09 Jan Navigating Ambiguous Cap in Mid LAD CTO: A Comprehensive Case Study
In this detailed lecture, Dr. Sharath Annam discusses a challenging case involving an ambiguous cap in a mid LAD CTO. This blog will explore the strategies, techniques, and insights shared during the lecture to provide a deeper understanding of this complex interventional cardiology scenario.
Table of Contents
- Introduction to the Case
- Patient Background and Initial Findings
- Dual Angiography Overview
- Understanding the Proximal Cap
- Wiring Strategy for Ambiguous Cap
- Techniques for Successful Cap Puncture
- Navigating Retrograde Access
- Confirming the Distal Cap
- Principles of Reverse Cut Technique
- Finalizing the Intervention
- Final Angiographic Results
- Key Learnings and Takeaways
- FAQ
Introduction to the Case
The case under discussion involves a 74-year-old male patient with a chronic total occlusion (CTO) in the mid left anterior descending (LAD) artery. The complexity of this case is heightened by the presence of an ambiguous proximal cap, which presents significant challenges in achieving successful revascularization.
This patient had previously undergone a primary percutaneous coronary intervention (PCI) to the right coronary artery for an acute ST-elevation myocardial infarction (STEMI). During that procedure, the CTO in the LAD was identified and scheduled for elective intervention. The patient’s heart rhythm was normal, and left ventricular function was preserved, making him a suitable candidate for further intervention.
Patient Background and Initial Findings
Our patient, a 74-year-old male, had a medical history marked by a primary PCI to the right coronary artery, performed for an acute STEMI. During the angiogram, a CTO in the LAD was discovered, necessitating a planned intervention.
Initial dual angiography revealed a mid-LAD CTO following the first diagonal branch. Three branches were identified at the occlusion site, complicating the cap’s interpretation. A stent was visible in the right coronary artery, extending from the ostium.
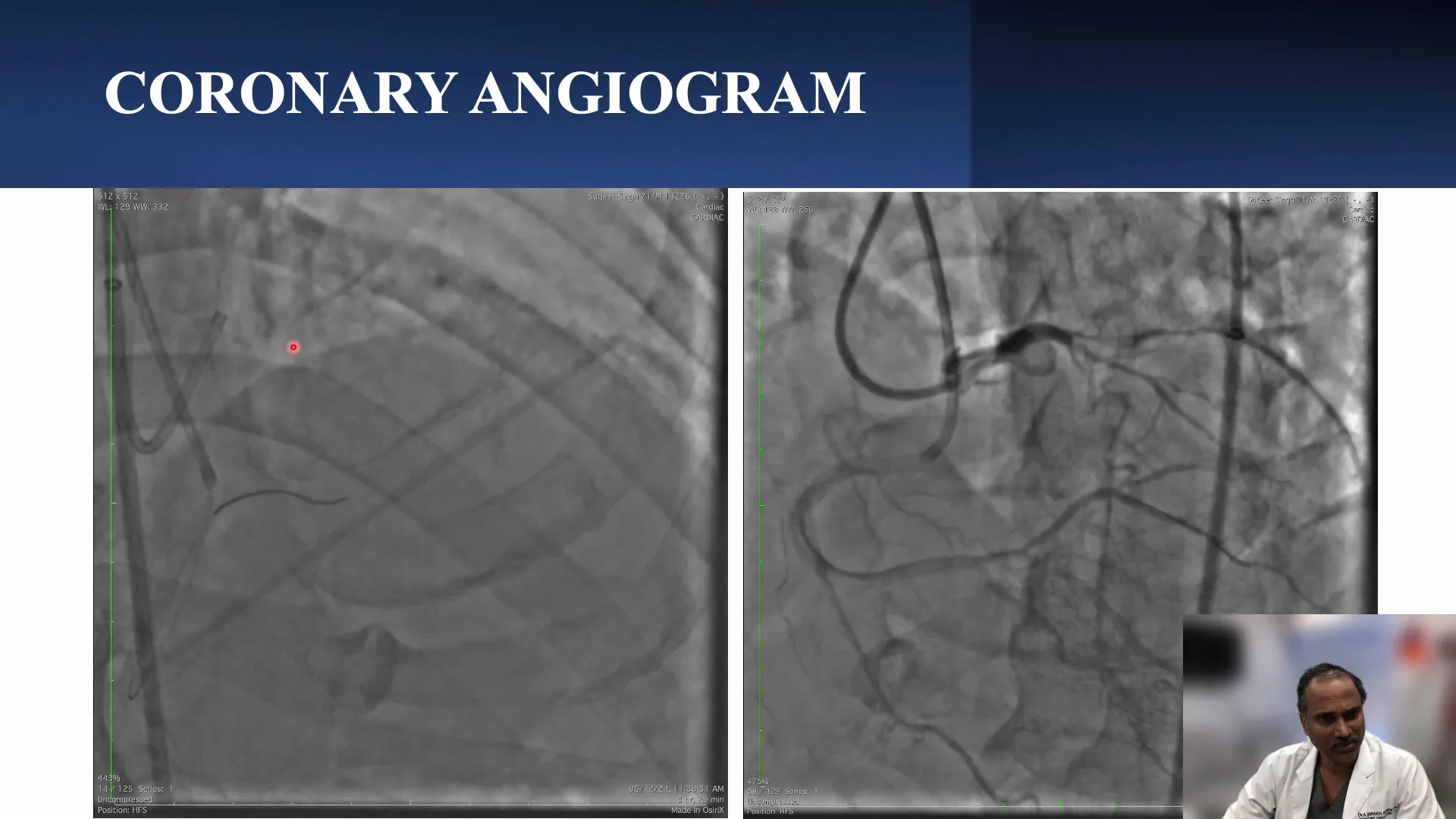
Dual Angiography Overview
Dual angiography is pivotal in assessing the CTO, particularly when dealing with an ambiguous cap. In this case, it was performed to delineate the anatomy and identify the branches arising at the occlusion site. This imaging technique aids in visualizing the LAD’s course and understanding the complex branching, which is crucial for planning the intervention strategy.
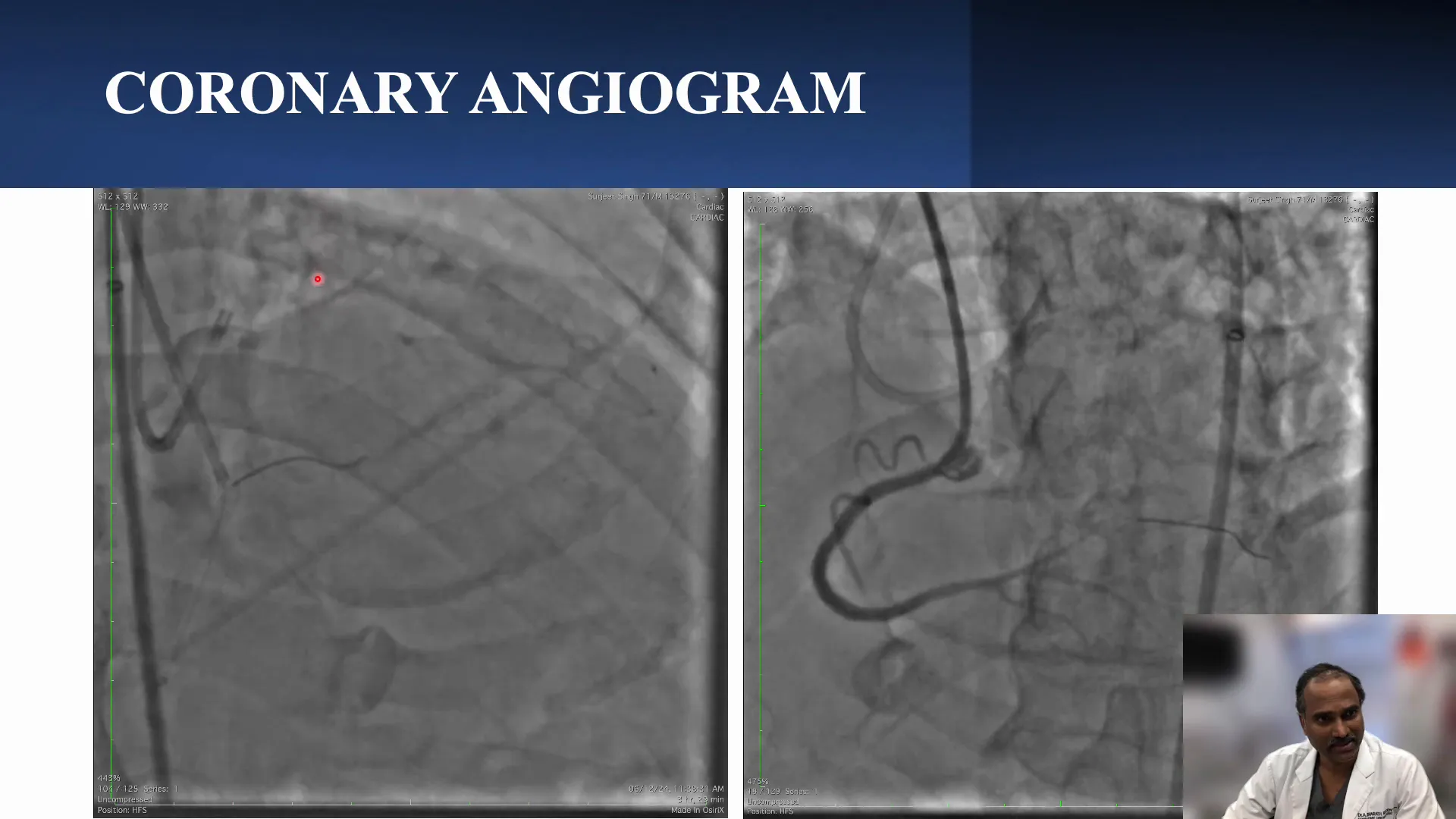
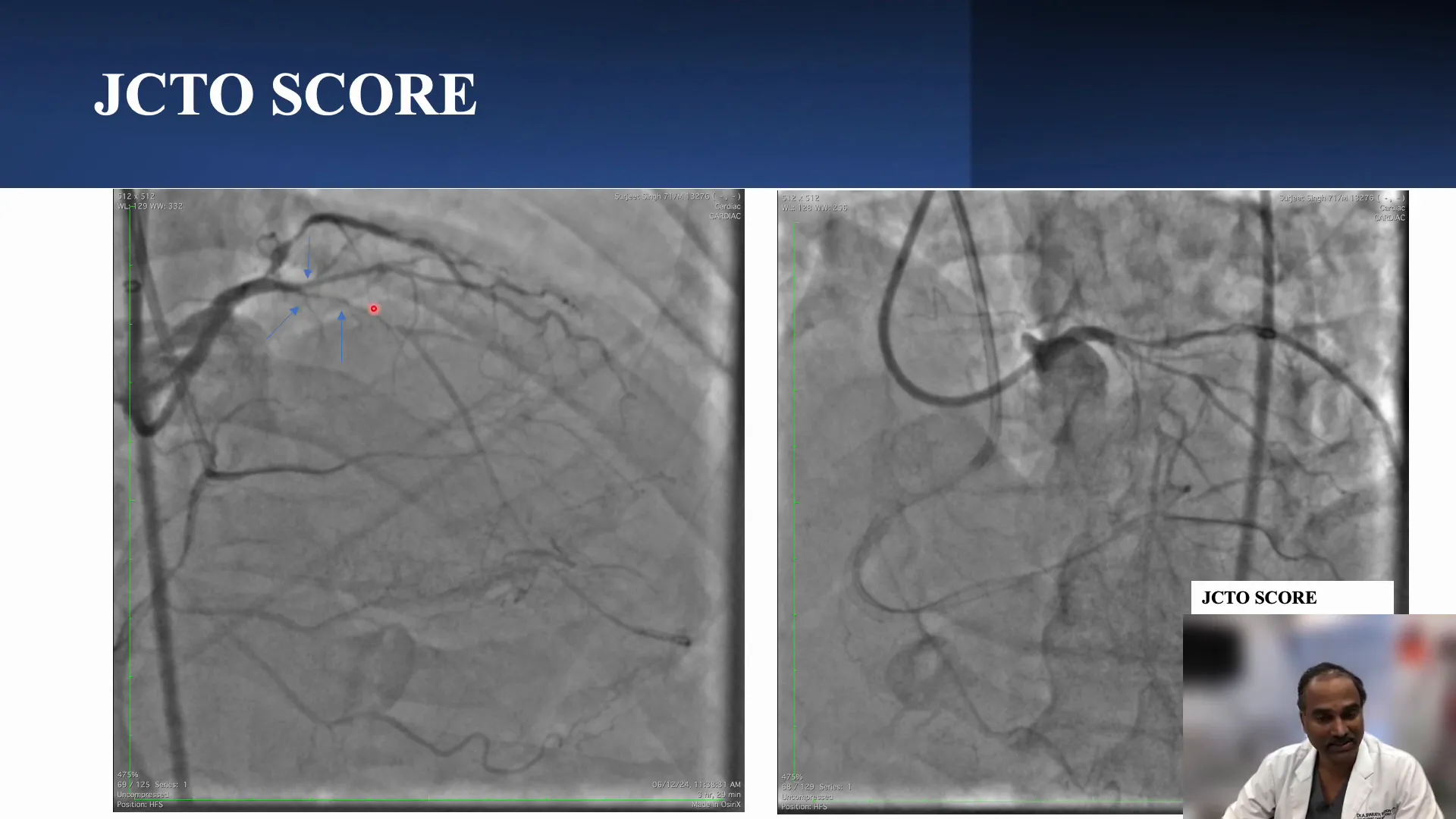
Understanding the Proximal Cap
The proximal cap in this scenario is ambiguous due to multiple side branches, including a diagonal, a septal, and another branch that could be either septal or part of the LAD. This complexity makes imaging and targeting the cap challenging, with the length estimated to be more than 20 mm and a bend of less than 45 degrees.
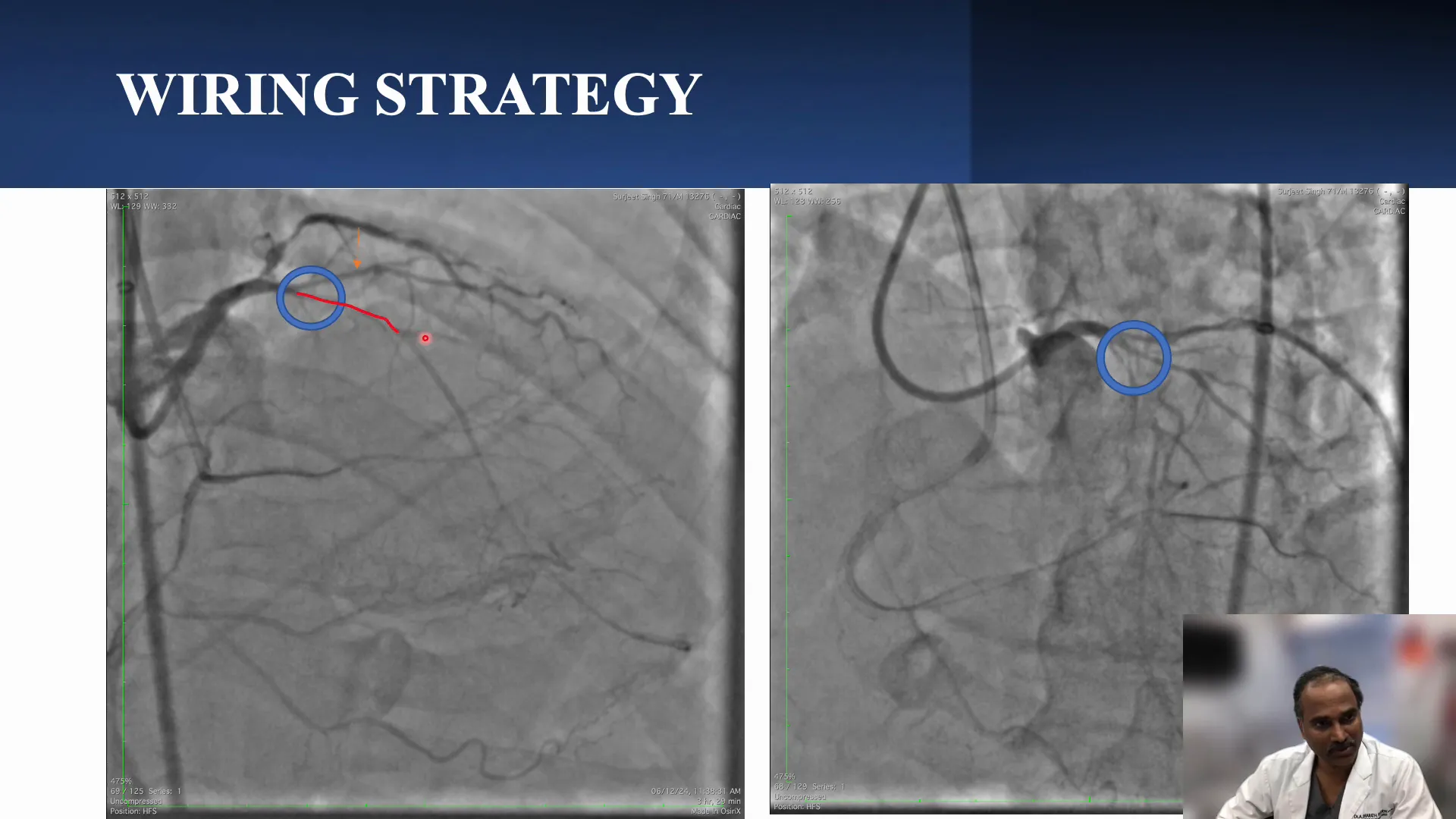
Wiring Strategy for Ambiguous Cap
Addressing the ambiguous cap begins with an intravascular ultrasound (IVUS)-guided cap puncture. Among the branches, the diagonal is deemed the most suitable for this procedure due to its size. Smaller septal branches may not accommodate the IVUS catheter effectively.
Once the cap is punctured, the wiring strategy involves advancing the wire while considering the visibility of the distal vessel, which is essential for guiding the wire accurately. The wire should ideally enter the distal LAD proximal to the second diagonal (D2).
Techniques for Successful Cap Puncture
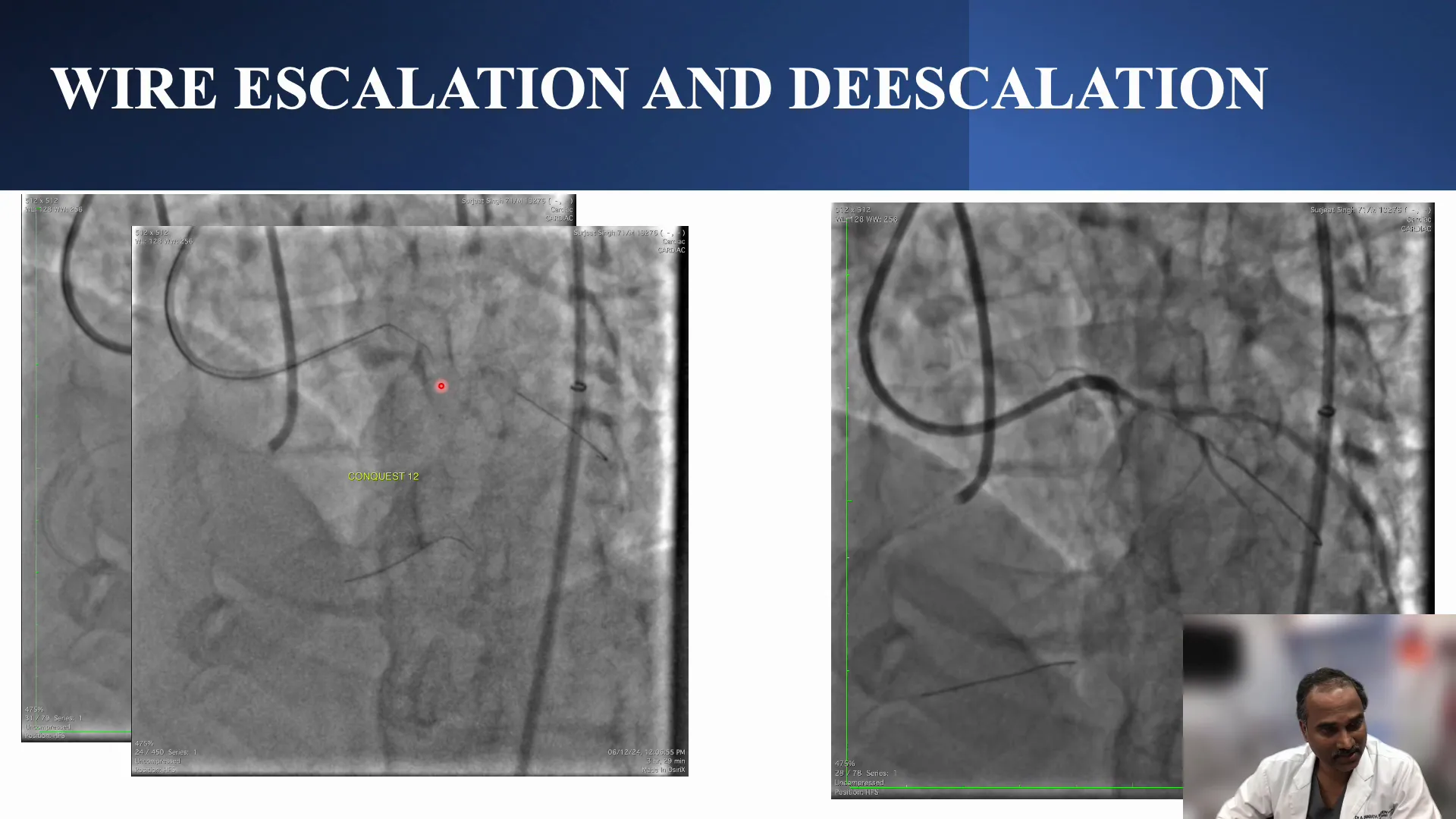
In this case, the initial attempt at cap puncture using a Gaia 2 wire was unsuccessful due to insufficient angulation penetration. Switching to a Conquest Pro wire didn’t yield better results, leading to contrast extravasation, indicating potential perforation. This necessitated reevaluation of the proximal cap or consideration of a retrograde approach.
Navigating Retrograde Access
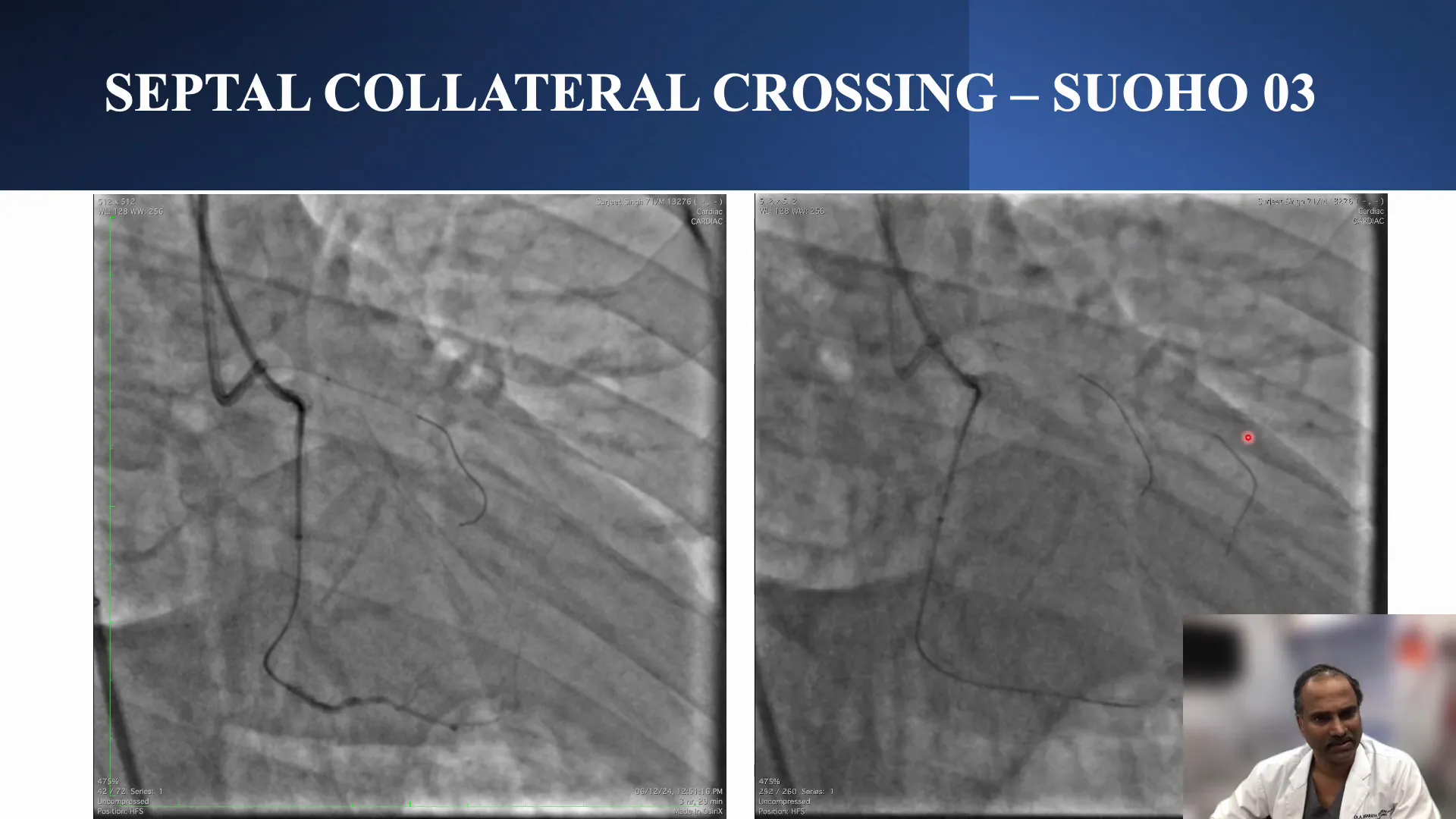
When the antegrade approach failed, a retrograde strategy was employed via a suitable septal collateral. Retrograde wiring demands precision, especially when navigating past stents in the aorto-ostial region of the retrograde vessel. Proper guide extension provides additional support and ensures the wire travels centrally through the stent, facilitating smoother progression.
Upon successfully navigating the septal collateral, a Corsair Pro catheter was used, but it couldn’t advance due to stiffness. Switching to a Finecross catheter allowed crossing into the LAD, confirming the distal cap’s clarity and enabling retrograde wire escalation.
Confirming the Distal Cap
Confirming the distal cap is a crucial step in managing a CTO with an ambiguous proximal cap. In this case, the retrograde approach allowed for clear visualization of the distal cap, ensuring no ambiguity remained.
Once the Corsair Pro crossed the septal collateral, the distal cap was confirmed to be clear. This clarity was essential before proceeding with the retrograde wire escalation and the subsequent intervention steps.
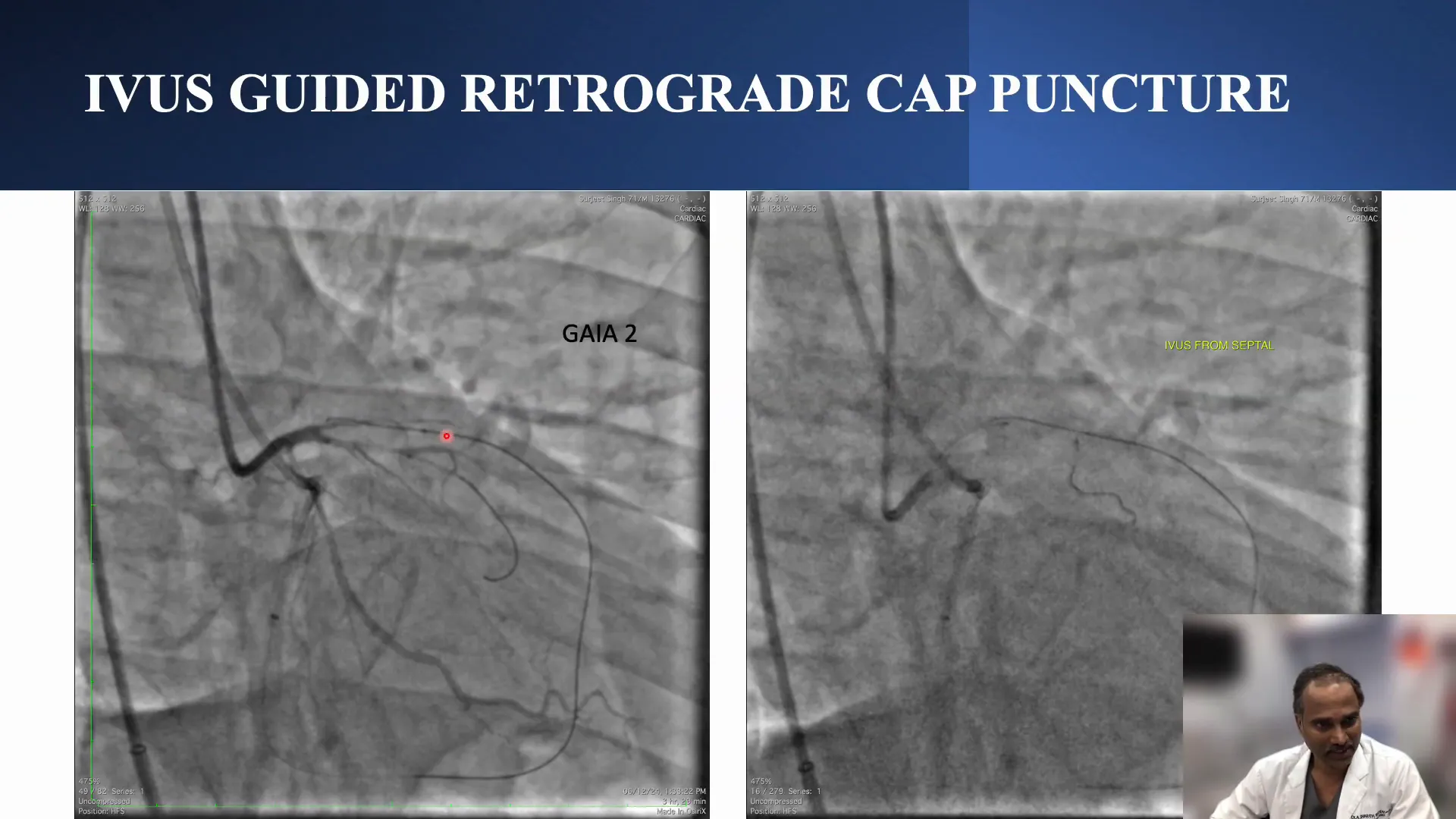
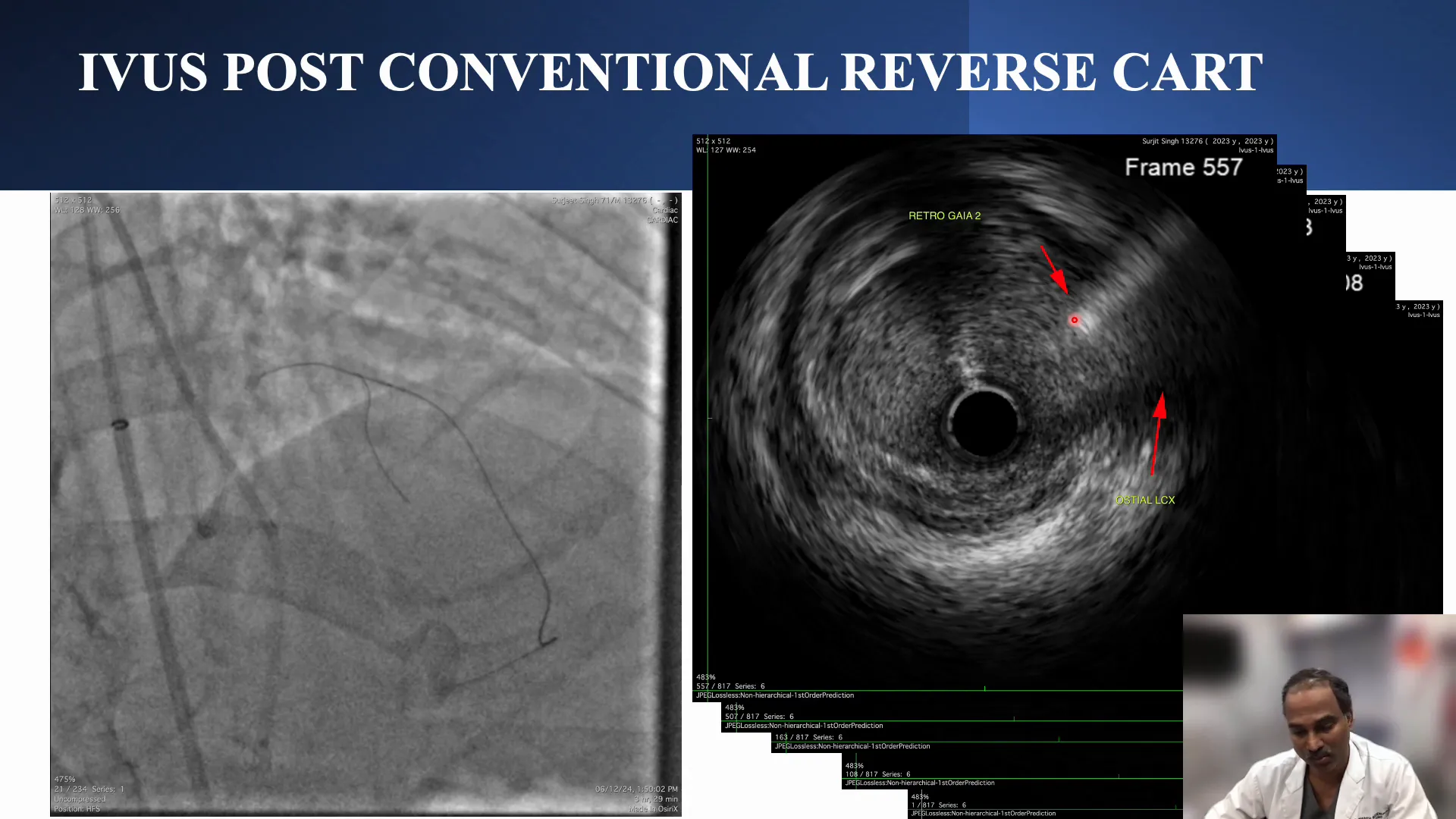
Principles of Reverse Cut Technique
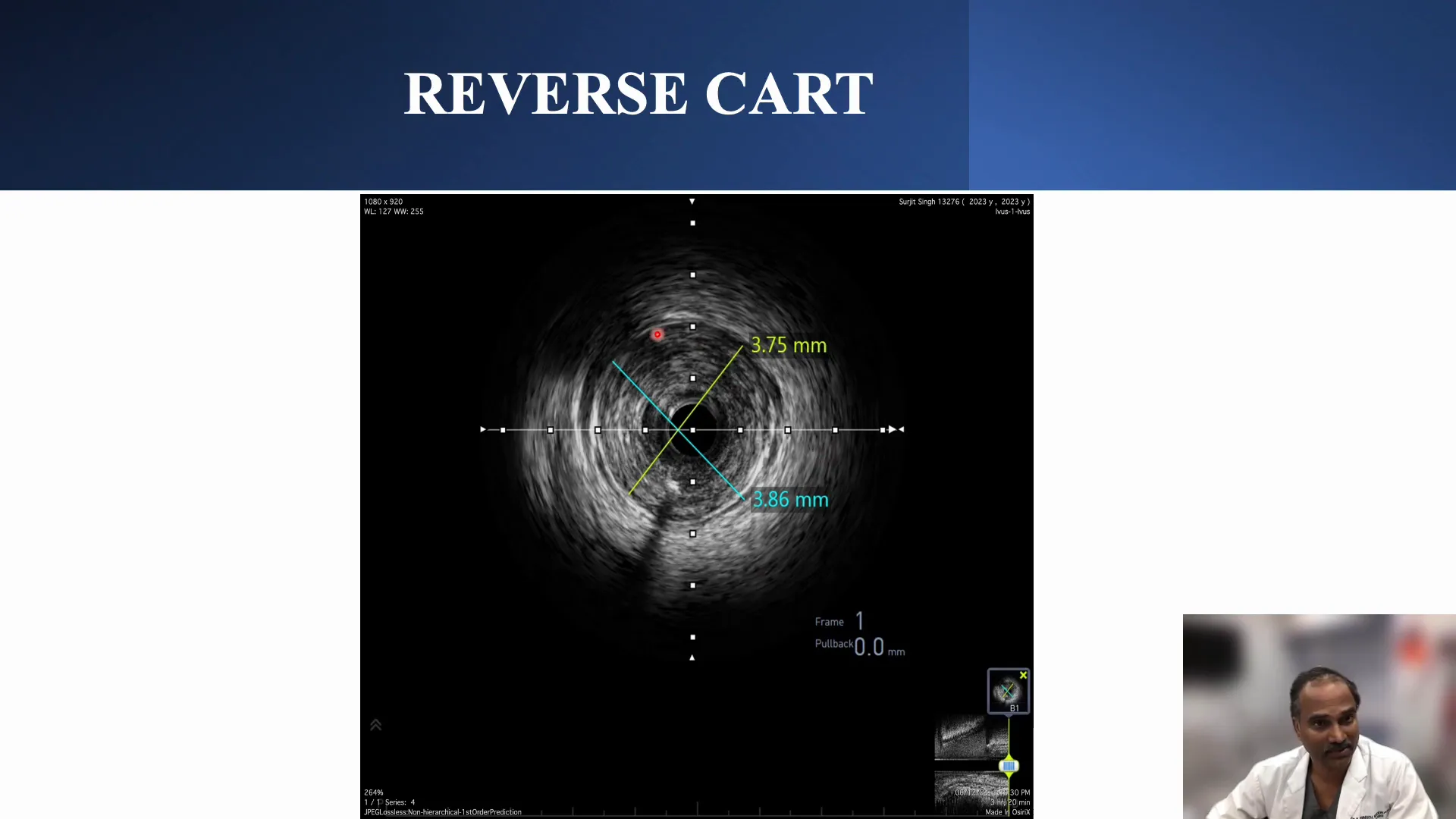
The reverse cut technique was employed to minimize the risk of losing side branches, particularly the D1, during the procedure. The key principle here is to perform the reverse cut beyond the diagonal branch, ensuring the preservation of side branches.
A 3mm balloon was used for the reverse cut beyond the supposed proximal cap. The retrograde wire, Gaia 2, was directed towards the end of the balloon, ensuring the wire remained in the true lumen and away from the proximal cap.
Finalizing the Intervention
After confirming wire placement in the true lumen, the intervention progressed with externalization avoided due to the presence of a stent at the aorto-ostial region. A tip-in technique was used for quick antegrade access, ensuring safety and efficiency.
Intravascular ultrasound (IVUS) was used to verify wire location in relation to side branches, confirming that the wire was in the true lumen throughout the vessel. This verification was critical before proceeding with stenting.
Final Angiographic Results
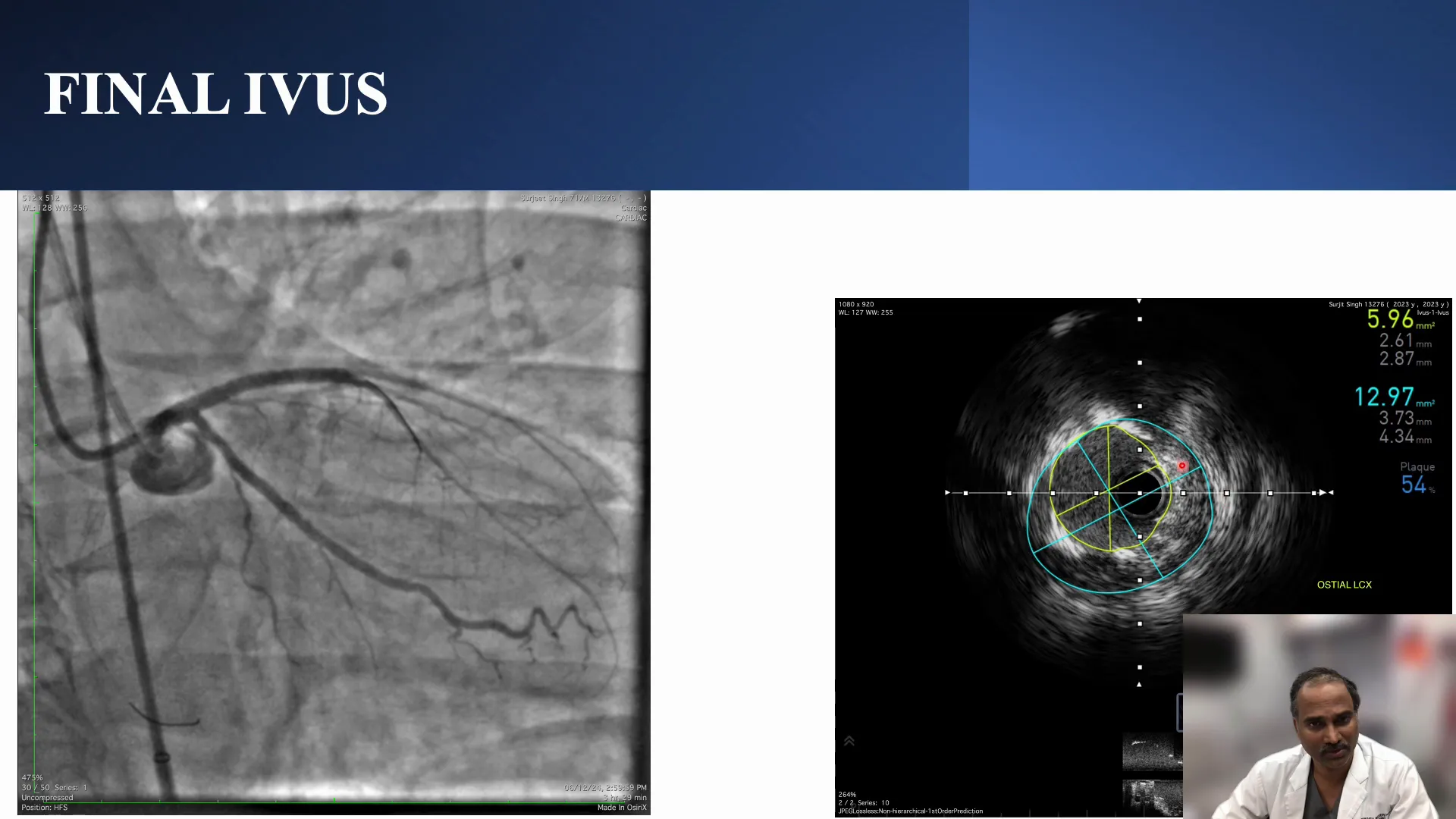
The final angiogram revealed well-expanded vessels with both diagonal branches preserved. The stenting strategy involved a two-stent technique, addressing the diseased LCX and ensuring optimal flow through the LED.
The angiographic results showed good lumen areas, with the LCX ostium measuring approximately 5.9 mm², the LED at 8.7 mm², and the LMCA nearly 13 mm². These measurements indicated a successful intervention with excellent vessel patency.
Key Learnings and Takeaways
- Ambiguous caps with multiple side branches complicate the intervention strategy, requiring careful planning and execution.
- IVUS-guided cap puncture remains essential for addressing ambiguous caps and confirming wire positioning.
- The reverse cut technique is instrumental in preserving side branches, particularly in complex CTO cases.
- Avoiding externalization in the presence of ostial stents is crucial to prevent complications.
- Comprehensive imaging and careful strategy adjustments are key to successful outcomes in complex CTO interventions.
FAQ
What is an ambiguous cap in CTO?
An ambiguous cap refers to a scenario in CTO where the proximal cap’s delineation is unclear due to the presence of multiple branching vessels, making it challenging to identify the appropriate entry point for intervention.
Why is the reverse cut technique important?
The reverse cut technique is crucial as it helps preserve side branches during CTO interventions, especially when dealing with ambiguous caps. It ensures that the main vessel remains open while maintaining flow through critical side branches.
When should externalization be avoided?
Externalization should be avoided when there is a stent at the aorto-ostial region of the retrograde vessel, as it may lead to complications. In such cases, alternative strategies like tip-in techniques are preferred.


No Comments