Transcatheter aortic valve replacement/implantation
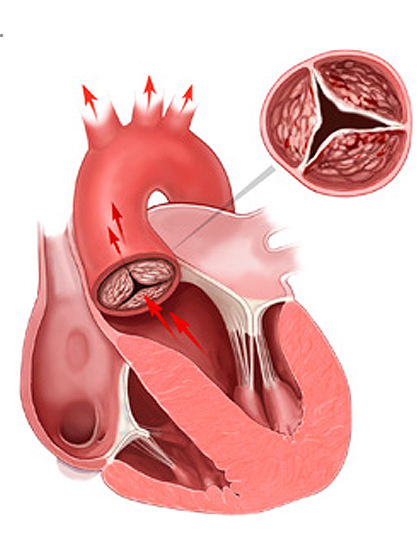
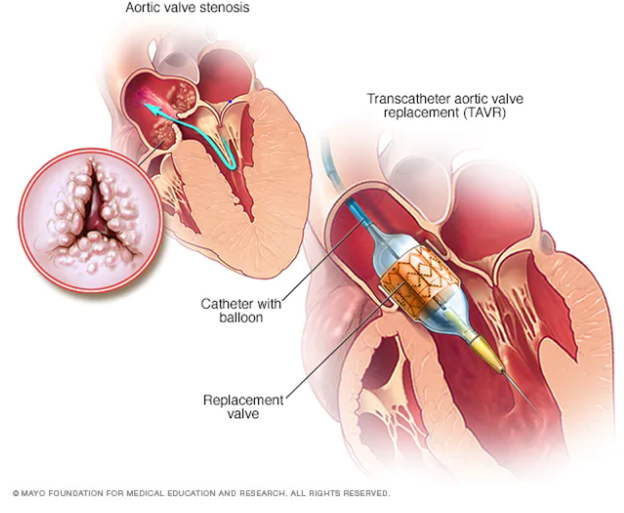
Transcatheter aortic valve replacement (TAVR) is a minimally invasive heart procedure to replace a thickened aortic valve that can’t fully open (aortic valve stenosis). The aortic valve is located between the left lower heart chamber (left ventricle) and the body’s main artery (aorta). If the valve doesn’t open correctly, blood flow from the heart to the body is reduced.
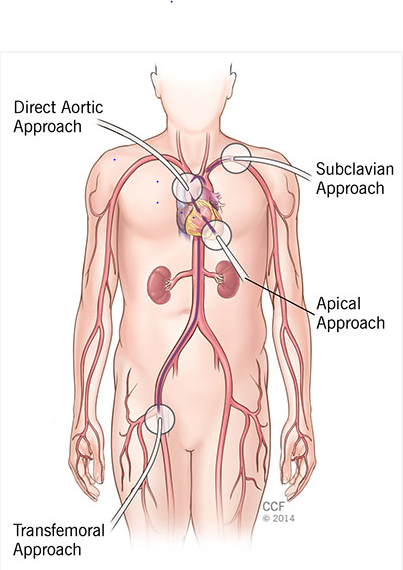
Types of TAVR approaches

TRANSFEMORAL APPROACH

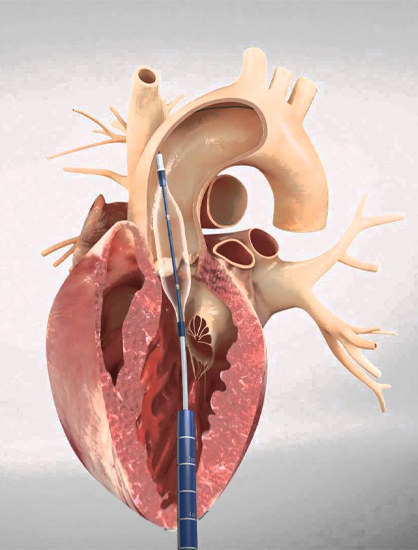
TRANSAPICAL APPROACH

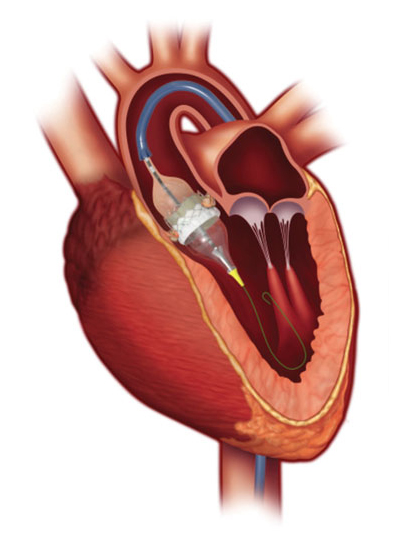
DIRECT AORTIC APPROACH

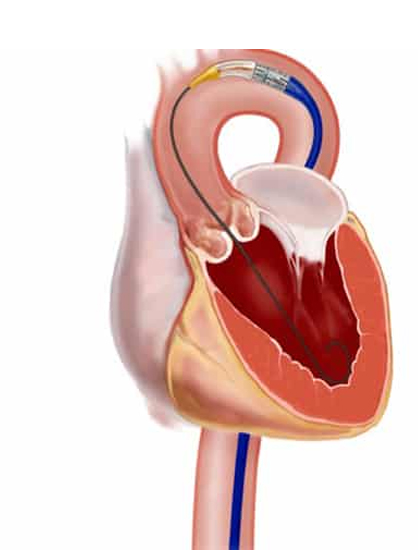
SUBCLAVIAN APPROACH
Types Of TAVI Valves
The Medtronic CoreValve and Edwards’ SAPIEN are the most commonly used TAVR prosthetic valves.
- SAPIEN VALVE
- CORE VALVE
Before the procedure
- Before the day of surgery, you will have a physical exam and tests. These tests include X-rays, CT scans, lung tests, and blood tests. You will have an echocardiogram to check your aortic valve. You may also have a cardiac catheterization..
- Tell your doctor if your allergic to any medications.
- Nill by mouth before few hours of surgery.
- You will be asked to remove jewellary and other objcets that interfere surgery
- You will changed to hospital gown and empty the bladder
- A surgical team will postion you in a operating table lying on your back and give IV medications and fluids, more catheters will be put in blood vessels to monitor your heart and blood pressure.
- Before your surgery, you may receive general anesthesia. This will put you in a pain-free sleep. Most often, the procedure is done with you heavily sedated. You are not completely asleep but you do not feel pain. This is called moderate sedation.
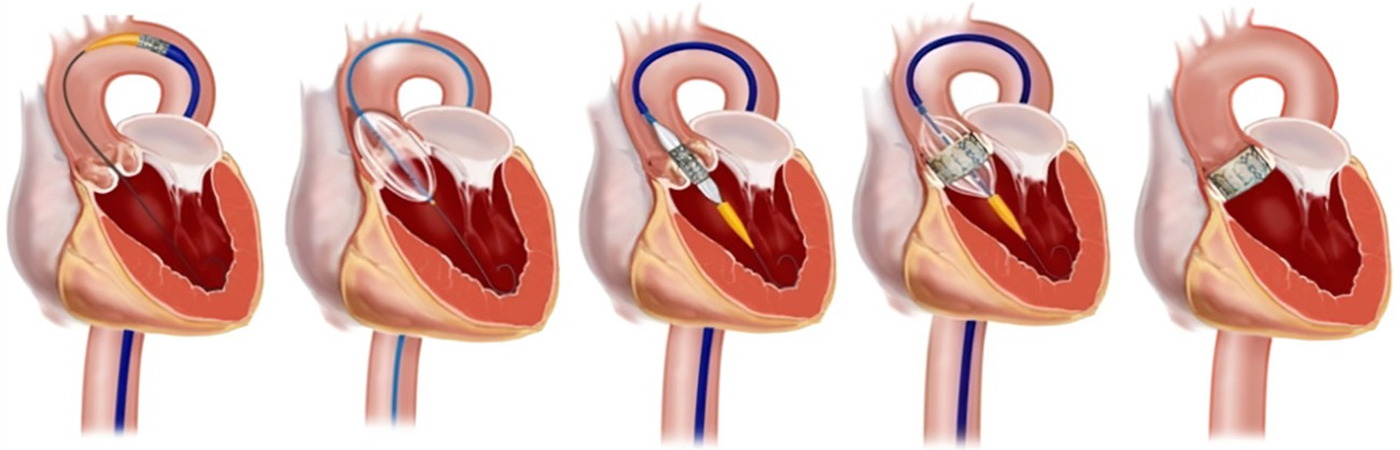
During the procedure
- Transcatheter aortic valve replacement (TAVR) involves replacing a damaged aortic valve with one made from cow or pig heart tissue (biological tissue valve).
- Sometimes, the biological tissue valve is placed into an existing biological tissue valve that is no longer working.
- To perform TAVR docors inserts a catheter into a blood vessel, usually in the groin or chest area, and guides it into the heart. Moving x-ray images or echocardiogram pictures helps the doctor place the catheter in to the correct positon.
- A replacement valve made of cow or pig tissue is passed through the hollow catheter and placed in the area of the aortic valve. A balloon on the catheter tip inflates to press the new valve into place. Some valves expand without the use of a balloon.
- The doctor removes the catheter once the new valve is securly in place.
- The anesthesiologist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
- You do not need to be on a heart lung mechine for this procedure
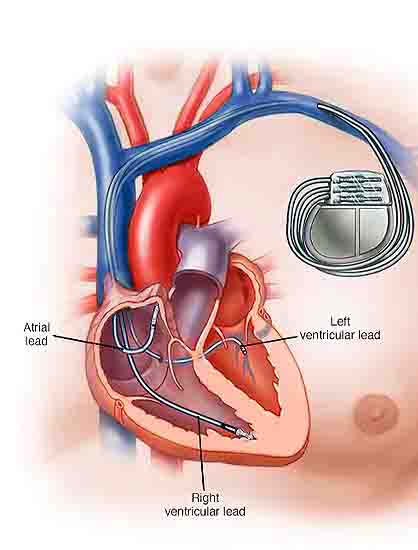
Pacemaker
- Every patient receives a temporary pacemaker during the TAVR procedure. A pacemaker is a device that uses electrical impulses to regulate your heart rhythm.
- This is a small wire through your vein in your leg into your heart that is most often taken out right after the procedure.
- Sometimes a permanent pacemaker is needed after a TAVR procedure. If a permanent pacemaker is needed, this will likely be placed while you are in the hospital the day after your TAVR procedure.
After the procedure
- You may spend the night in the intensive care unit (ICU) for monitoring after your procedure. How long you need to stay in the hospital after TAVR depends on many things. Some people who have TAVR go home the next day.
- Before you leave the hospital, your treatment team will explain how to care for any incisions and how to watch for signs and symptoms of infection.
- Warning signs of infection include
- Fever
- increased pain
- redness
- swelling
- draining
- oozing at the catheter site

Causes
Age

Sign and Symptoms
Shortness of breath with exertion

Tests
Chest x-ray

Benefits
Excellent alternative to open heart surgery

Risk Factors/
Complications
Bleeding during or after the surgery

Pre-operative
investigations
ECG
Contraindications
1.Life expectency less than 12 months
2.Myocardial infraction with in last 30 days
3.Congenital unicuspid
4.Bicuspid
5.Cardiomyopathy
6.Short distance between the annulus and coronary ostium
7.Need for emergency surgery
8.Severe pulmonary hypertension
9.Echocardiographic evidence of intracardiac mass
10.End stage renal disease
Management therapy
1. Blood thinners (anticoagulants): Blood-thinning medication is prescribed to prevent blood clots. Your doctor will explain how long you may need to take this medicine. Always take medications as prescribed.
2. Antibiotics: Artificial heart valves can become infected with bacteria. Most bacteria that cause heart valve infections come from the bacteria in the mouth. Excellent dental hygiene, including routine dental cleanings, can help prevent these infections. Antibiotics are prescribed for use before certain dental procedures.
Follow up appointments
1.Within one week
2.One month – you will have an echocardiogram before you see your cardiologist. This appointment will take about 2 hours. You may have other testing as needed.
3.One year – you will have an echocardiogram before you see your cardiologist. This appointment will take about 2 hours. Your may have other testing as needed. You will receive a follow-up phone call in 1 to 3 days to see how you are doing
Life style modification
1.No smoking
2.Regular exercises
3.Maintain a healthy weight
4.Eat a healthydiet rich in fruits and veggies and low intake of salt(2000-3000 mg/ day) and saturated and trans fats
Self care
1.You may shower.
2.Do not scrub your incision site.
3.Pat the incision site dry, do not rub.
4.Do not use ointments or perfumes.
5.No bath tubs, hot tubs, or pools for one week after surgery.
6.Cough and deep breathe using your incentive spirometer 5 to 10 times each hour while you are awake.
7.Weigh yourself at the same time each day. Write your weight down.
Food to Avoid
1.Fatty meats
2.Fried food
3.Refined with carbohydrates
4.Sugary drinks such as soda
5.Fatty oils such as butter
6.Processed and packaged foods
7.High cholesterol foods
8.Full fatty dairy products
When to call your doctor
1.If your incision is any of the following: – Red – Swollen – Warm to touch – Draining – Opened up
2.Temperature is 101 degrees or higher
3.Severe or increased pain in your incision
4.Abdominal (belly) pain with a firm abdomen
5.Not able to pass gas
6.Not able to have a bowel movement (poop)
7.Change of color or temperature in your foot or hand
8.Numbness
9.Trouble breathing
10.Unusual pain in legs
11.Swelling in legs
12.Back pain
13.If you have any questions or concerns

