09 Jun Parallel Wire Technique: A Comprehensive Guide by Dr. Sharath Reddy Annam
The Parallel Wire Technique is a critical strategy in the field of interventional cardiology, especially when dealing with complex chronic total occlusions (CTOs). In this detailed guide, we explore the insights shared by Dr. Sharath Reddy Annam, a leading expert in the field, who breaks down the nuances of this technique in a live lecture. Whether you are a cardiologist, interventionalist, or a medical professional interested in coronary interventions, understanding the parallel wire technique can enhance your procedural success and patient outcomes.
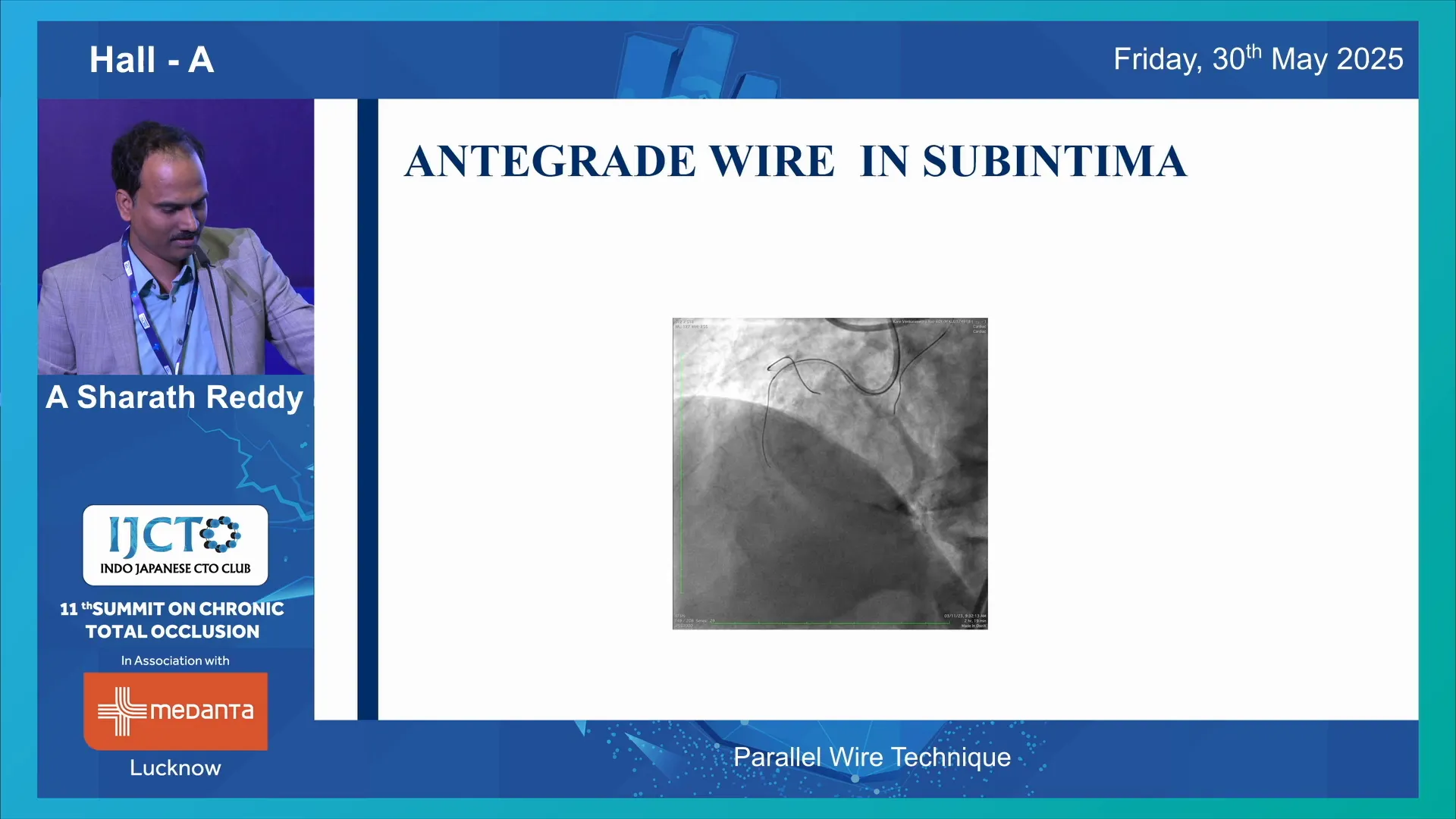
Table of Contents
- Introduction to the Parallel Wire Technique
- Choosing the Right Strategy: The Importance of Distal Vessel Visibility
- How Does the Parallel Wire Technique Work?
- Case Studies Illustrating the Parallel Wire Technique
- When Parallel Wire Technique Fails
- Key Takeaways and Best Practices
- Frequently Asked Questions (FAQs)
- Conclusion
Introduction to the Parallel Wire Technique
Intentional intimal tracking, or navigating within the subintimal space, is a concept frequently encountered during antegrade wiring in CTO interventions. Despite the best intentions, operators often find their initial wire in a suboptimal, subintimal position. For example, Dr. Sharath illustrates this with a case involving a Fielder XTR wire in a mid right coronary system (RCS) CTO, where the wire clearly lies in the subintimal space.
When faced with such a scenario, the interventionalist has several options:
- Pull back and redirect the same wire
- Use a parallel wire alongside the first wire
- Employ a Stingray device to re-enter the true lumen
- Utilize an ISO catheter to enter the subintimal space and attempt re-entry retrogradely
Each option has its place, but the parallel wire technique often stands out as a preferred antegrade strategy due to its relatively high success rate and cost-effectiveness.
Choosing the Right Strategy: The Importance of Distal Vessel Visibility
One of the most important determinants in choosing the parallel wire technique is the clarity of the CTO exit site, particularly the distal vessel visibility on the angiogram. If the distal vessel is well-visualized, the parallel wire technique is usually the best option. It is an antegrade approach with a good success rate and generally costs less than device-based re-entry techniques like the Stingray system.
Dr. Sharath emphasizes that these three techniques—parallel wire, redirecting the first wire, and device-based re-entry—are mutually exclusive. Attempting one technique extensively can cause expansion of the subintimal space, making the other techniques less effective or even impossible to perform afterward.
How Does the Parallel Wire Technique Work?
When the first wire enters the subintimal space, it effectively straightens the vessel to some extent due to its stiffness. This first wire becomes a roadmap for the second wire, allowing the operator to navigate the vessel more precisely than with the first wire alone.
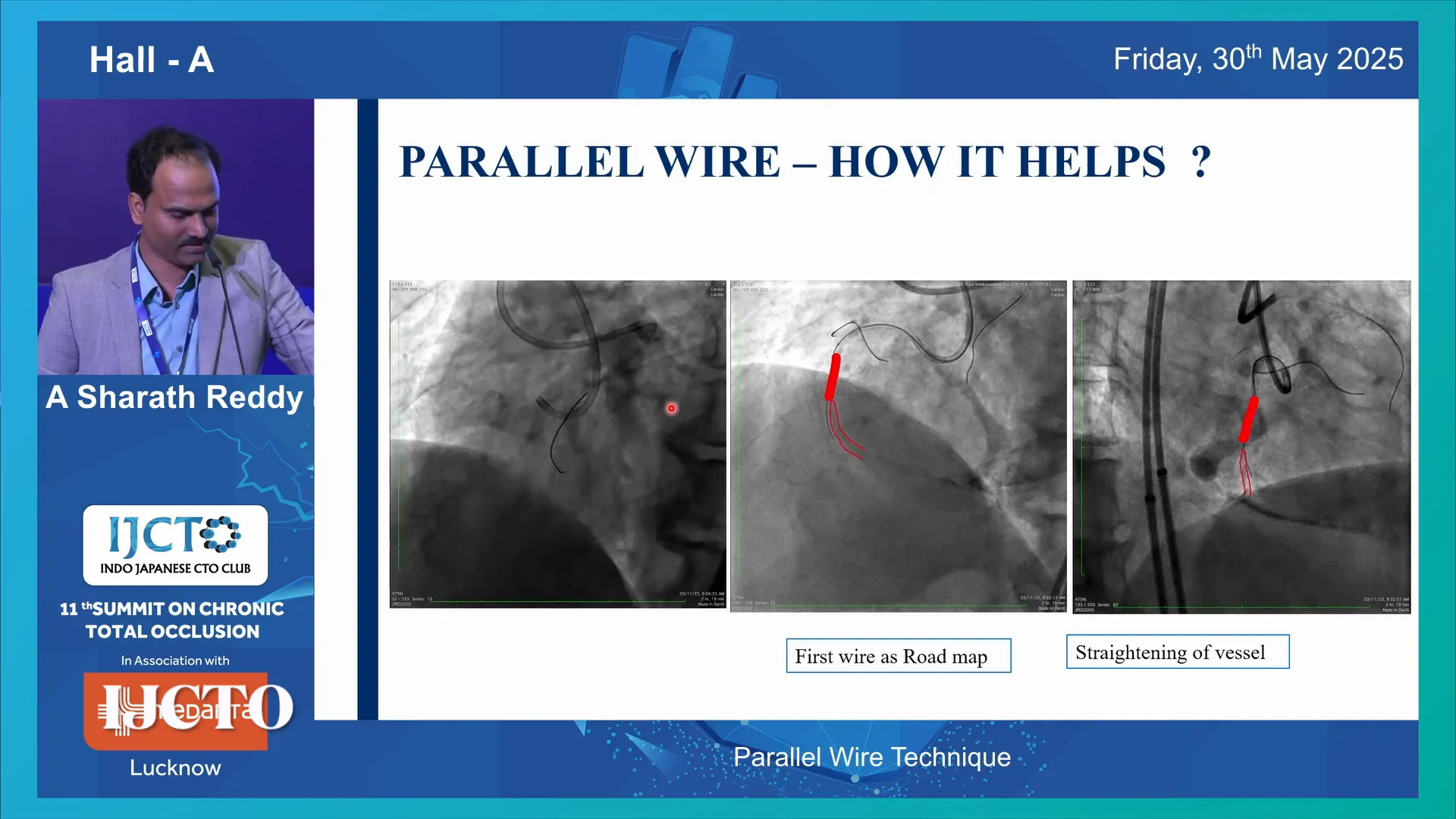
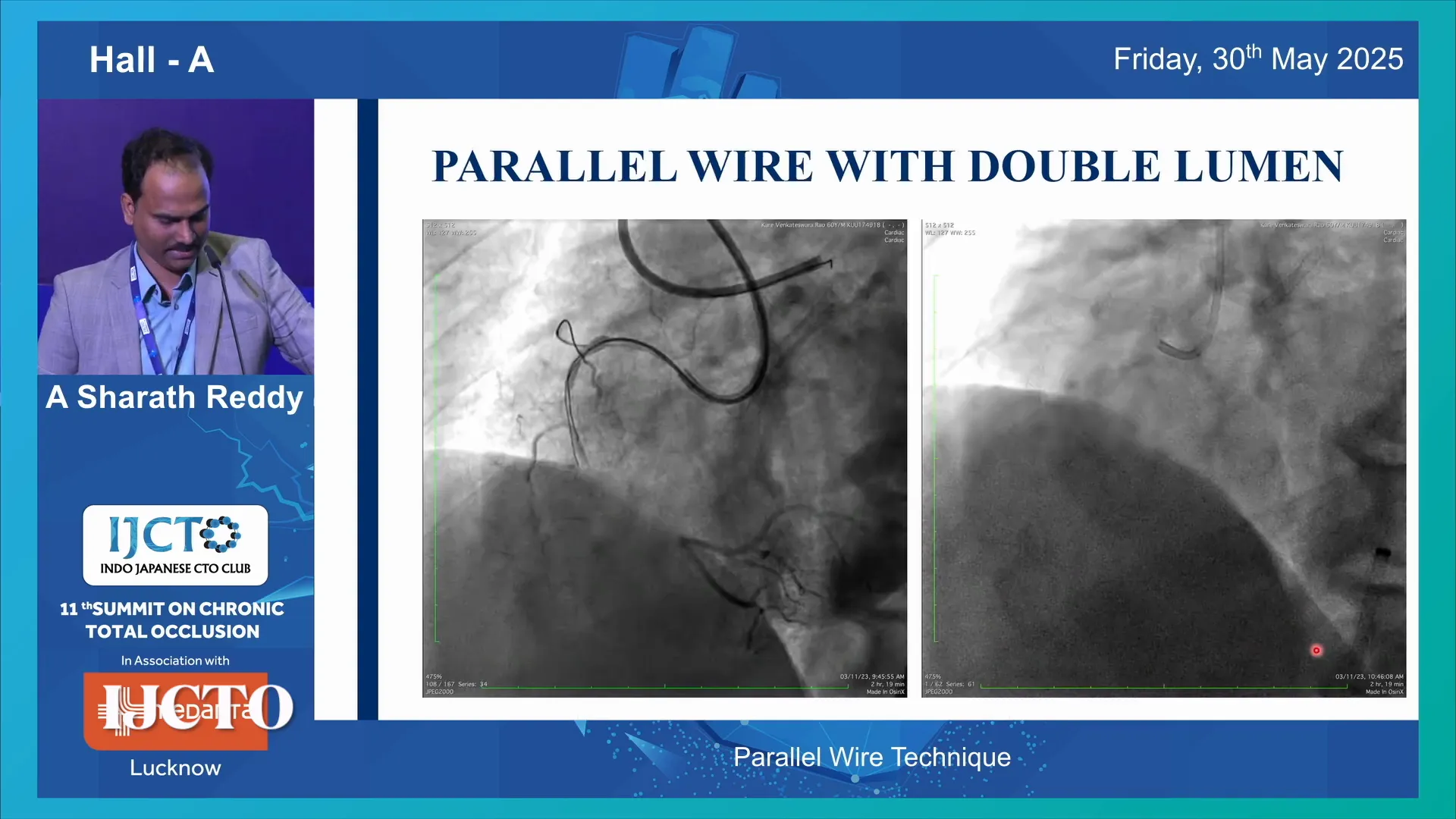
To facilitate this, operators often use a double lumen catheter or a microcatheter positioned parallel to the first wire. The choice of catheter depends on the size of the guiding catheter used initially. The double lumen catheter allows for the introduction of a second wire alongside the first, improving control and access.
Wire Selection for Parallel Wiring
Since the first wire has encountered resistance and entered a low-resistance subintimal plane, the second wire should be capable of breaking through this resistance. This means using a wire with a higher tip load and better steerability.
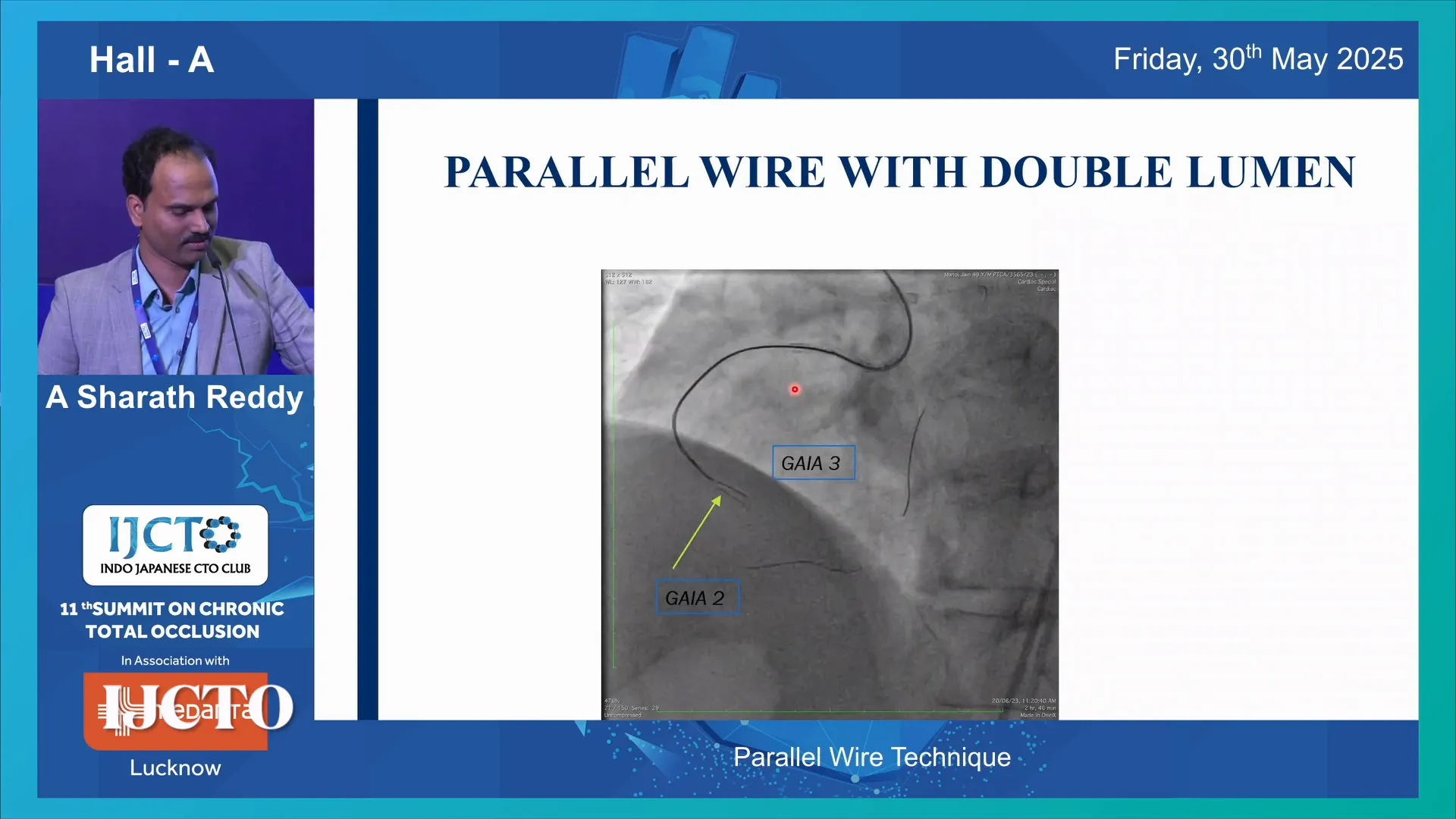
For instance, if the first wire is a Fielder XTR, the next wire might be escalated to a Gaia 2 or Gaia Next 2. If the first wire is already a Gaia 2, escalation to Gaia 3 is considered. Occasionally, operators may de-escalate depending on the situation, but escalation is the norm.
It is critical to confirm the position of the second wire using two orthogonal angiographic views. This ensures the wire is indeed in the true lumen, not subintimal, which is essential to preserving side branches and achieving optimal procedural success.
Case Studies Illustrating the Parallel Wire Technique
Case 1: Mid RCS CTO
In one example, a distal RCS CTO showed a good vessel proximal to the posterior descending artery (PDA) origin. The initial wire, a Fielder XTR, failed to progress, prompting escalation to Gaia 2, which unfortunately also entered the subintimal space.
At this point, a parallel wire technique was attempted using a double lumen catheter and escalating the wire to Gaia 3. Despite this, Gaia 3 also remained subintimal. This case highlights that even with the best roadmap and wire escalation, success is not guaranteed.
In response, Dr. Sharath used two wires simultaneously, navigating one wire with the other as a guide. Switching back to Gaia 2 and advancing it using Gaia 3 as the roadmap, the wire finally reached the distal true lumen. The procedure was completed successfully with wire exchange and final angiographic results showing preserved branch filling.
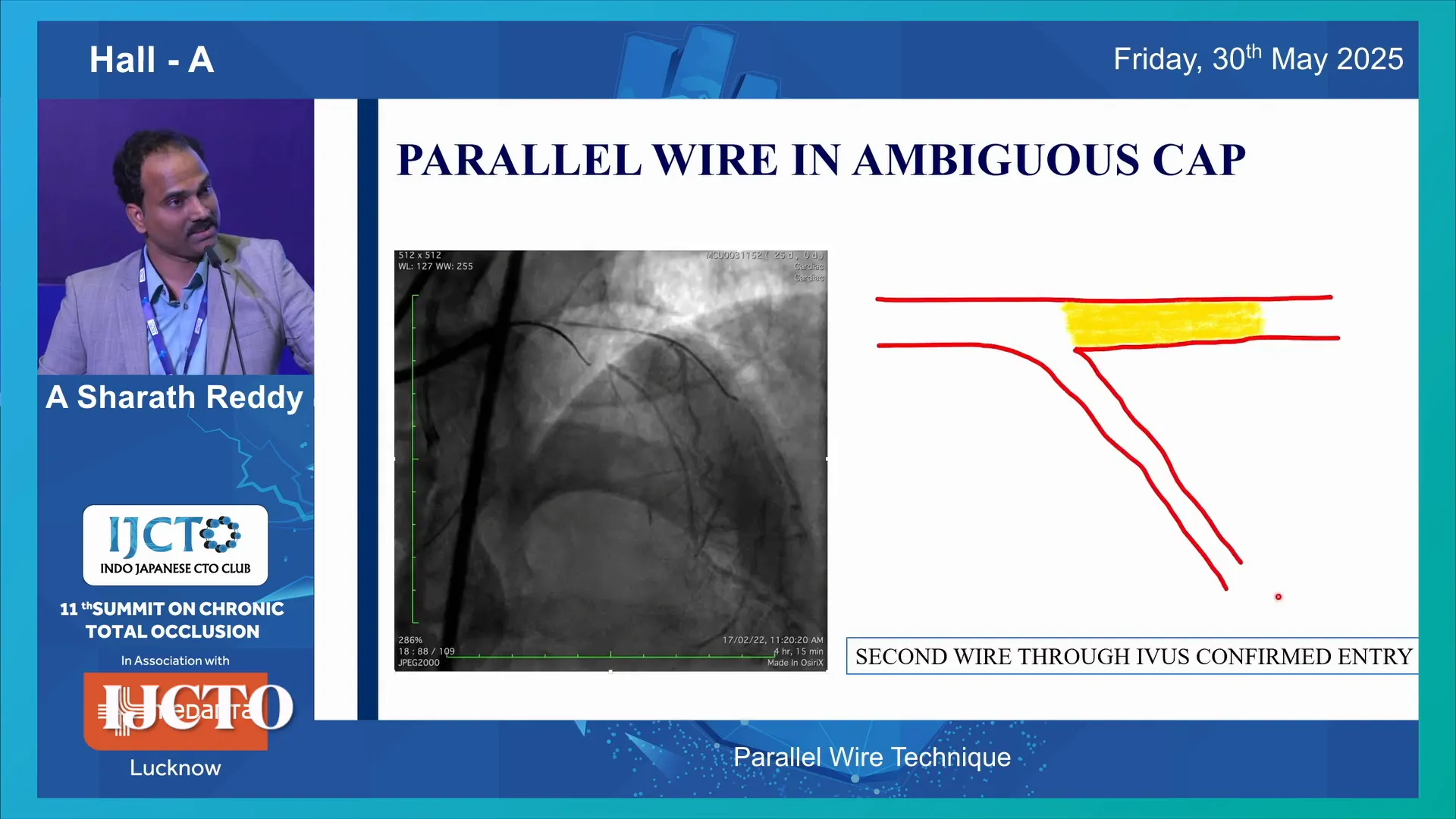
Case 2: Ambiguous Cap Scenario
Another challenging scenario involves an ambiguous occlusion cap. The team performed an intravascular ultrasound (IVUS)-guided cap puncture to confirm central wire entry. However, the wire distal to the cap was subintimal.
To proceed with parallel wiring here, it is crucial that the second wire passes through the same entry point as the first wire. This is ensured by balloon dilatation at the entry site and the use of a double lumen catheter, which extends the over-the-wire lumen beyond the lesion entry.
Once confirmed, the second wire is advanced parallel to the first, guided by the roadmap provided by the initial wire. This strategy improves the chances of successful true lumen entry beyond the subintimal space.
When Parallel Wire Technique Fails
Success with the parallel wire technique is not 100%. There are cases where despite all efforts, the second wire also enters the subintimal space. For example, in a mid left anterior descending (LAD) CTO with an ambiguous cap, after an IVUS-guided puncture, both the first and second wires were subintimal despite attempts lasting nearly 10 minutes.
This situation can cause the distal vessel to become less visible or even invisible on angiography, effectively spoiling the distal lumen and complicating further interventions.
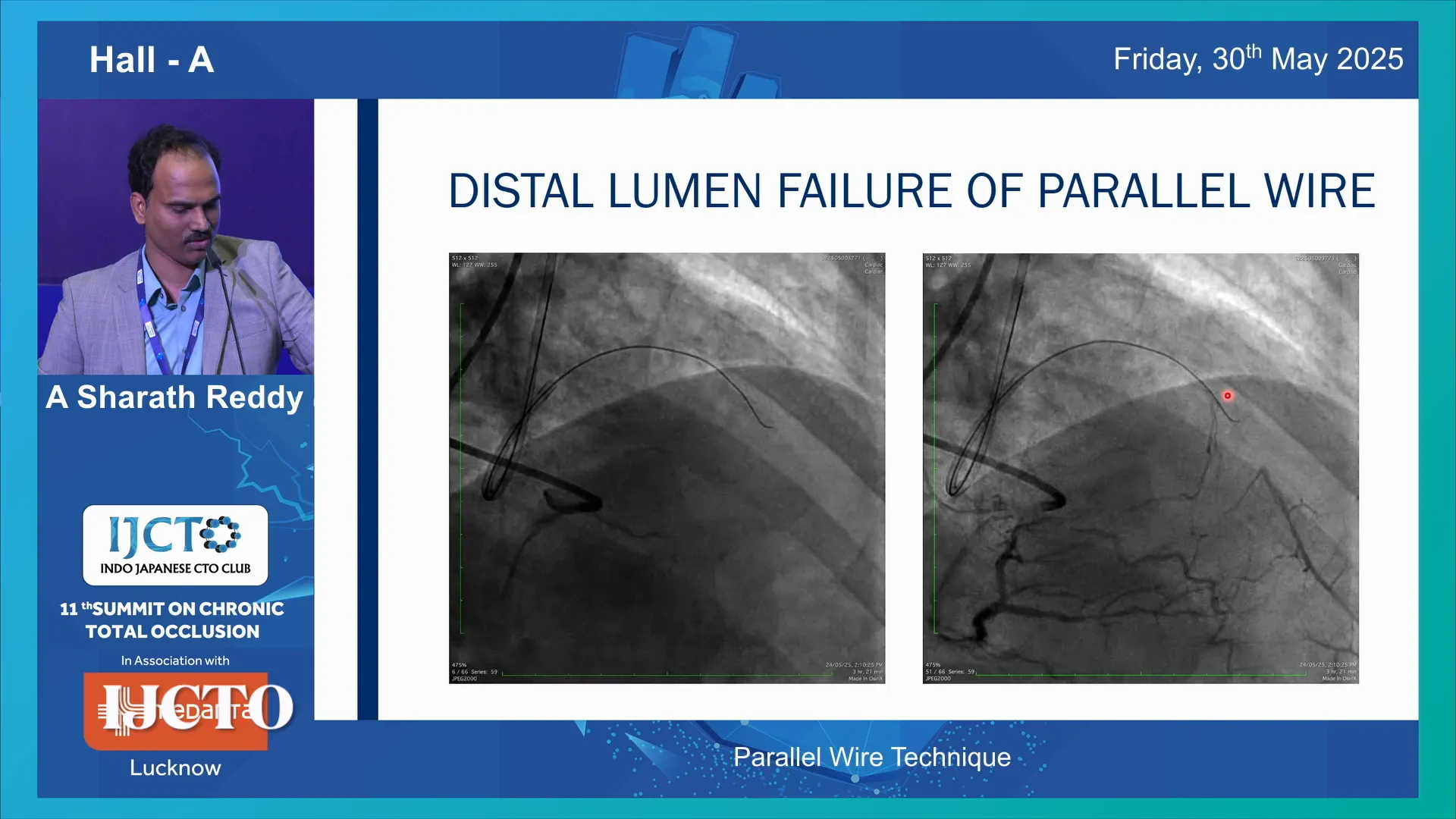
When this occurs, alternative strategies must be employed:
- Switching to a retrograde approach
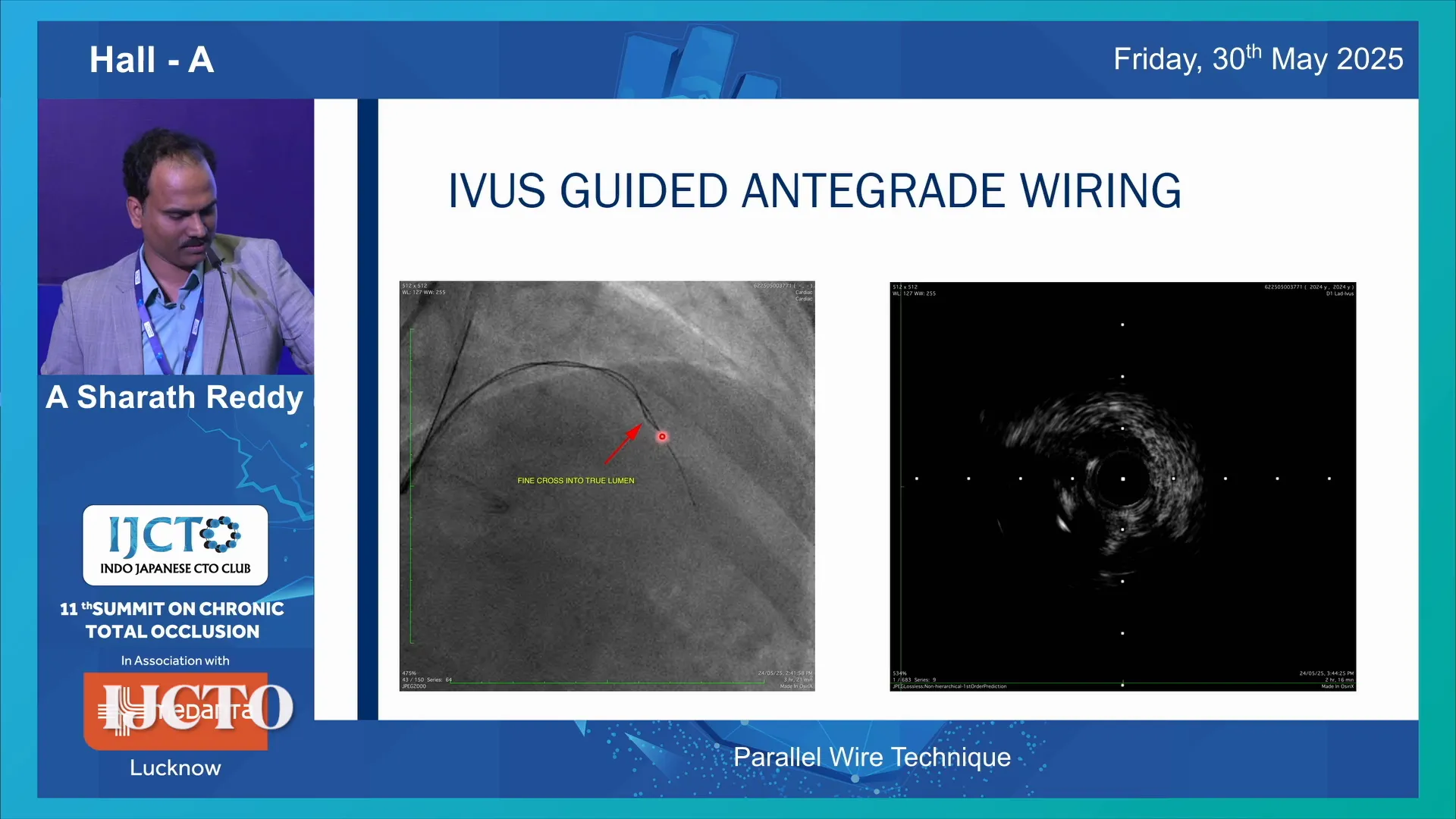
- Using an IVUS catheter to perform guided antegrade wiring
- Tip detection techniques such as Antegrade Dissection and Re-entry (ADR) from the subintimal space
In the case described, an Iris catheter was introduced with a parallel microcatheter and a high-tip-load wire (Harnet wire). This allowed true lumen wiring and subsequent microcatheter advancement, leading to successful completion of the procedure.
Key Takeaways and Best Practices
- The parallel wire technique is a powerful and cost-effective antegrade approach when the first wire is subintimal.
- Clear visualization of the distal vessel on angiography is the most important predictor of success.
- The technique relies on using the first wire as a roadmap, often requiring the use of double lumen or microcatheters to facilitate the second wire.
- Wire selection is critical: escalation to higher tip load, more steerable wires increases success rates.
- The three main techniques—parallel wire, redirecting the first wire, and device-based re-entry—are mutually exclusive due to subintimal space expansion.
- In ambiguous cap cases, IVUS-guided cap puncture and the use of double lumen catheters ensure the second wire follows the same entry path.
- Be prepared to switch strategies if parallel wire attempts fail, including retrograde approaches or IVUS-guided antegrade wiring.
- Continuous angiographic confirmation in two orthogonal views is essential for wire position verification.
Frequently Asked Questions (FAQs)
What is the parallel wire technique in CTO interventions?
The parallel wire technique involves inserting a second guidewire alongside the first when the first wire enters a subintimal space. The first wire acts as a roadmap, helping the second wire navigate towards the true lumen to improve procedural success.
When should I choose the parallel wire technique over other methods?
Parallel wire technique is preferred when the distal vessel is clearly visible on angiography, and the first wire is subintimal. It is a cost-effective antegrade approach with a good success rate compared to device-based re-entry methods.
What types of wires are used in the parallel wire technique?
The second wire usually has a higher tip load and better steerability than the first wire to overcome resistance in the subintimal space. Examples include escalating from Fielder XTR to Gaia 2 or Gaia 3 wires.
What are the risks of the parallel wire technique?
One risk is expansion of the subintimal space, which can make other re-entry techniques less effective. Failed parallel wiring attempts may also reduce distal vessel visibility, complicating further interventions.
How can I confirm the position of the second wire?
Use two orthogonal angiographic views to verify that the second wire is in the true lumen, not subintimal. In ambiguous cap cases, intravascular ultrasound (IVUS) guidance and double lumen catheters help ensure accurate wire placement.
What if parallel wire attempts fail?
If parallel wiring is unsuccessful, alternative strategies include switching to retrograde wiring, IVUS-guided antegrade wiring, or tip detection ADR from the subintimal space.


No Comments