SEVERE HEART PUMPING DYSFUNCTION/ HEART FAILURE
Heart failure is a disorder in which the heart is unable to keep up the demands of the body, leading to reduced blood flow, back up of blood in the veins and lungs or other changes that may further weaken or stiffen the heart.
Heart failure does not means that the heart has stopped it means heart cannot keep up the work required to pump adequate blood to all parts of the body.
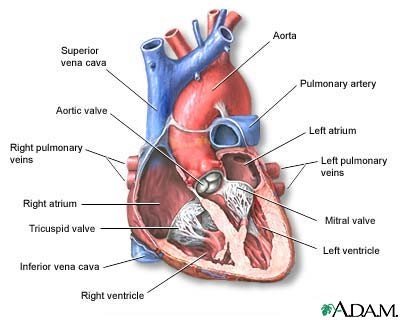
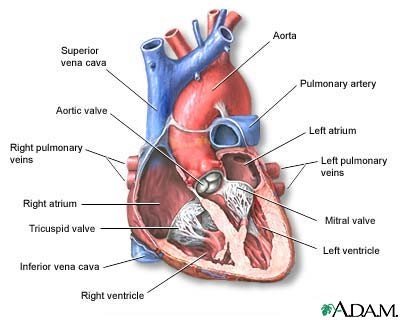
The function of the heart is to pump. The right side of the heart pumps blood from the veins in to the lungs. The left side of the heart pumps blood from the lungs out through the arteries to the rest of the body.
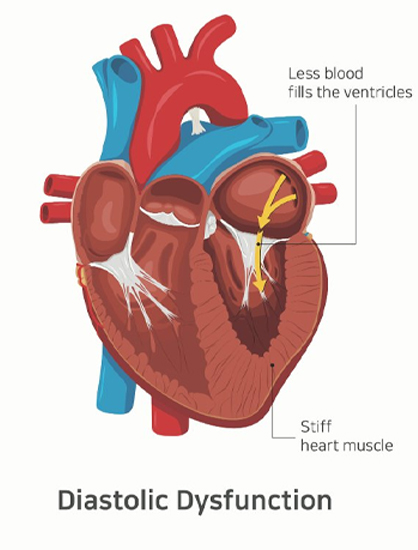
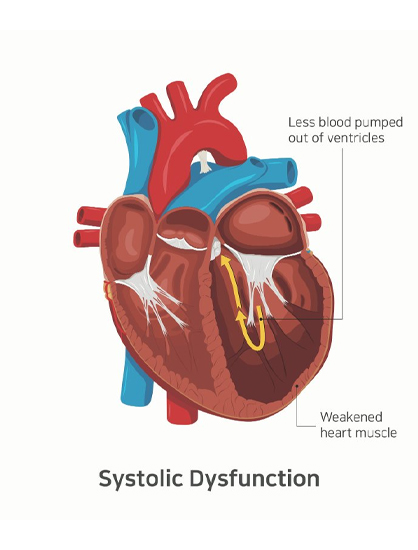
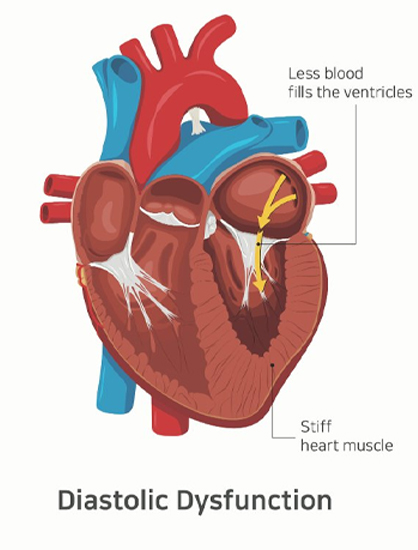
Blood goes out of the heart when the heart muscle contracts (called systole) and comes into the heart when the heart muscle relaxes (called diastole).
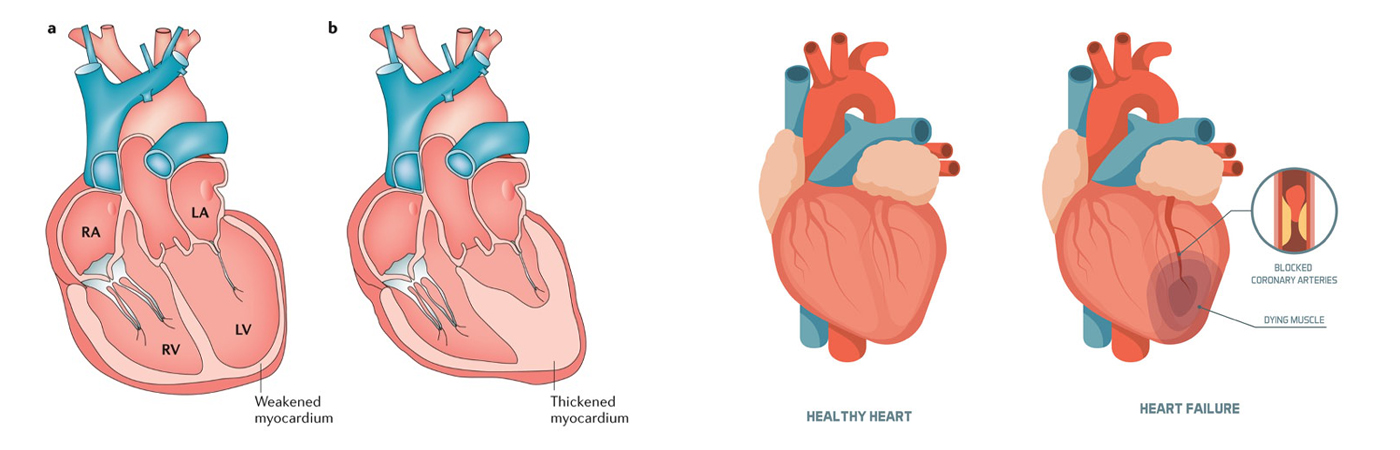
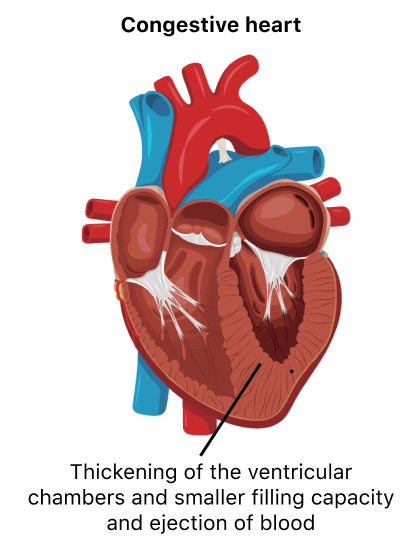
Heart failure develops when the contracting or the relaxing action of the heart is inadequate, typically because the heart muscle is weak, stiff, or both. Heart failure may be described as left sided heart failure or right sided heart failure.
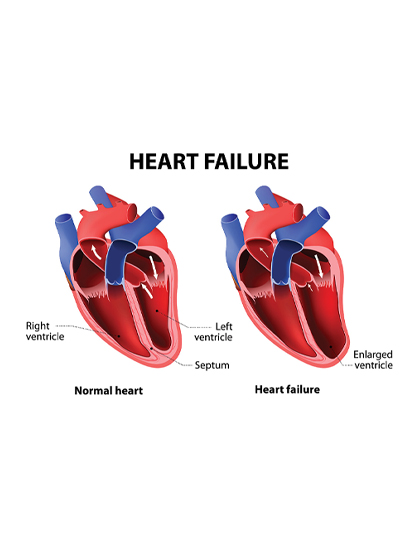
The main pumping chambers of the heart (the ventricles)
- Left side heart failure: Fluid may backup in the lungs, causing shortness of breath.
- Right side heart failure: Fluid may back up in to the abdomen, legs and feet, causing swelling.
- Systolic heart failure: The left ventricle cannot contract vigorously, indicating pumping problem.
- Heart failure with preserved ejection fraction: The left ventricle cannot relax or full fully indicating a filling problem.
Types of heart failure
The heart failure is classified by the ejection fraction (EF), which is the percentage of blood pumped out by the heart with each beat. A normal left ventricular ejects about 55 to 60% of blood.

Heart failure with reduced ejection fraction (systolic heart failure)

Heart failure with preserved ejection fraction (diastolic heart failure)

Heart failure with mid range ejection fraction
New York heart association classified a scale on heat failure
- Class I heart failure: There are no heart failure symptoms.
- Class II heart failure: Everyday activities can be done without difficulty but exertion causes shortness of breath or fatigue.
- Class III heart failure: It is difficult to complete everyday activities.
- Class IV heart failure: Shortness of breath occurs even at rest. This category includes the most severe heart failure.

Causes
High blood pressure.

Sign and Symptoms
Shortness of breath

Diagnosis
Blood tests

Prevention
Preventing heart failure involves treating the disorders that causing heart failure

Complications
Kidney damage or failure
Drugs for heart failure
- Drugs to relive symptoms: Diuretics, Nitrates, Digoxin
- Drugs the helps to improve survival: Angiotensin converting enzyme inhibitors, Beta blockers, Aldosteron antagonist, Angiotensin II receptor blockers, Angiotensin receptor inhibitors, Sodium glucose co-transporter 2 inhibitors, sinus node inhibitors.
The type of drug used depends on the type of heart failure. In systolic heart failure all the drug classes are helpful. In diastolic heart failure only ACE inhibitors, ARBs, Aldosterone antagonists and beta-blockers are typically used.

The following surgeries and devises may be required for some patients with heart failure
1. Heart bypass surgery
Heart bypass surgery creates a new route, called a bypass, for blood and oxygen to go around a blockage to reach your heart. The patient will be given general anesthesia. Once the patient is unconscious the heart surgeon will make an 8 to 10-inch (20.5 to 25.5 cm) surgical cut in the middle of your chest. Your breastbone will be separated to create an opening. This allows your surgeon to see your heart and aorta, the main blood vessel leading from the heart to the rest of your body.
Most people who have coronary bypass surgery are connected to a heart-lung bypass machine, or bypass pump. Your heart is stopped while you are connected to this machine. This machine does the work of your heart and lungs while your heart is stopped for the surgery. The machine adds oxygen to your blood, moves blood through your body, and removes carbon dioxide.
Risks
Prognosis
2. Heart valve surgery
Heart valve surgery is used to repair or replace diseased heart valves. Blood that flows between different chambers of your heart must flow through a heart valve. Blood that flows out of your heart into large arteries must also flow through a heart valve.
There are 4 valves in your heart:
- Aortic valve
- Mitral valve
- Tricuspid valve
- Pulmonic valve
Aortic valve and mitral valve are the most common valve to be repaired. Rarely tricuspic and pulmonic valve replaced or repaired.
Before surgery you will receive general anesthesia.
In open heart surgery, the surgeon makes a large surgical cut in your breastbone to reach the heart and aorta. You are connected to a heart-lung bypass machine if your heart is stopped while connecting to this machine. This machine does the work of your heart, providing oxygen and removing carbon dioxide.
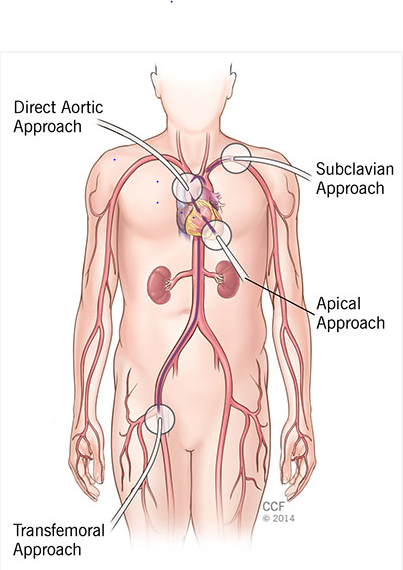
Minimally invasive valve surgery is done through much smaller cuts than open surgery, or through a catheter inserted through the skin. Several different techniques are used:
- Percutaneous surgery
- Robot surgery
If surgeon can repair mitral valve
If your valve is too damaged then the valve replacement to be done
3. Heart pacemaker
A pacemaker is a small, battery-operated device. This device senses when your heart is beating irregular or too slowly
- Pacemakers weigh as little as 1 ounce (28 grams). Most pacemakers have 2 parts.
- The generator contains the battery and the information to control the heartbeat.
- The leads are wires that connect the heart to the generator and carry the electrical messages to the heart.
- A pacemaker is implanted under the skin this procedure takes 1 hour in most of the cases
- You will be awake during the procedure
- A small incision is made on the left side of the chest below your collarbone. A pacemaker generator is then placed under the skin at this location
- Using live x-ray to see the area the doctors puts the leads through the cuts in to the veins and then in to heart. This leads are connected to the generator. There are two types
- Transcutaneous pacemaker
- Transvenous pacemaker
Why the procedure is performed
Risks
Prognosis
4. Implantable Cardioverter-defibrillator
ICD is a device that detects any life threatening, rapid heat beat. If an arrhythmia occurs ICD quickly sends an electrical shock to the heart. The shock changes the rhythm back to normal. This is called defibrillation.
The ICD is made of 3 parts
- The pulse generator contains battery and electrical circuit that reads the electrical activity of your heart
- Your ICD has 1, 2, 3 electrodes. Most ICD has built in pacemaker.
- There is a special kind of ICD called a subcutaneous ICD. This device has a lead that is placed in the tissue to the left of the breastbone rather than in the heart. This type of ICD cannot also be a pacemaker.
- The surgeon will place the electrode into a vein, then into your heart. This is done using a special x-ray to see inside your chest. Then the surgeon will connect the electrodes to the pulse generator and pacemaker. This procedure takes 2 to 3 hours.
Why the procedure is performed
Risks
Prognosis
End stage heart failure
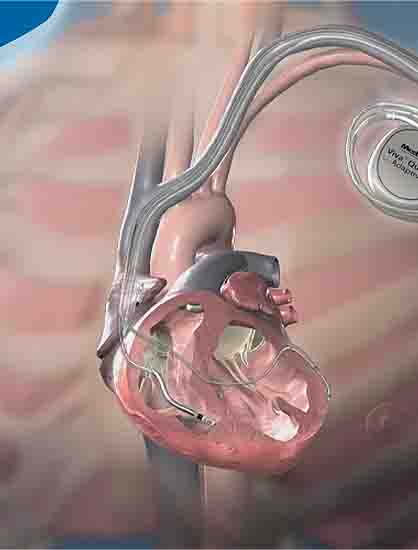
Ventricular assist device
Ventricular assist devices (VADs) help your heart pump blood from one of the main pumping chambers to the rest of your body or to the other side of the heart. These pumps are implanted in your body. In most cases they are connected to machinery outside your body.
A ventricular assist device has 3 parts:
Pump: The pump weighs 1 to 2 pounds (0.5 to 1 kilogram). It is placed inside or outside of your belly.
An electronic controller: The controller is like a small computer that controls how the pump works.
Batteries or another power source: The batteries are carried outside your body. They are connected to the pump with a cable that goes into your belly.

During surgery

Why the procedure is performed

Risks

Prognosis

Overall prognosis of heart failure

When to contact medical professional

Alternative names