19 Oct Mastering the Reverse Wire Technique in CTO PCI: A Comprehensive Guide
In this detailed lecture, Dr. Sharath Reddy explores the reverse wire technique for accessing side branches during chronic total occlusion (CTO) percutaneous coronary intervention (PCI). This blog will break down the key concepts, challenges, and procedural steps involved in this advanced technique, providing valuable insights for interventional cardiologists.
Table of Contents
- Introduction to the Case
- Understanding the Angiogram
- Challenges in CTO PCI
- Selecting the Appropriate Side Branch
- Assessing the Diagonal Branch
- Dual Injection Technique
- Wire Positioning and Adjustments
- Identifying the Diagonal Osteum Flap
- Executing the Reverse Wire Technique
- Post-Procedure Analysis and Stenting
- Conclusion and Key Takeaways
- Frequently Asked Questions
Introduction to the Case
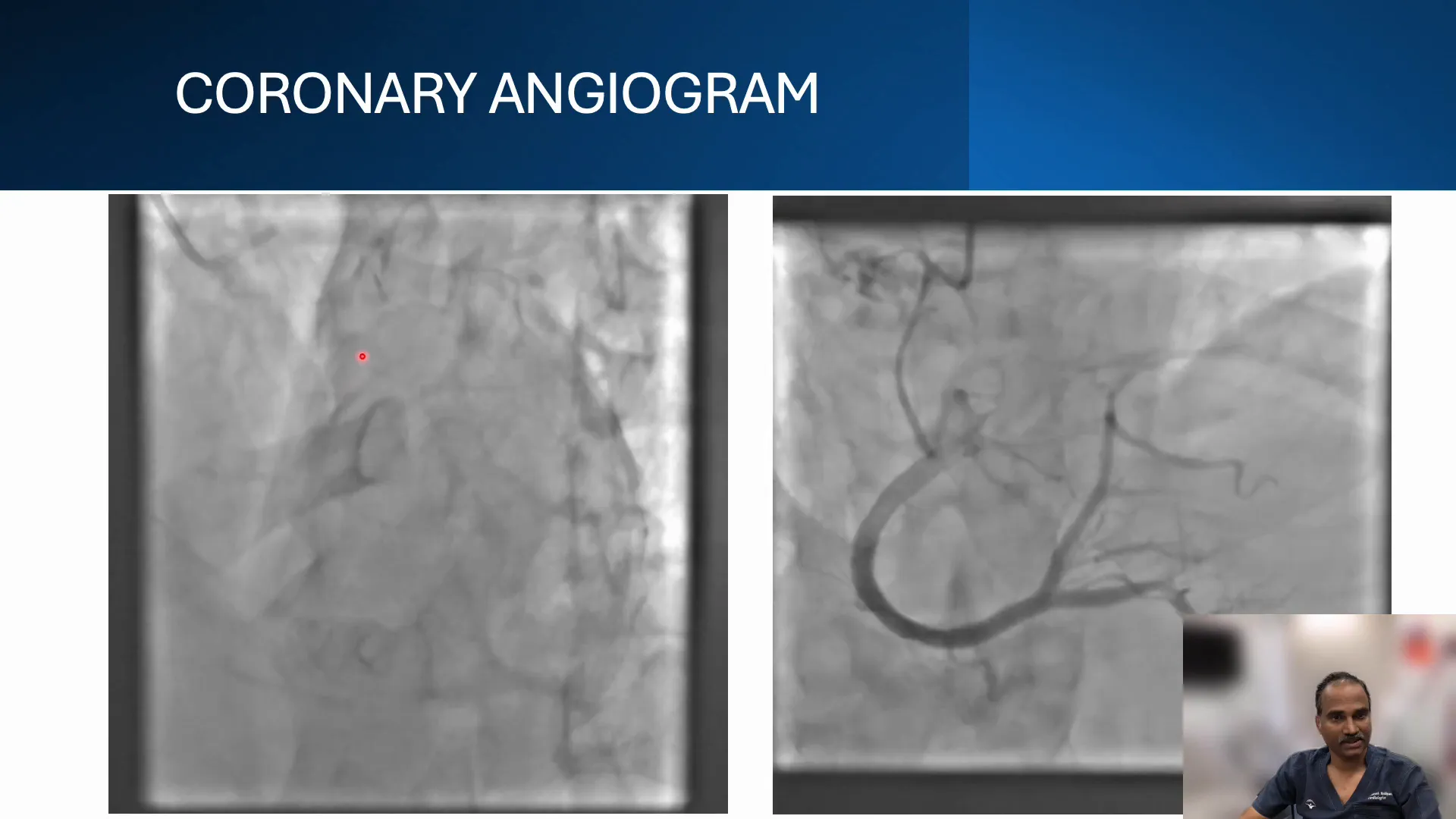
In this segment, we delve into the complexities of a chronic total occlusion (CTO) case involving a 64-year-old male patient. Despite having chronic stable angina and good left ventricular (LV) function, the patient presented with a complete occlusion in the mid-LAD as revealed by the angiogram.
The angiogram depicted a total occlusion at the mid-segment of the LAD, with a couple of branches emerging from the proximal cap. The ambiguity of the proximal cap posed significant challenges, necessitating a meticulous approach to the procedure.
Understanding the Angiogram
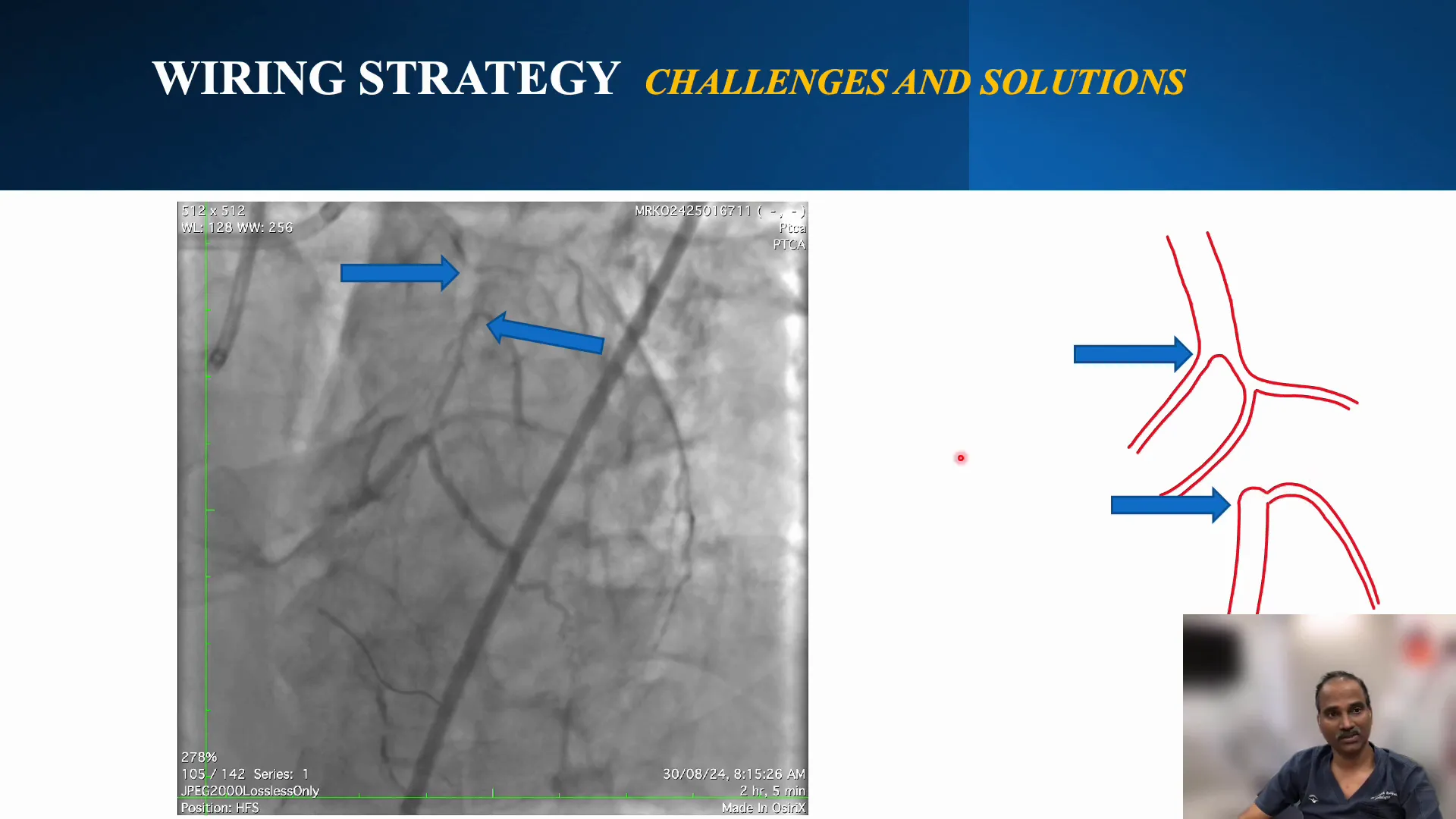
The coronary angiogram plays a crucial role in assessing the anatomy and planning the intervention. In this case, the angiogram revealed a bifurcation at the distal cap with a prominent diagonal branch.
Using retrograde injection, the length of the CTO was estimated to be around 20 mm. The ambiguous nature of the proximal cap and the presence of side branches required careful consideration in planning the procedure.
Challenges in CTO PCI
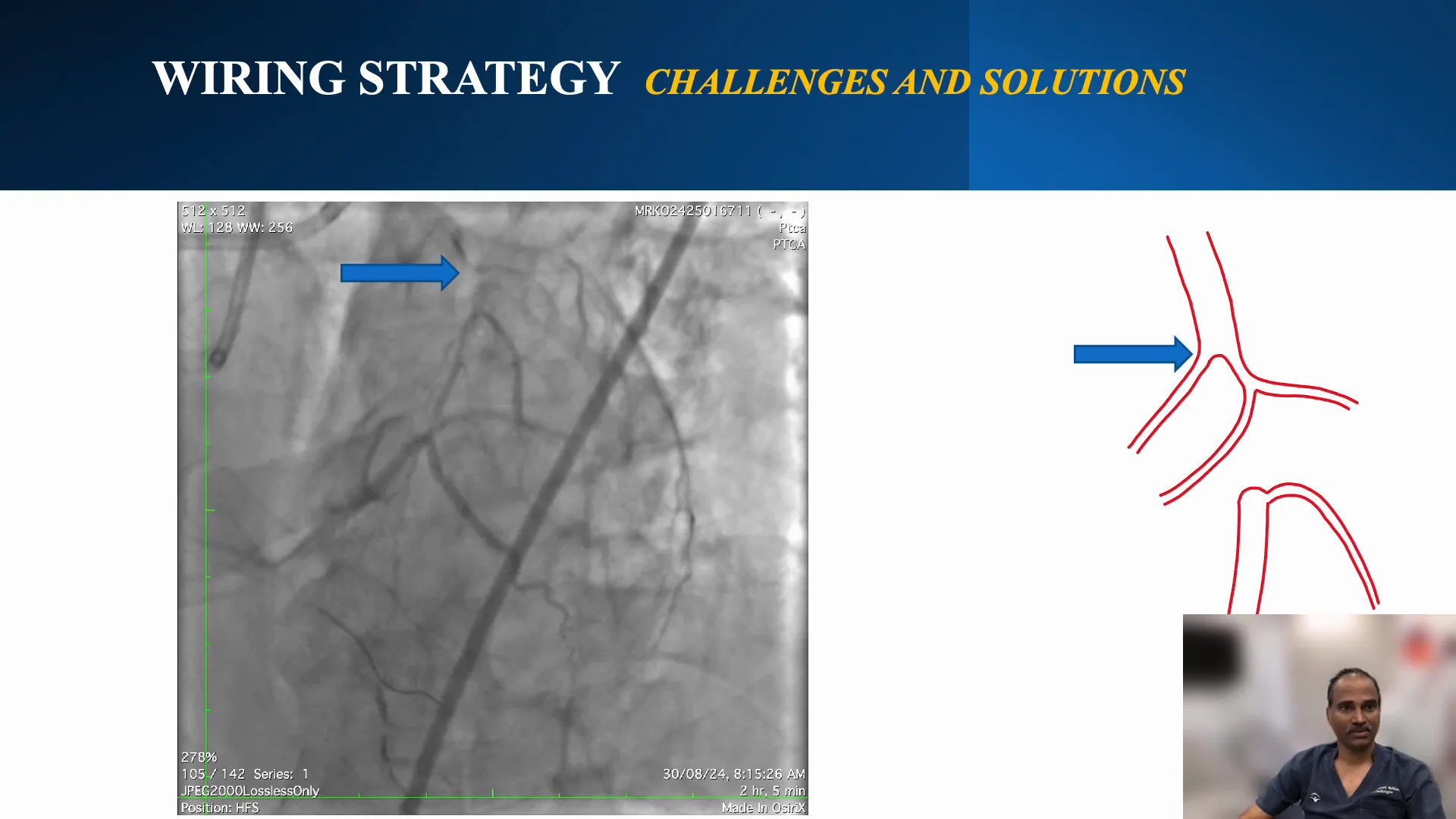
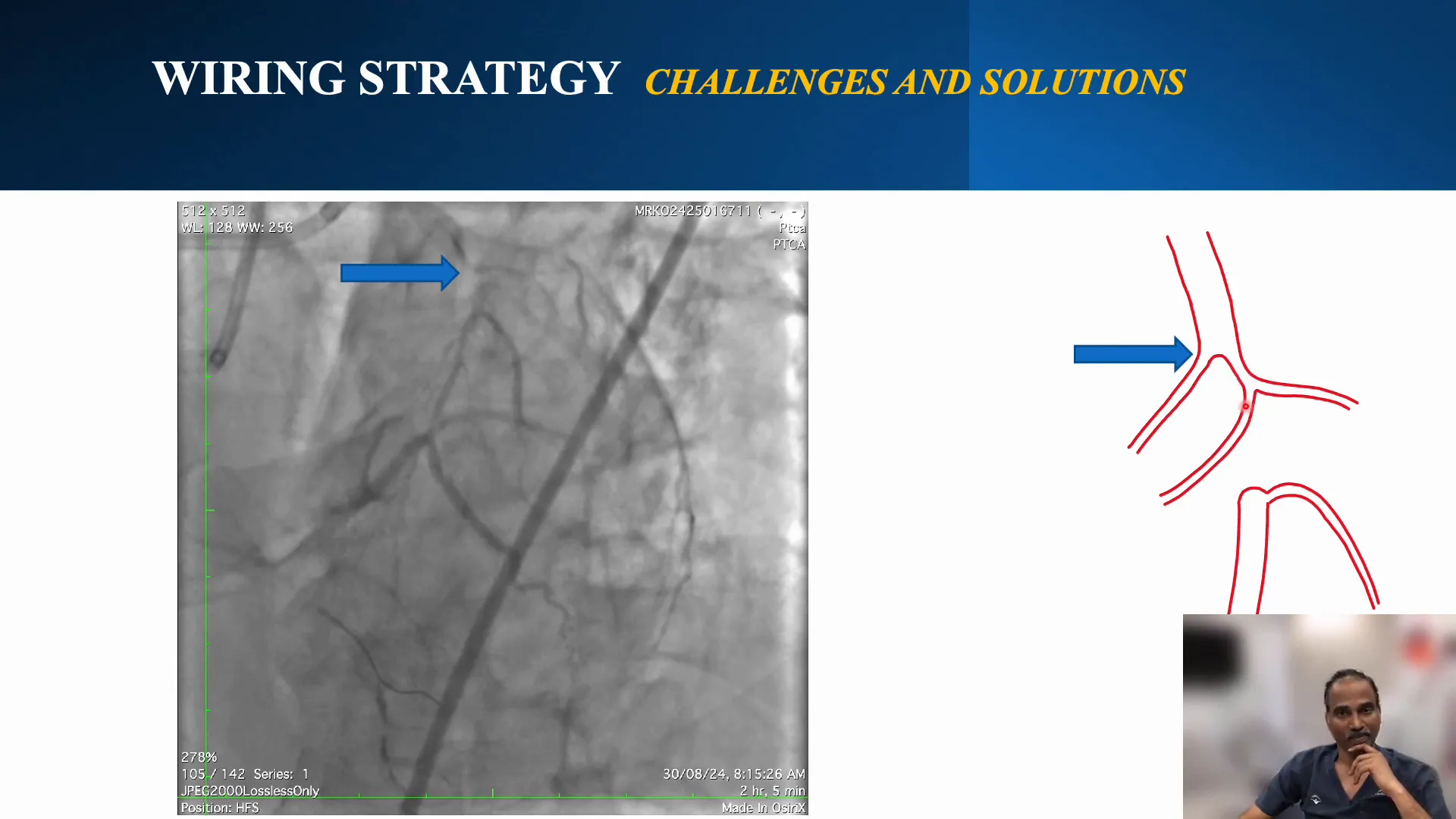
CTO percutaneous coronary intervention (PCI) presents unique challenges, particularly when dealing with ambiguous caps and side branches. In this case, the proximal cap’s ambiguity and the diagonal branch’s angle made the procedure complex.
The J-CTO score was low due to the relatively short length of the occlusion, but the ambiguous cap and the presence of side branches added layers of difficulty to the procedure.
Selecting the Appropriate Side Branch
Choosing the right side branch for imaging and intervention is critical in CTO PCI. In this case, the branch closer to the vessel being imaged was preferred for intravascular ultrasound (IVUS)-guided cap puncture.
This selection was based on the branch’s proximity to the vessel and its suitability for the Boston Opticross IVUS device, which was used to navigate the procedure.
Assessing the Diagonal Branch
The diagonal branch posed a significant challenge due to its cranial angle and the risk of compromising it during the procedure. The branch’s origin and angle were carefully evaluated to plan the intervention strategy.
Predilation with a small balloon was performed to assess the branch and ensure it remained patent during the procedure, thus minimizing the risk of compromising the diagonal branch.
Dual Injection Technique
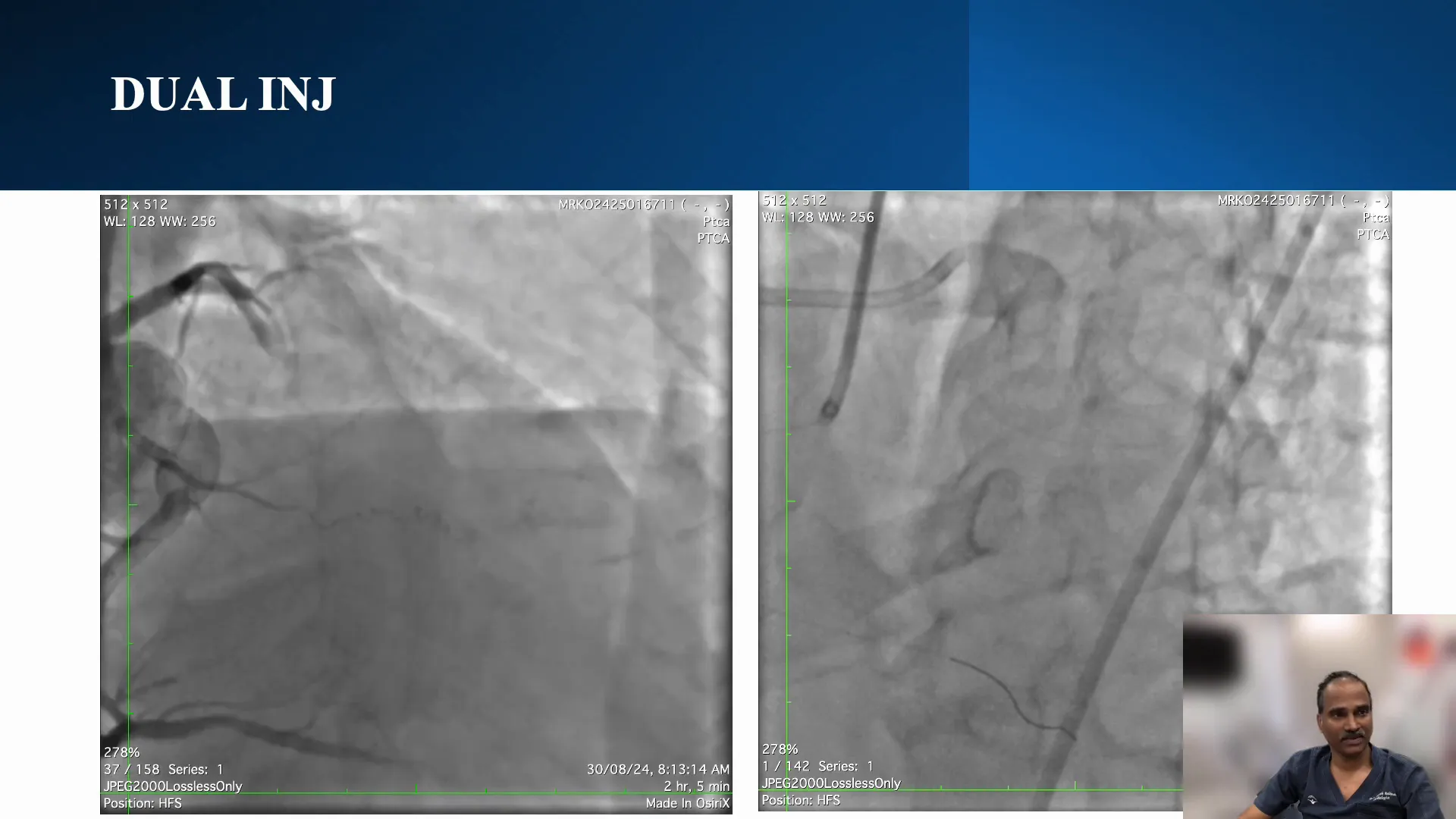
The dual injection technique was employed to provide a comprehensive view of the coronary anatomy. This approach helped clarify the anatomy of the CTO segment, distinguishing between overlapping branches and the occluded segment.
This technique was crucial in confirming the wire’s position and ensuring it was correctly placed in the distal cap, thus preventing the loss of the diagonal branch during the procedure.
Wire Positioning and Adjustments
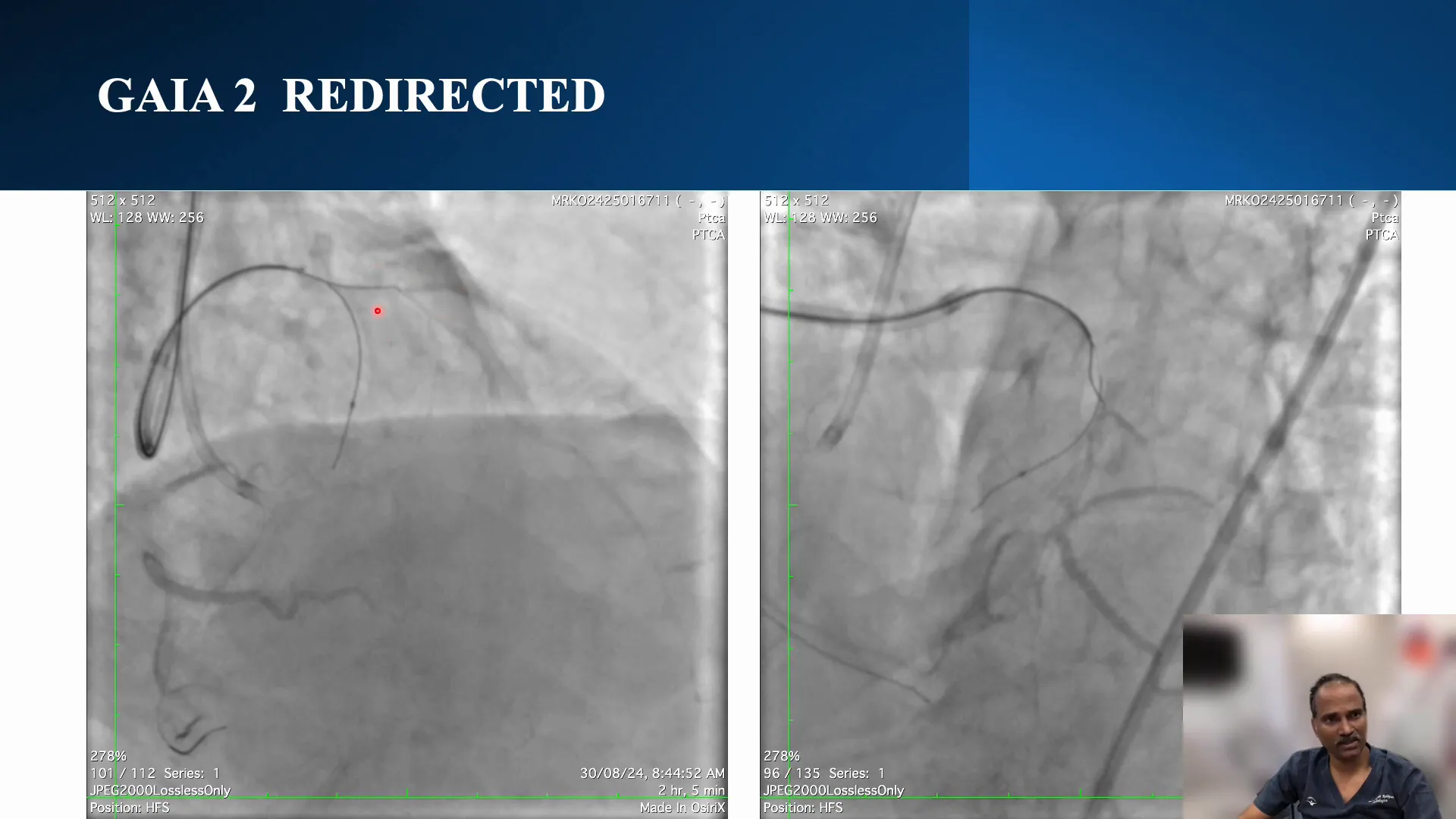
Ensuring accurate wire positioning is crucial in CTO PCI to avoid complications such as losing critical side branches. In this procedure, the initial wire position was assessed using intravascular ultrasound (IVUS). The wire was found to be suboptimal as it was positioned medially to the distal cap, risking the loss of the diagonal branch.
To correct this, the wire was redirected towards the distal cap. This adjustment was confirmed in orthogonal views, ensuring the wire’s optimal placement right on the top of the distal cap, thus preserving the diagonal branch’s integrity.
Identifying the Diagonal Osteum Flap
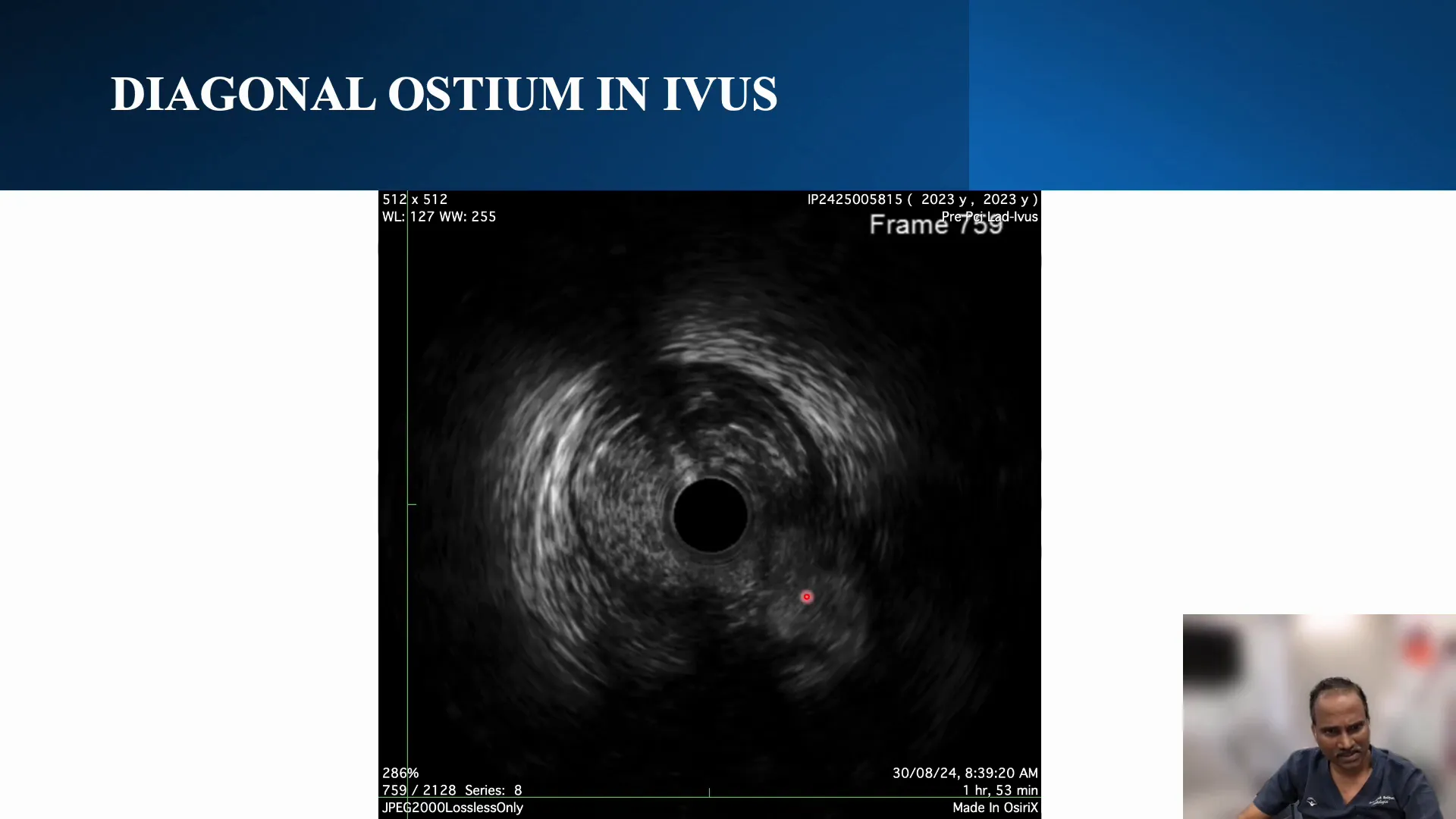
Identifying and addressing obstructions such as flaps at the diagonal osteum is essential to maintain vessel patency. During the procedure, IVUS revealed a flap over the diagonal osteum, which posed a risk of occlusion.
To manage this, a small balloon dilation was performed to assess the severity of the flap. Despite attempts, regular wiring was unsuccessful, confirming the presence of a significant flap that required alternative techniques to address.
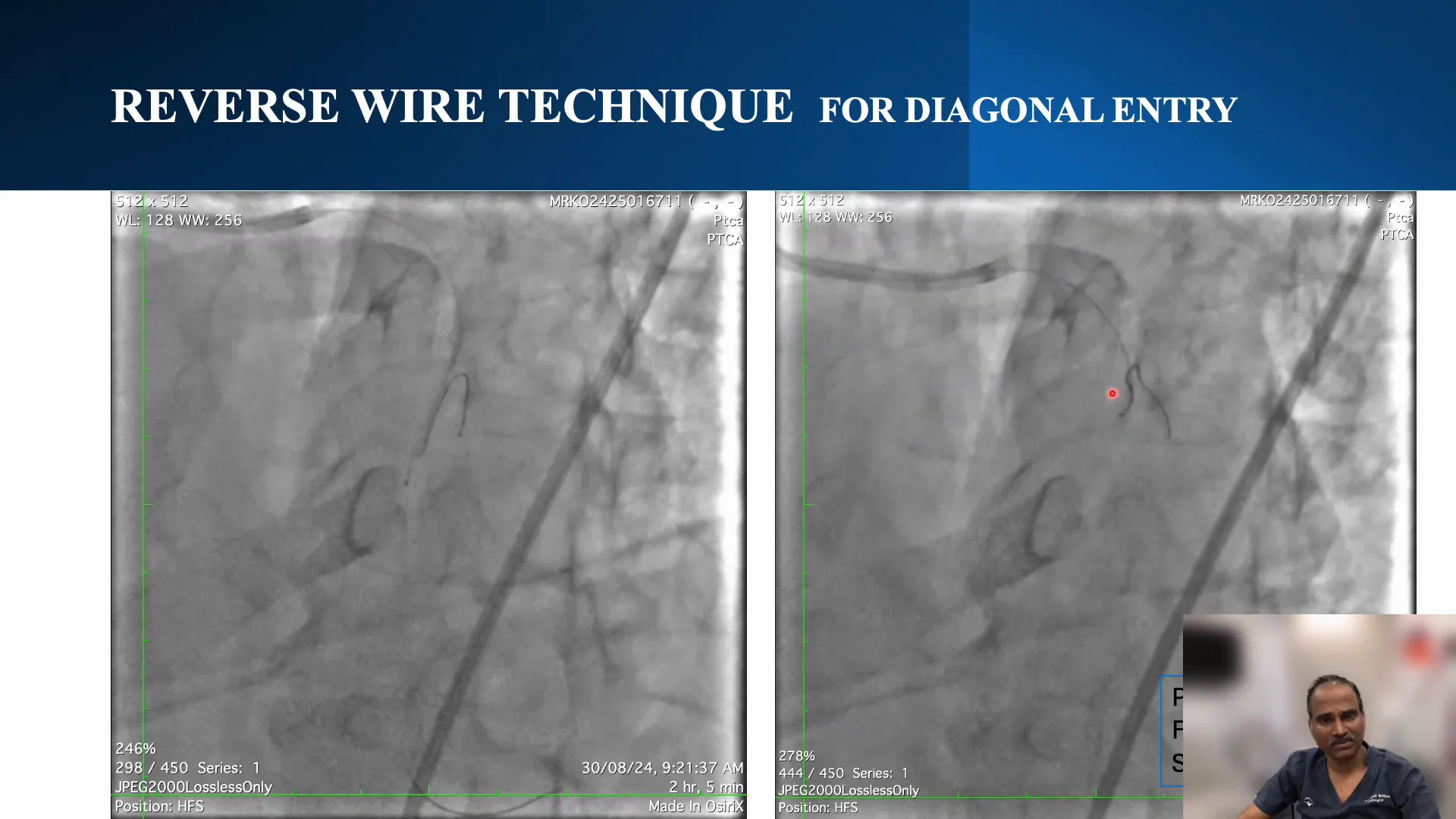
Executing the Reverse Wire Technique
The reverse wire technique can effectively navigate challenging anatomy by redirecting the wire into the desired branch. The procedure involved creating a secondary curve on the wire and using a dual catheter approach for precise navigation.
This technique requires careful manipulation and a good understanding of wire torque characteristics. The wire was guided into the target diagonal branch, overcoming the flap obstruction efficiently. This method allowed for successful wiring despite initial challenges.
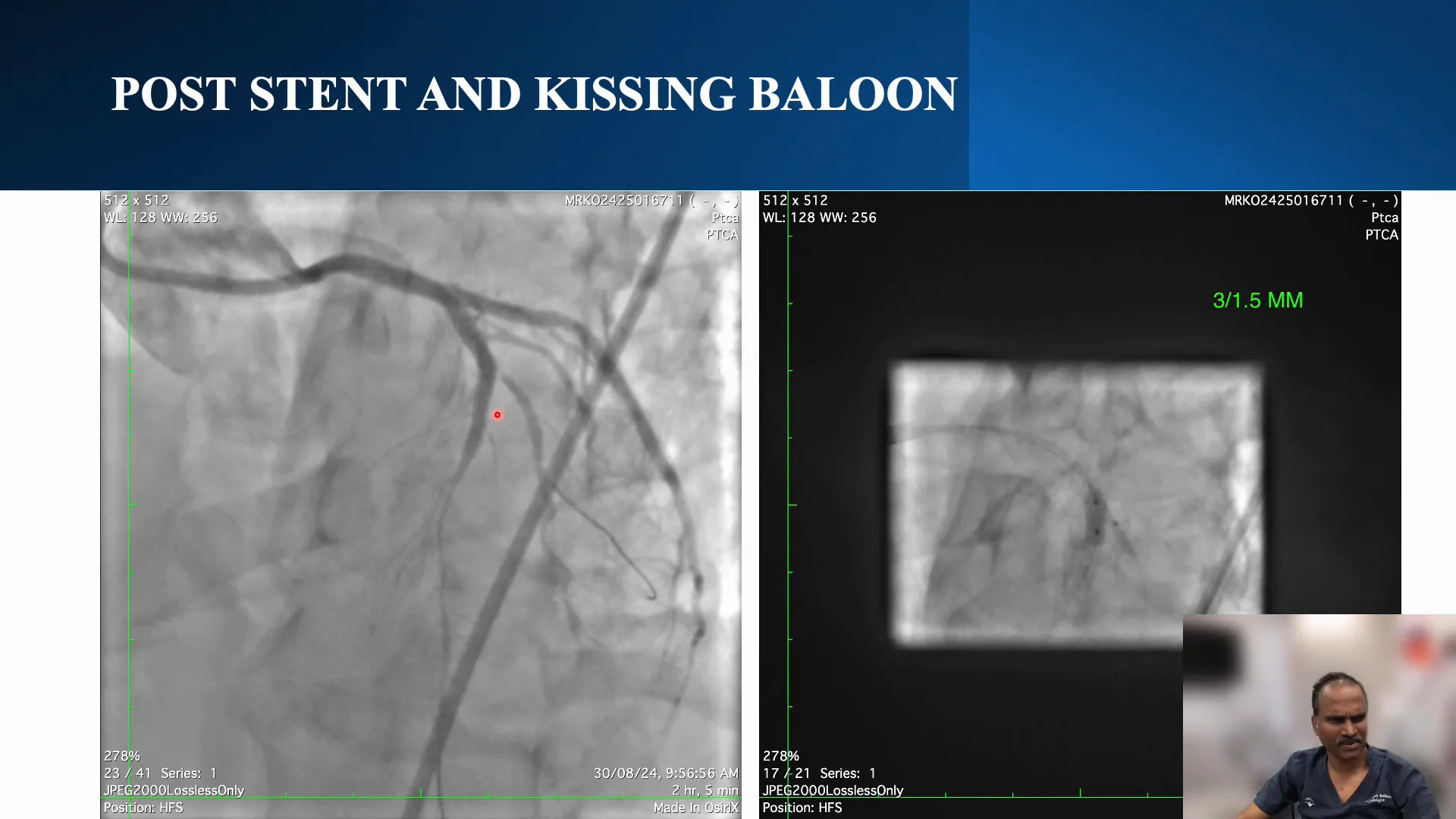
Post-Procedure Analysis and Stenting
Post-procedure, the focus shifted to analyzing the outcomes and ensuring vessel patency. A cutting balloon was used at the diagonal ostium to split the flap, facilitating a provisional stenting strategy. This technique ensures the flap does not occlude the branch post-procedure.
Stenting was performed with a 3.0 x 28 mm stent across the diagonal, achieving satisfactory flow restoration. The final angiogram confirmed the successful management of the diagonal branch with no significant residual stenosis.
Conclusion and Key Takeaways
This case highlights the complexities involved in CTO PCI, particularly when managing side branches at the distal cap. The reverse wire technique proved invaluable in addressing the diagonal osteum flap, demonstrating the need for flexibility and precision in interventional cardiology.
Key takeaways include the importance of thorough pre-procedural planning, the need for adaptability during the procedure, and the effectiveness of advanced techniques like the reverse wire method in overcoming anatomical challenges.
Frequently Asked Questions
What is the reverse wire technique?
The reverse wire technique involves manipulating the wire to redirect it into a specific branch, often using a dual catheter approach. This method is particularly useful in navigating complex coronary anatomy.
How do you manage flaps at the diagonal osteum?
Flaps at the diagonal osteum can be managed using balloon dilation and cutting balloons to split the flap. This approach helps maintain vessel patency and facilitates successful stenting.
What are the risks associated with CTO PCI?
CTO PCI carries risks such as vessel perforation, dissection, and loss of side branches. Careful planning and the use of advanced techniques can mitigate these risks and improve procedural outcomes.


No Comments