Percutaneous Coronary
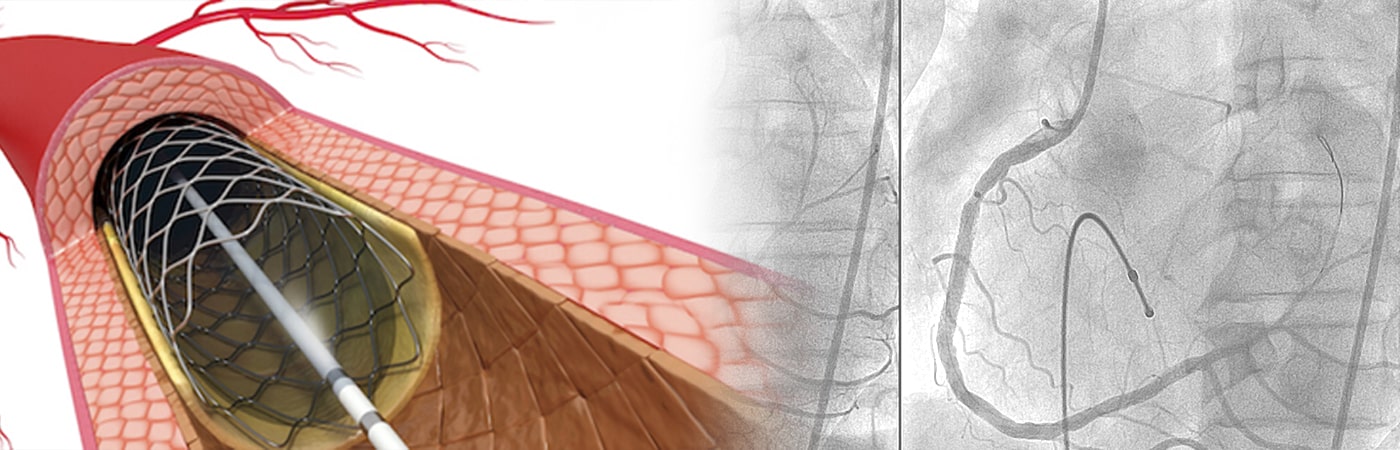
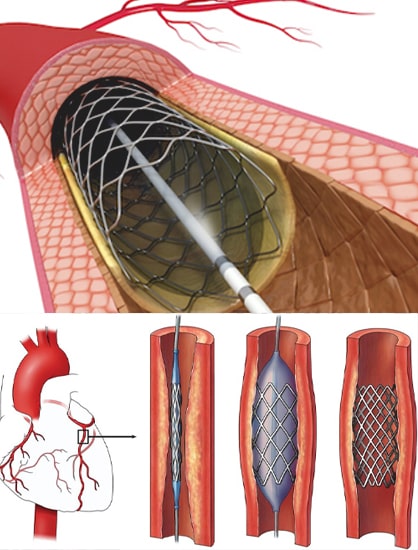
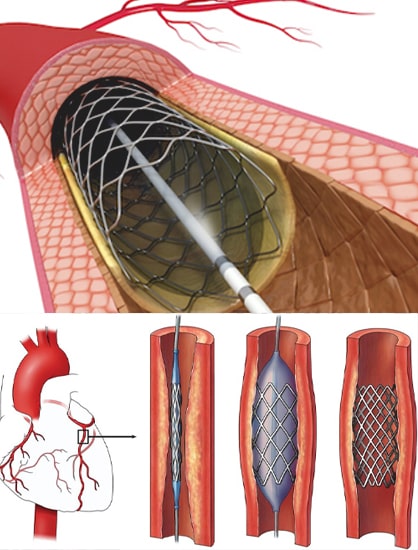
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a nonsurgical technique for treating obstructive coronary artery disease, including unstable angina, acute myocardial infarction (MI), and multivessel coronary artery disease (CAD) procedure that improves blood flow to your heart.
PCI requires cardiac catheterization, which is the insertion of a catheter tube and injection of contrast dye, usually iodine-based, into your coronary arteries.
The treatment is minimally invasive and relies on thin tubes called catheters. Doctors enter the body through an artery in the wrist or leg, and then thread catheters toward the heart.
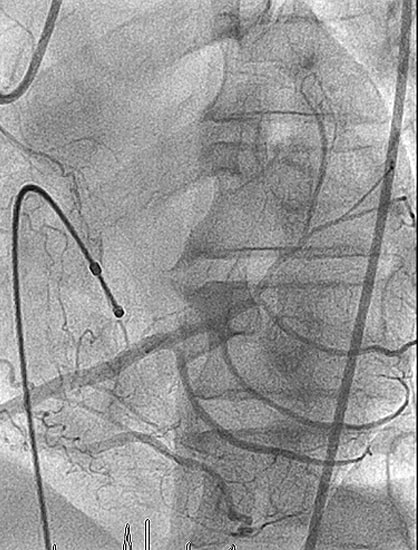
They use contrast dye and X-rays to guide their work. This imaging procedure is called an angiogram and is a type of cardiac catheterization.

Risk Factors
Ciggerate Smoking

Clinical
Indications
Acute ST-elevation myocardial infarction (STEMI)

Conditions Treated
Using PCI
Obstructive coronary artery disease
Spontaneous coronary artery dissection (SCAD)
Types of
Percutaneous Coronary
Interventions
Before the procedure
- Shortly before your procedure, you may receive a sedative to help you relax. For most PCIs, patients are sedated but not asleep.
- Your hair may be clipped in the area where a catheter will be inserted, such as the groin or wrist.
- An intravenous (IV) line is placed, allowing us to give you medications quickly, if necessary.
- Electrodes will be placed on your body to monitor your heart, and a small device called a pulse oximeter may be clipped on a finger or ear to track the oxygen level in your blood.

During the procedure
- A PCI may take from one hour to three hours, depending on complexity.
- You will lie on your back on a procedure table. A local anesthetic (a medication that temporarily blocks pain signals) will be injected at the site where the catheter will be inserted.
- When the catheter reaches your heart, a contrast dye – a harmless solution that shows up well in medical imaging – will be injected, so that doctors can clearly see the vessel’s narrowed area on an X-ray. The doctors will then perform whichever type of PCI is best for your condition.
- When finished, the catheter will be withdrawn and pressure applied to the insertion site to stop the bleeding.
- If the catheter was inserted through your groin, you will need to stay flat on your back and keep your leg straight for several hours. If the catheter was inserted in your arm, it will be elevated on pillows and kept straight with a stabilizing board.
After the Procedure
- We will take you to a recovery room for several hours of observation. You’ll need to stay in bed for two to six hours, depending on your condition and the type of PCI you had.
- You may experience mild pain or an ache in your chest. If the discomfort is too much, we can give you pain medication.
- You will be encouraged to drink water and other fluids to help flush the contrast dye from your body.
- Some patients spend the night in the hospital for observation, some go home the same day. Your doctor will decide which option is best for you. If you go home the same day, you will need someone to drive you home. You should not operate a motor vehicle for 24 hours after the procedure.
At Home
Contact your doctor for advice if you experience any of the following symptoms:
- You may shower 24 to 48 hours after the procedure.
- For five days, avoid activities that involve lifting and pulling with the wrist.
- During this time, there should be no strenuous exercise; playing sports, such as golf, household chores, such as vacuuming or demanding physical tasks, such as moving furniture.
- A week after your procedure, you can resume activities of moderate intensity.
- moderate physical activity (such as walking, swimming or using a stationary bike) at least five days a week is recommended to strengthen your heart.
Success Rate
- Angioplasty is successful in opening coronary arteries in well over 90% of patients.
- Up to 30% to 40% of patients with successful coronary angioplasty will develop recurrent narrowing at the site of balloon inflation.
- Post CABG PCI
- PCI after CABG
- Low contrast PCI
- Cardiologist for protected PCI
- IMPELLA assisted PCI
- Simple protected PCI
- Protected PCI for IMPELLA
- High risk PCI

