessel course in CTO interventions:
- IVUS guidance is critical: It helps precisely localize the proximal cap, identify vessel architecture, and confirm wire position.
- Wire selection and shaping matter: Using stiff wires like Hornet for cap puncture and softer wires like GIA or Pilot for ambiguous courses reduces vessel injury risk.
- Patience and technique are essential: Rotating wires gently and allowing them to follow natural vessel paths prevent false lumens and perforations.
- Knuckle wire technique is useful: Creating a knuckle facilitates crossing long or ambiguous occlusions safely.
- Side branch protection is vital: Protect branches like the RV branch to avoid ischemic complications and hemodynamic instability.
- Balloon trapping and escalation: Using balloons to trap microcatheters provides support for wire manipulation and prevents dislodgement.
Frequently Asked Questions (FAQ)
What is an ambiguous proximal cap and why does it complicate CTO intervention?
An ambiguous proximal cap refers to an unclear or indistinct starting point of the occlusion on angiography. It complicates intervention because the operator cannot confidently identify where to puncture the occlusion, increasing the risk of vessel dissection or perforation.
How does IVUS help in managing ambiguous caps?
IVUS provides cross-sectional vessel images beyond what angiography shows, allowing visualization of the vessel wall layers, true lumen, and occlusion cap. This helps localize the exact entry point for safe wire puncture.
What is the rationale for using wire escalation in CTO procedures?
Wire escalation involves starting with softer wires that are safer but less penetrative and gradually moving to stiffer, more penetrating wires as needed. This strategy balances safety with effectiveness, reducing vessel trauma while enabling crossing of tough lesions.
Can you explain the knuckle wire technique?
The knuckle wire technique involves forming a loop or “knuckle” with the wire tip, which is then advanced through the occlusion. This loop reduces the risk of vessel perforation by distributing force over a wider area and is especially useful in ambiguous or long occlusions.
How do you protect side branches during CTO interventions?
Side branches can be protected by wiring them separately and using techniques like kissing balloon dilations, where balloons are inflated simultaneously in the main vessel and branch to maintain patency and prevent occlusion.
What are the risks of subintimal wiring and how can they be minimized?
Subintimal wiring can lead to vessel dissection, false lumen creation, or perforation. These risks are minimized by careful wire manipulation, using IVUS for guidance, choosing appropriate wires, and confirming true lumen entry before ballooning or stenting.
Conclusion
Managing CTOs with unclear caps and ambiguous vessel courses demands a blend of advanced imaging, strategic wire selection, and meticulous technique. This case of an RCA mid-CTO demonstrates how IVUS-guided cap puncture, wire escalation, and knuckle wire techniques can be harmonized to achieve successful revascularization.
By following these principles and maintaining patience and precision, interventional cardiologists can navigate even the most challenging CTOs, improving patient outcomes and expanding the boundaries of percutaneous coronary interventions.
For more insights and case discussions, visit Interventional Strategies.


No Comments