17 Mar Navigating Complexities in Post-CABG RCA CTO: A Live Case Analysis
In this detailed case study, we explore the intricate process of managing a chronic total occlusion (CTO) in a post-CABG patient. With a focus on strategic planning and execution, this live procedure showcases the challenges and decision-making involved in ensuring patient safety and optimizing outcomes.
Table of Contents
Introduction to the Patient’s Condition
The case involves a 66-year-old male patient who presented with non-ST elevation myocardial infarction (NSTEMI) and Q-wave myocardial infarction (QMI), accompanied by severe left ventricular (LV) dysfunction. Upon his initial presentation, the patient’s ejection fraction (EF) was a concerning 30%. His medical history is significant for an old anterior myocardial infarction and coronary artery bypass grafting (CABG) performed in 2005.
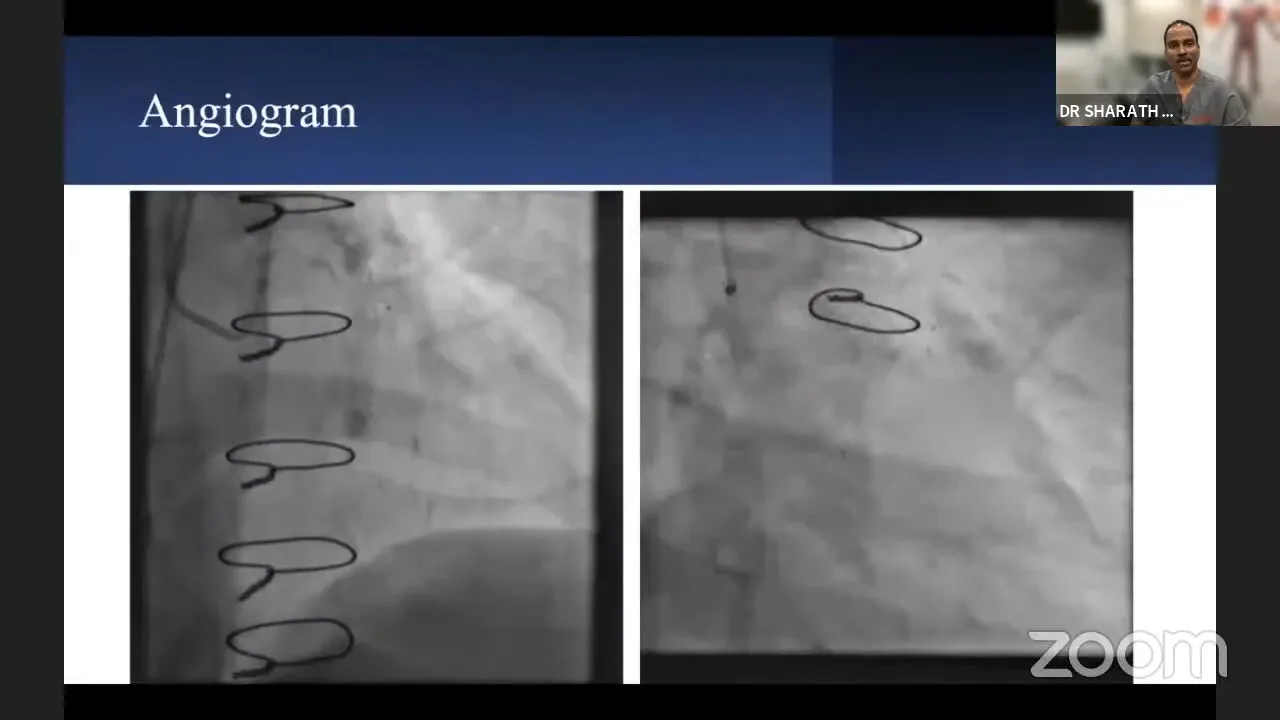
Further investigations revealed triple vessel disease with significant lesions in the saphenous vein grafts (SVG) to the diagonal branches and a chronic total occlusion (CTO) in the right coronary artery (RCA). The RCA was primarily being filled by collaterals from the left anterior descending artery (LAD) and left circumflex artery (LCX). The LAD was receiving blood supply from the left internal mammary artery (LIMA) graft as well as SVGs to the diagonal branches, which were also contributing to the RCA’s perfusion.
Initial Intervention to Address Decompensation
Given the patient’s critical condition and severe LV dysfunction, an immediate intervention was necessary to stabilize him. The strategy was to manage the acute decompensation without resorting to mechanical circulatory support due to financial constraints and mild renal impairment. A percutaneous intervention was performed to stent the diagonal branch, which was crucial as the patient had a tight lesion in the SVG to the diagonal. This lesion was contributing to his acute deterioration.
An intravascular ultrasound (IVUS)-guided stenting of the distal and ostial diagonal was carried out, minimizing contrast usage to protect renal function. Post-procedure, the patient’s LV function showed marked improvement, transitioning from severe to mild-to-moderate dysfunction.

Planning for RCA CTO Procedure
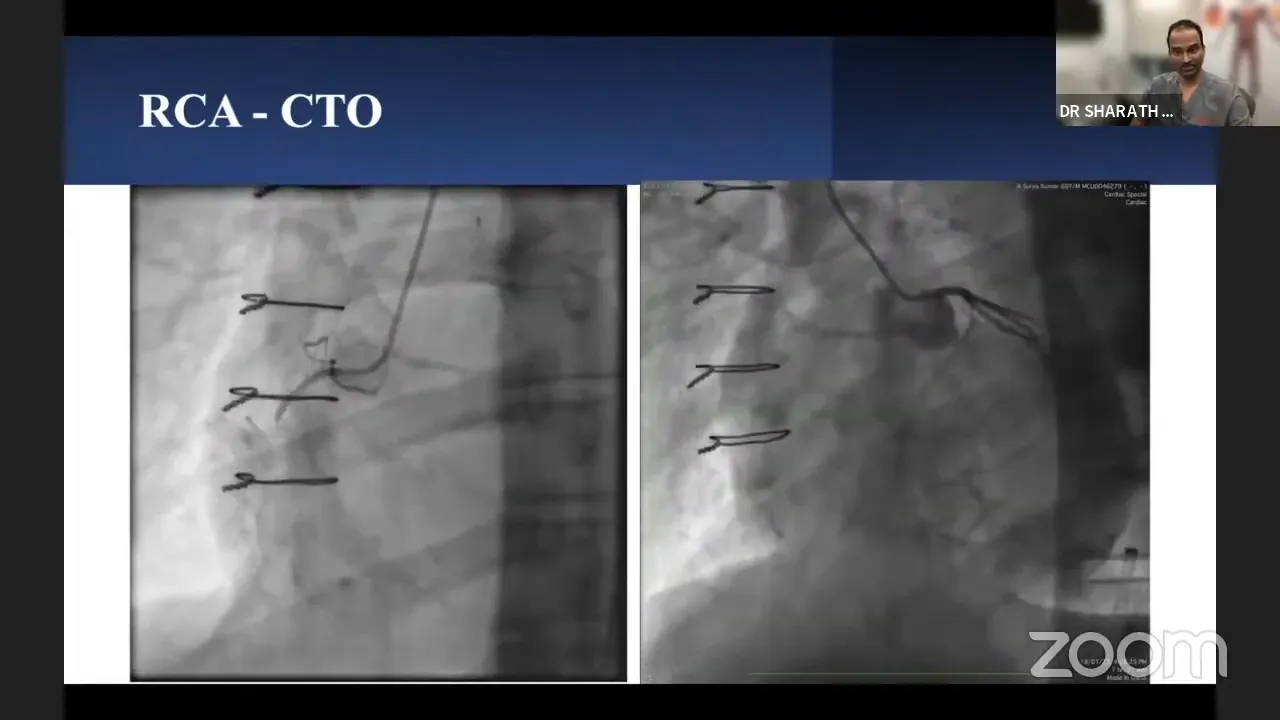
Following the initial stabilization, focus shifted to addressing the RCA CTO. The RCA CTO presented as a long segment occlusion with an ambiguous proximal cap, compounded by retrograde filling only up to the crux. Additionally, the lesion was characterized by calcification and significant angulation, making it a complex case with a high Japanese Chronic Total Occlusion (J-CTO) score.
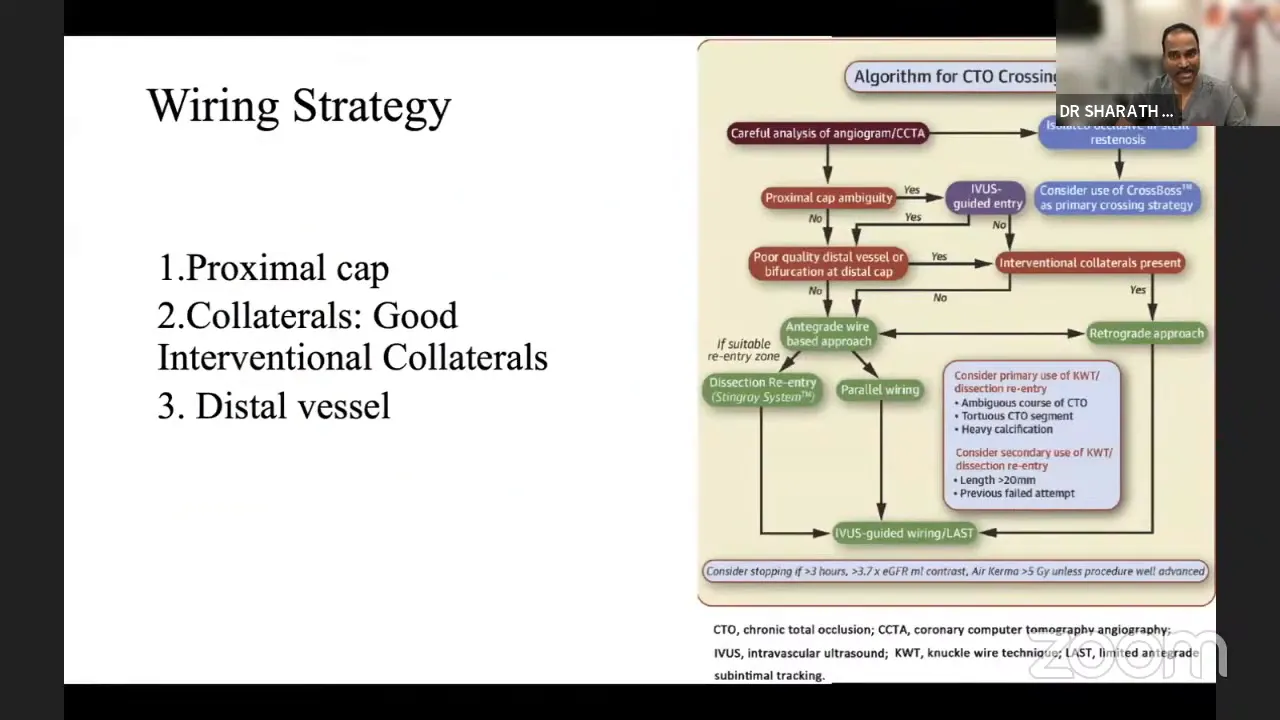
The strategic approach involved a retrograde-first strategy due to the ambiguous cap and long lesion length. The presence of robust septal collaterals originating beyond the LAD CTO provided a feasible retrograde pathway. The plan was to initiate retrograde preparation, followed by antegrade techniques based on the progress and results observed.
Wiring Strategy and Challenges
The wiring strategy was influenced by the lesion’s complexity and the potential for losing side branches during the procedure. The initial plan was to attempt antegrade preparation, but given the limited success rate and the ambiguous nature of the proximal cap, a primary retrograde approach was deemed more suitable. The retrograde approach would allow for better visualization and access, given the limitations of the antegrade route.
Challenges included navigating through the dense calcification and angulated segments of the RCA, requiring precise wire manipulation and selection. The use of a microcatheter system was integral to successfully negotiating these anatomical challenges.
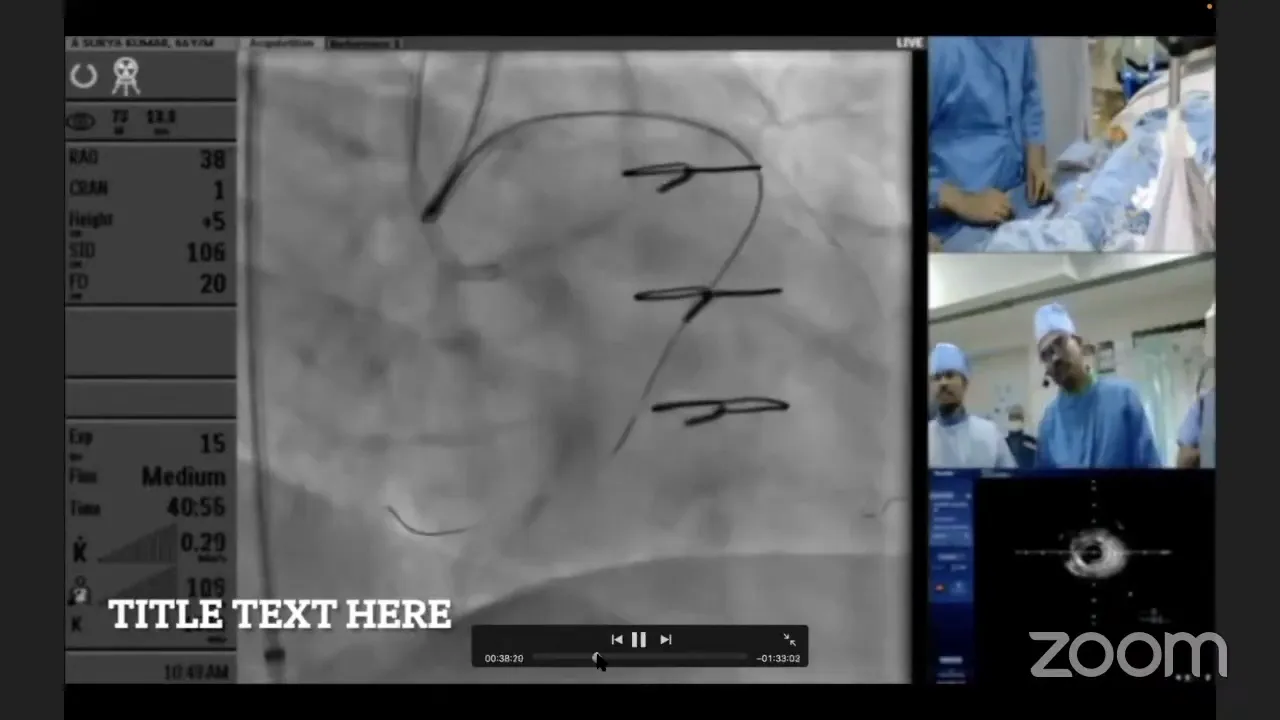
Live Procedure: Part 1 – Initial Attempts
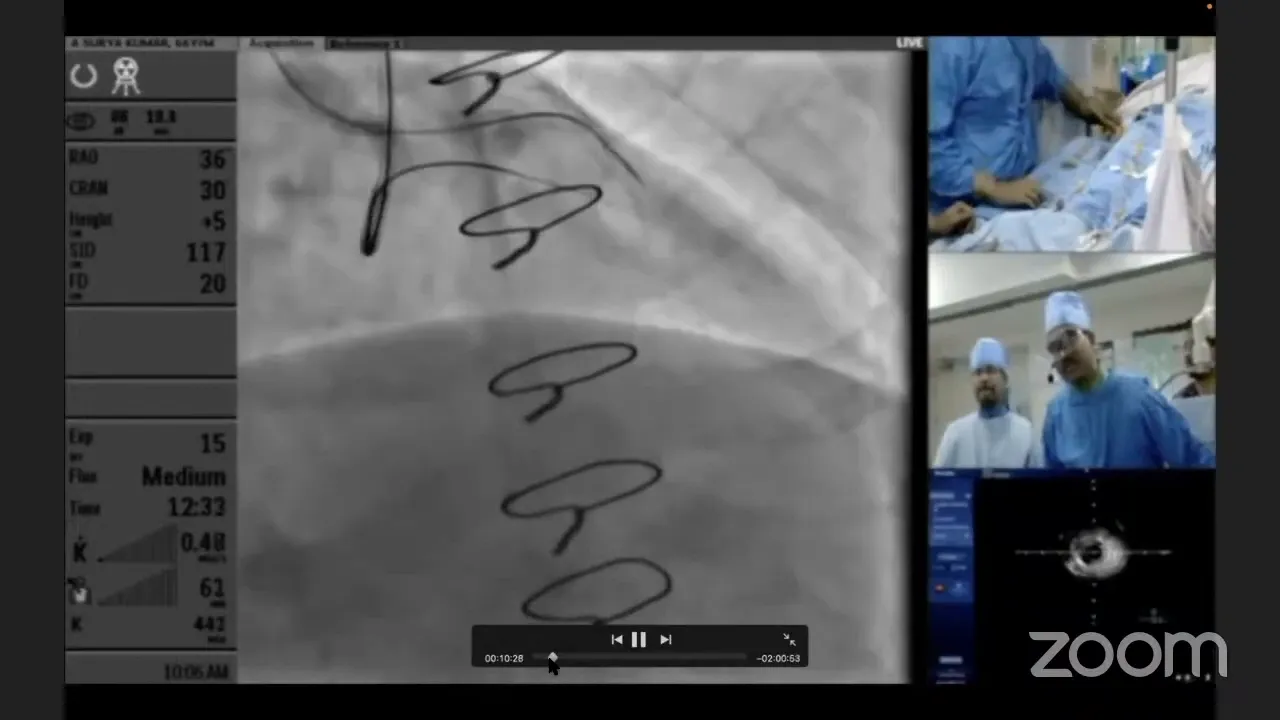
The live procedure commenced with the utilization of dual microcatheters to minimize contrast and enhance visualization. The initial attempts involved an antegrade wiring approach using a Gaia 2 wire, which unfortunately resulted in subintimal tracking at the distal cap. This was attributed to the hardness and calcification at the distal cap, causing the wire to deviate from the intended path.
Despite multiple attempts to redirect the wire, the guide catheter support proved insufficient, and the wire continued to track subintimally. Recognizing the limitations, an escalation to a higher tip load wire, the Hornet, was made. This wire, with its taper tip design, offered greater penetration capabilities, although it initially followed the same subintimal path as the Gaia 2. Adjustments were made to correct the trajectory in orthogonal views, highlighting the importance of multi-angle visualization in complex CTO interventions.
Live Procedure: Part 2 – Escalation and Adjustments
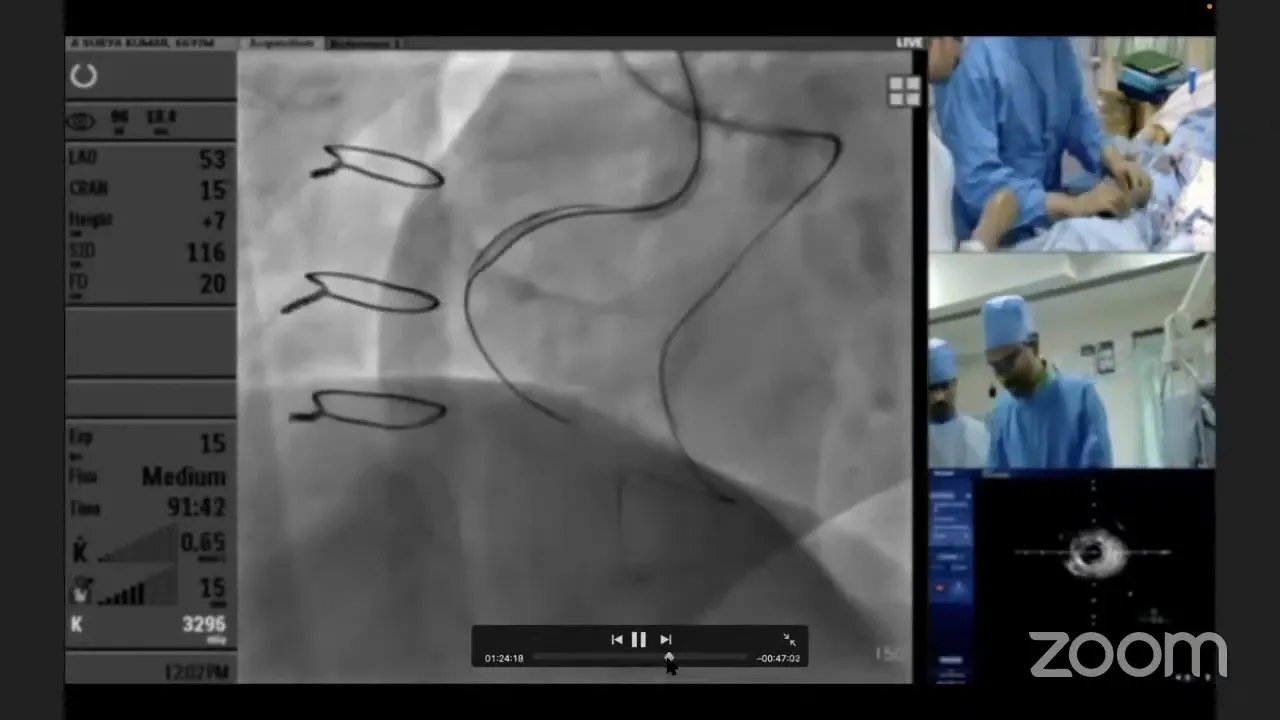
As we moved forward with the procedure, it became evident that navigating the complex RCA occlusion required careful escalation and adjustments. The initial approach with the Gaia 2 wire revealed limitations due to its subintimal tracking. We decided to escalate to a higher tip load wire, the Hornet, which offered enhanced penetration capabilities. However, the wire continued to track subintimally, prompting further adjustments.
To enhance support, we introduced a Corsair microcatheter but encountered catheter fatigue. This necessitated a switch to another microcatheter system, which provided the necessary support to cross the lesion successfully. The use of a sequential double-inflation technique with small balloons, ranging from 1.25 mm to 2.0 mm, was instrumental in creating space for wire advancement. This strategic escalation allowed us to navigate the challenging anatomical features of the RCA CTO.
Transitioning to Investment Procedure
Despite the progress, the complexity of the case led us to consider transitioning to an investment procedure. This decision was influenced by several factors, including the extensive length of the CTO, operator fatigue, and the patient’s stability post-graftoplasty. The investment procedure involved creating a subintimal space across the CTO segment, extending beyond the distal cap.
By dilating with a 2 mm balloon, we aimed to create potential microchannels or fenestrations that could facilitate future interventions. This approach, while not guaranteeing immediate success, was a strategic move to set the stage for a more straightforward antegrade re-entry in subsequent procedures.
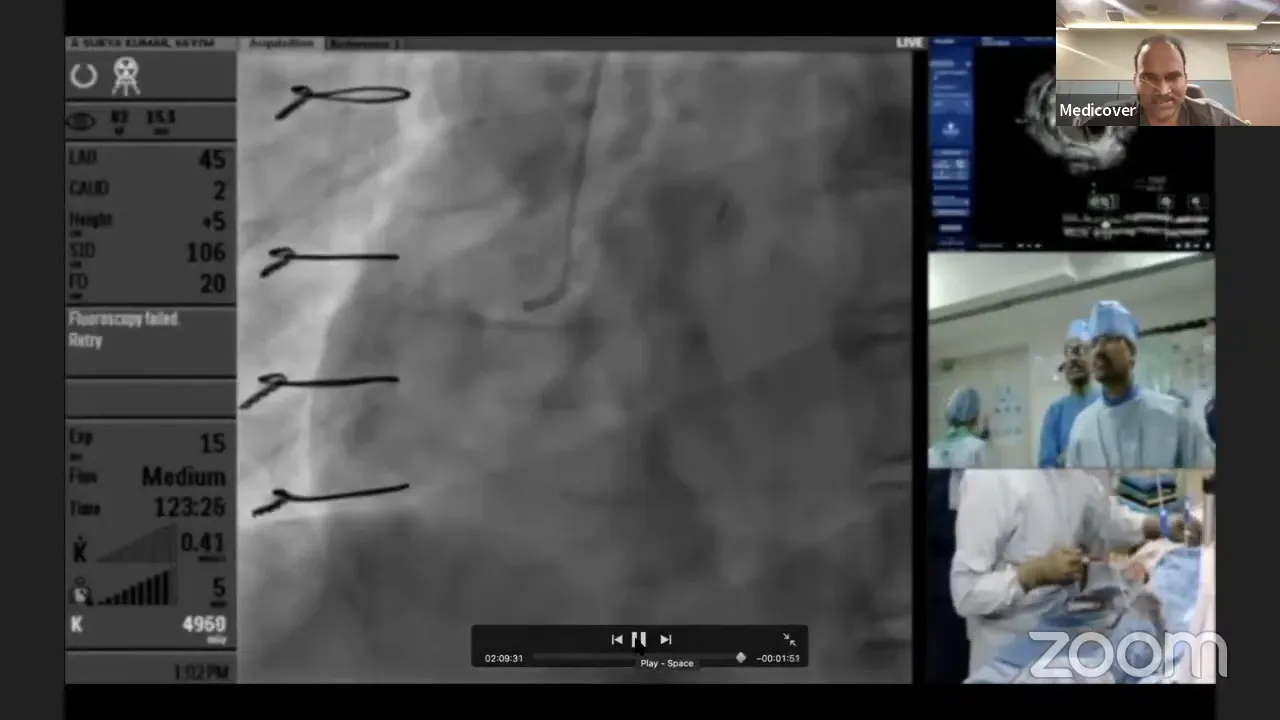
Final Steps and Considerations
As the procedure progressed, we revisited the decision regarding stenting the LAD. Given the importance of maintaining an open LAD for potential retrograde access, we opted to stent the vessel. This action served as a comprehensive investment for future interventions, ensuring that both antegrade and retrograde routes remained viable.
The procedure concluded with careful post-dilation and checks to confirm the stent’s position and function. The final angiographic results showed improved flow and collateralization in the RCA, setting a positive foundation for the next session.

Discussion on Safety and Future Procedures
Safety remains paramount in complex interventions like this RCA CTO case. Throughout the procedure, we took measures to minimize radiation exposure and preserve the patient’s stability. These considerations are critical, especially in lengthy procedures where both patient and operator fatigue can pose risks.
For future procedures, the investment approach enhances the likelihood of successful re-entry, reducing the need for extensive retrograde interventions. However, it’s essential to remain adaptable, ready to adjust strategies based on real-time findings and patient response.
FAQs
- Why was an investment procedure chosen? The investment procedure was selected due to the complexity and length of the CTO, operator fatigue, and the need to set up a successful future intervention.
- What are the benefits of subintimal dilation? Subintimal dilation creates potential microchannels that can facilitate easier re-entry in subsequent procedures, improving the likelihood of success.
- How is patient safety maintained during such complex procedures? Safety is prioritized by minimizing radiation exposure, ensuring stable patient hemodynamics, and making strategic decisions to avoid excessive procedural length.
- What are the next steps after an investment procedure? The next steps involve allowing time for the formation of microchannels and planning a follow-up procedure to attempt re-entry, with both antegrade and retrograde options available.



No Comments