08 Mar Mastering LM Bifurcation PCI with DKS Strategy Under IVUS Guidance
In this detailed presentation, we explore the intricacies of Left Main (LM) bifurcation Percutaneous Coronary Intervention (PCI) using the Double-Kissing (DKS) strategy under Intravascular Ultrasound (IVUS) guidance. Join us as we navigate through critical steps and decision-making processes during the procedure, ensuring optimal patient outcomes.
Table of Contents
- Introduction to the Procedure
- Initial Assessment and Strategy Planning
- Handling the Distal Bifurcation: LED and D1
- Evaluating and Dilating the Diagonal Branch
- Assessing the LCX and LED Lesions
- Device Selection and Balloon Dilatation
- Deploying Stents in the LCX
- Crushing the Stents and Recrossing Strategy
- Finalizing Stent Deployment and Optimization
- Final Kissing Balloons Technique
- Post-Dilation and Final Assessment
- Evaluating Final Luminal Areas
- FAQ
Introduction to the Procedure
The Left Main (LM) bifurcation Percutaneous Coronary Intervention (PCI) is a complex procedure that requires precision and expertise. Our approach utilizes the Double-Kissing (DKS) strategy under Intravascular Ultrasound (IVUS) guidance to ensure accuracy and optimal outcomes. This comprehensive method addresses the challenges of managing lesions in the left coronary artery system, particularly those involving the left anterior descending (LAD) artery and its branches.
In this procedure, we focus on two primary areas: the LM bifurcation and the distal bifurcation involving the LAD and D1. Both regions present significant lesions that demand careful strategic planning and execution. Our goal is to systematically address these lesions, ensuring that each step is guided by detailed imaging and precise technique.
Initial Assessment and Strategy Planning
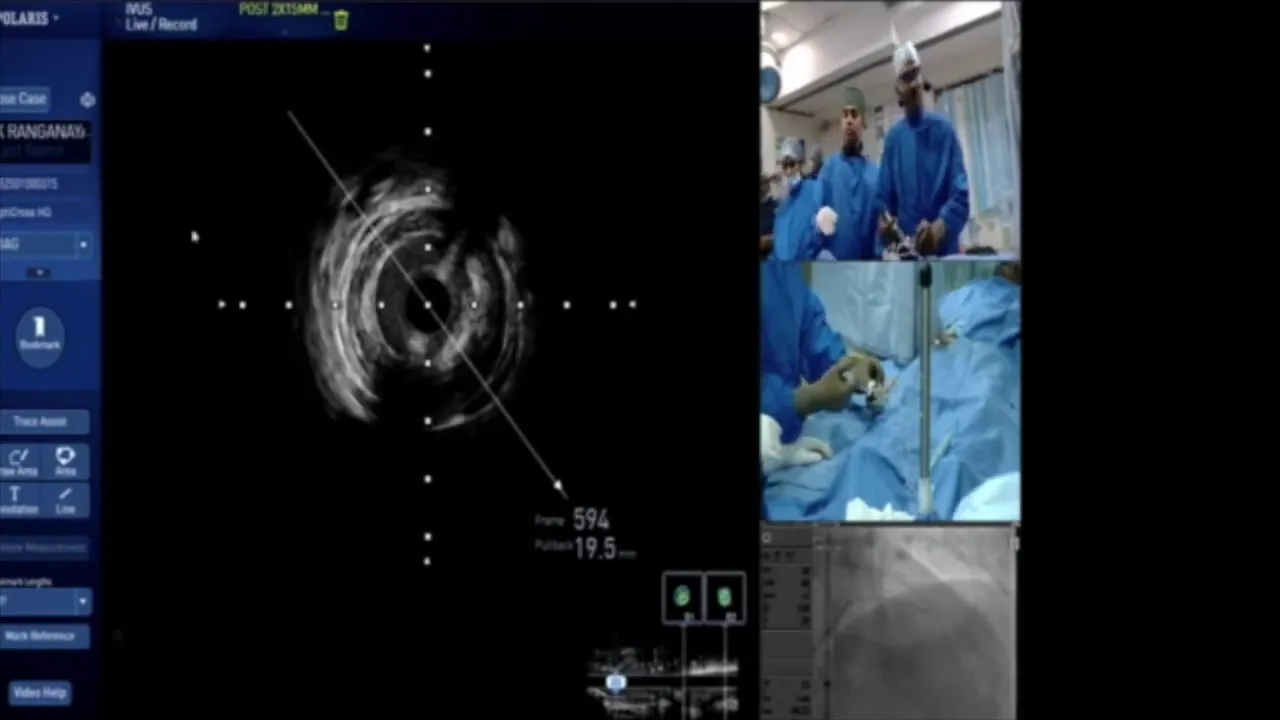
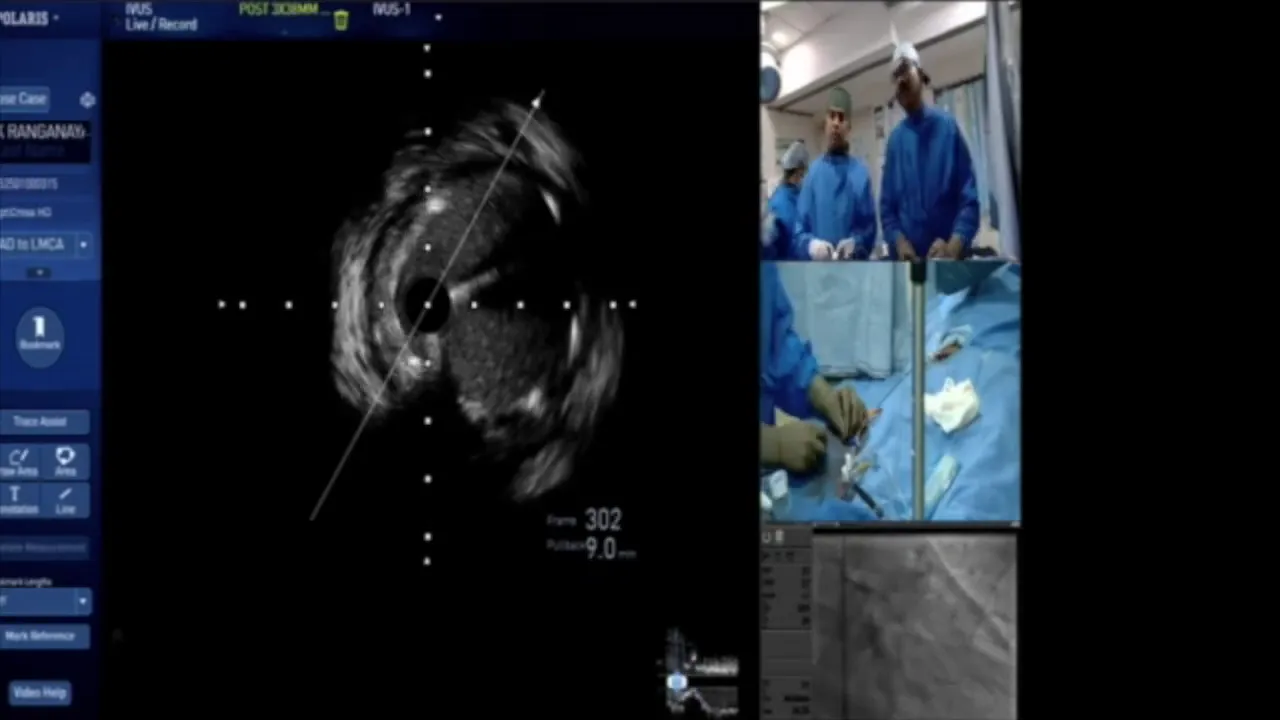
Before initiating the procedure, a thorough assessment of the patient’s coronary anatomy is essential. Using IVUS, we evaluate the severity and extent of the lesions in the LM, LAD, and D1. This imaging modality provides crucial insights into the vessel dimensions and plaque characteristics, guiding our decision-making process.
The strategy involves first addressing the distal bifurcation, specifically the LAD and D1, before moving to the proximal LM bifurcation. This approach allows us to manage the more complex distal lesions first, ensuring that the flow to the vital LAD artery is preserved. Once the distal bifurcation is stabilized, we can confidently proceed to the LM, knowing that the downstream vessels are adequately supported.
Handling the Distal Bifurcation: LED and D1
Our initial focus is on the LAD and its diagonal branch, D1. This involves the precise placement of guidewires and balloons to prepare the lesion for stenting. The LAD is a critical artery, and any intervention must maintain its patency and functionality.
The diagonal branch is initially dilated using a 2 mm non-compliant balloon, aiming to achieve adequate luminal expansion without causing trauma to the vessel walls. This step is crucial as it sets the stage for subsequent interventions. The use of IVUS here allows us to confirm the absence of dissection or hematoma, ensuring the vessel is ready for stenting.
Evaluating and Dilating the Diagonal Branch
Following the initial dilation, further assessment of the diagonal branch is conducted. Using a Wolverine cutting balloon, we attempt to achieve optimal expansion. This specialized balloon allows for precise cutting of the plaque, enhancing luminal gain while minimizing the risk of vessel wall injury.
IVUS imaging post-dilation confirms the luminal area and helps in deciding whether further intervention is necessary. The goal is to ensure that the diagonal branch is sufficiently opened to maintain adequate blood flow, while avoiding unnecessary interventions that could complicate the procedure.

Assessing the LCX and LED Lesions
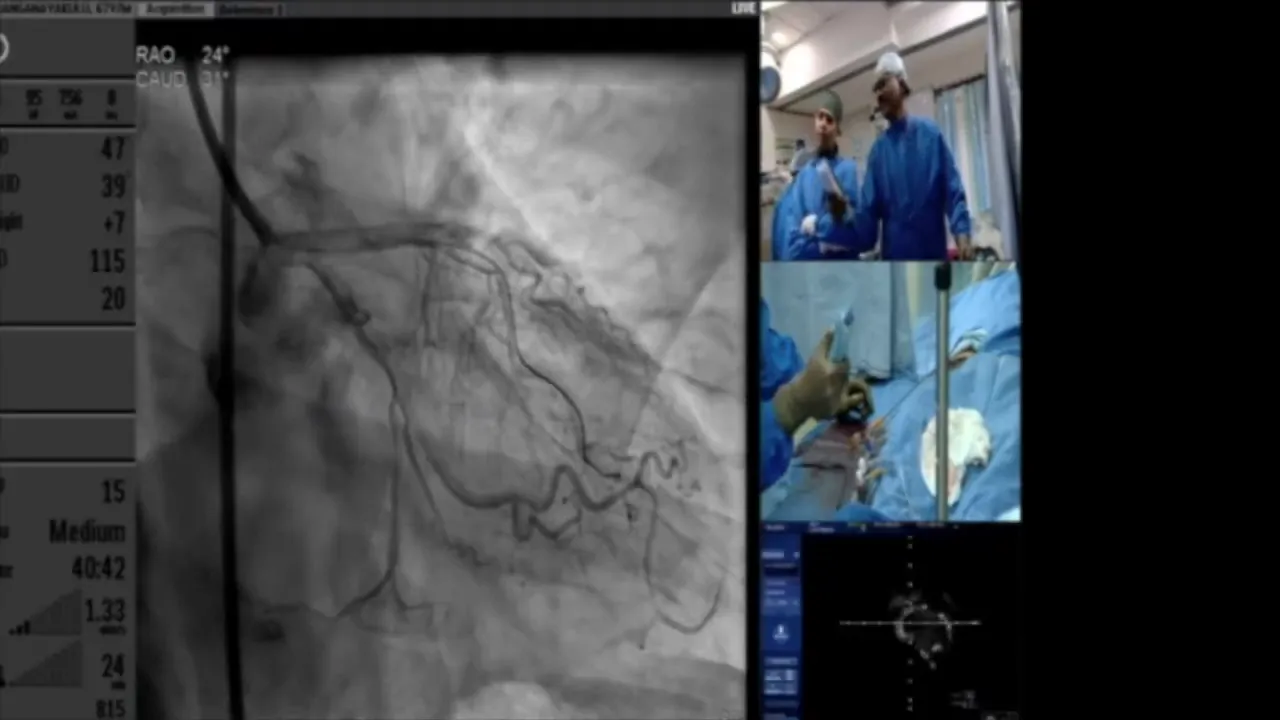
With the diagonal branch stabilized, attention turns to the Left Circumflex (LCX) and the LAD lesions. The LCX, being a major branch of the LM, requires careful consideration. IVUS measurements indicate the vessel size and the extent of the lesion, guiding our choice of balloon and stent sizes.
A 2.5 mm cutting balloon is used to pre-dilate the LCX lesion, preparing it for stenting. This step is crucial as it facilitates the passage and deployment of the stent, ensuring it conforms well to the vessel wall. The LAD is similarly assessed, with IVUS providing detailed insights into the vessel dimensions and lesion characteristics.
Device Selection and Balloon Dilatation
Choosing the right devices for the procedure is pivotal. Based on IVUS measurements, we select stents and balloons that match the vessel dimensions. The goal is to achieve optimal stent apposition and expansion, minimizing the risk of restenosis.
Balloon dilatation is performed using non-compliant balloons sized according to the vessel diameter. The LCX and LAD are sequentially dilated, ensuring that each segment is adequately prepared for stenting. This meticulous approach helps in achieving a uniform expansion, reducing the risk of complications.
Deploying Stents in the LCX
Once the vessels are prepared, stents are deployed in the LCX. The stent size is chosen based on the vessel’s luminal dimensions, ensuring full coverage of the lesion. Deployment is carefully monitored using IVUS to confirm proper expansion and apposition against the vessel wall.
After stent deployment, post-dilatation is performed to optimize the stent’s position. This involves using a slightly larger balloon to ensure the stent is well apposed and the vessel is adequately expanded. The use of IVUS at this stage provides real-time feedback, confirming the success of the intervention.

Crushing the Stents and Recrossing Strategy
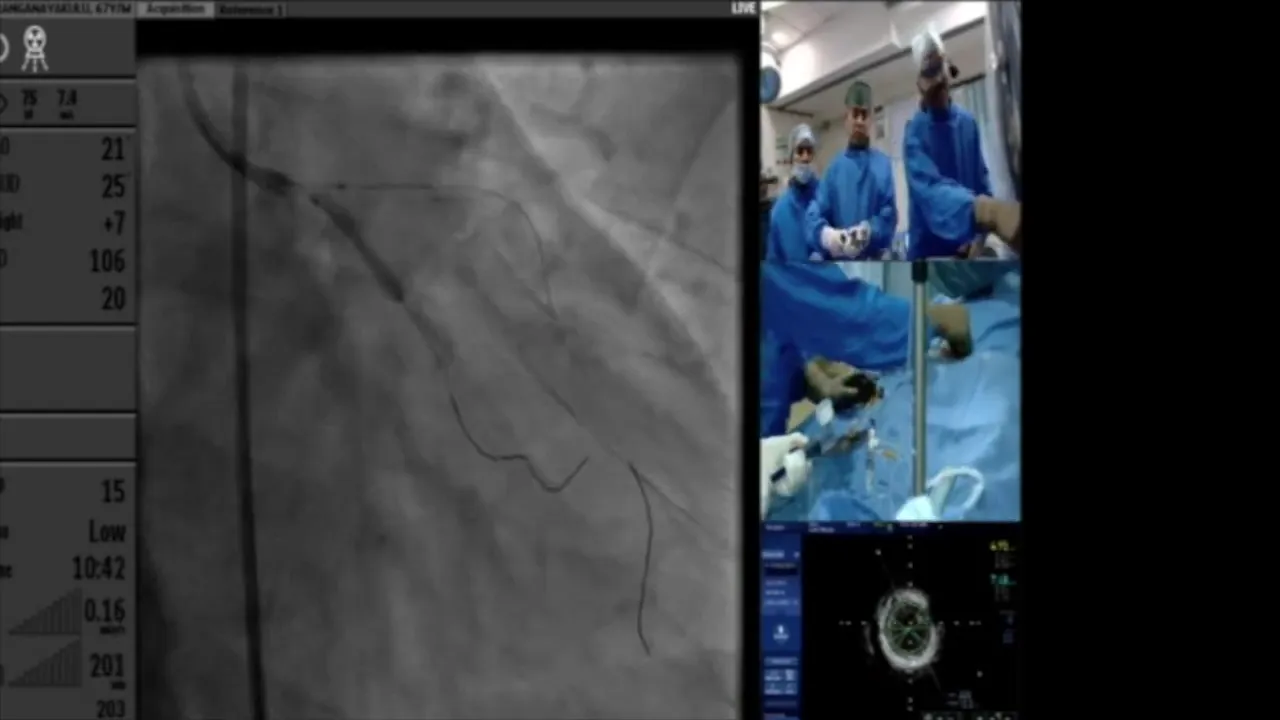
After the initial stent deployment in the LCX, we proceeded to crush the stent using a 3.25 mm balloon. This step is crucial to ensure the stent is adequately apposed against the vessel wall. However, if the initial crush is inadequate, a larger pot balloon of 4.25 mm is used to provide additional pressure and ensure optimal stent positioning.
Recrossing is a delicate step that requires precision. The shape of the wire is critical when recrossing to ensure it navigates through the stent struts without causing any damage. It’s essential to confirm the wire’s position using IVUS to avoid distal stent strut penetration, which can lead to complications.
Finalizing Stent Deployment and Optimization
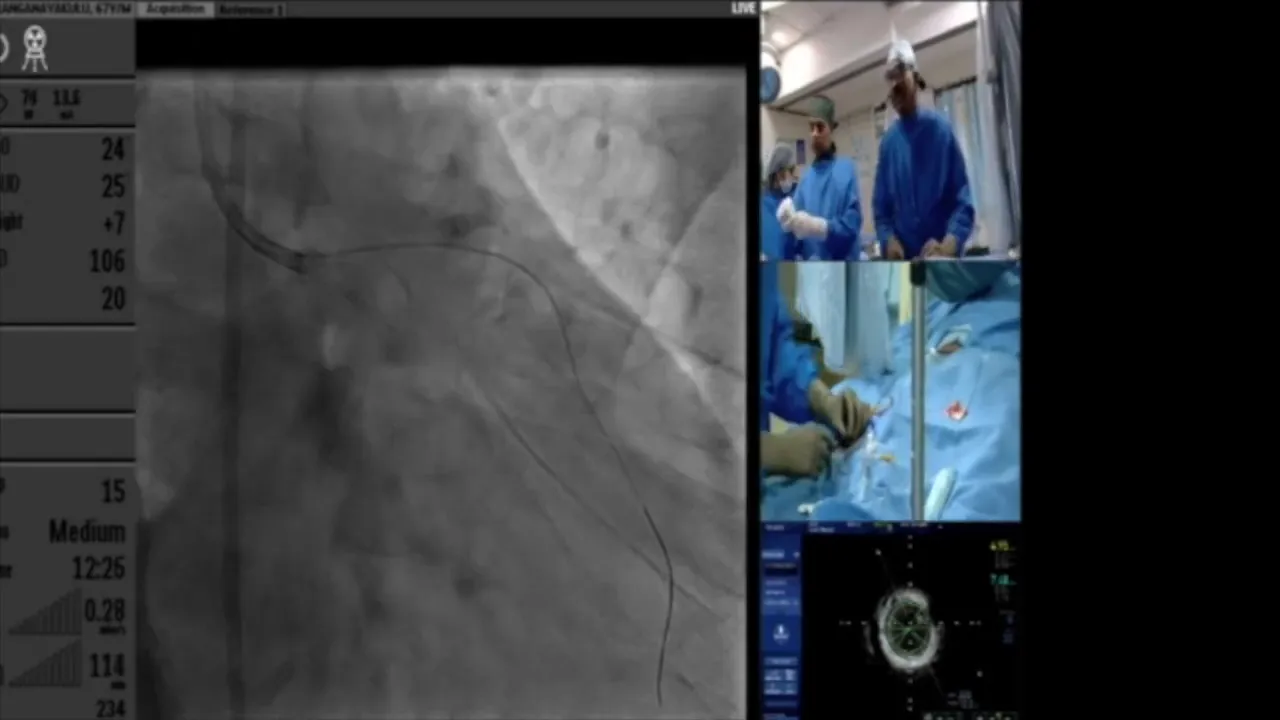
Once the stent is crushed and the wire is recrossed, the next step involves optimizing the stent deployment. This is achieved by performing post-dilation with a non-compliant balloon sized to the vessel’s luminal diameter. The goal is to ensure the stent is fully expanded and well-apposed to the vessel wall.
IVUS imaging is used to confirm the stent’s position and expansion, ensuring there are no areas of under-expansion or malapposition. This step is critical to prevent restenosis and ensure long-term patency of the vessel.

Final Kissing Balloons Technique
The final kissing balloons technique is performed to ensure both branches of the bifurcation are adequately opened and supported. This involves simultaneous inflation of balloons in both the LAD and LCX to optimize the stent geometry and ensure even distribution of the stent struts across the bifurcation.
This technique helps in achieving a more uniform expansion and reduces the risk of restenosis at the bifurcation site. The use of IVUS during this step confirms the success of the technique by showing a well-expanded stent with no residual stenosis.

Post-Dilation and Final Assessment
Post-dilation is performed using a slightly larger balloon to ensure the stent is optimally expanded. This step is crucial for ensuring the stent conforms perfectly to the vessel wall and that any areas of concern are addressed before concluding the procedure.
Final assessment with IVUS provides a comprehensive view of the stent and vessel, confirming the absence of complications such as dissections or stent malapposition. This imaging ensures that the procedure’s outcomes meet the desired standards for patient safety and efficacy.
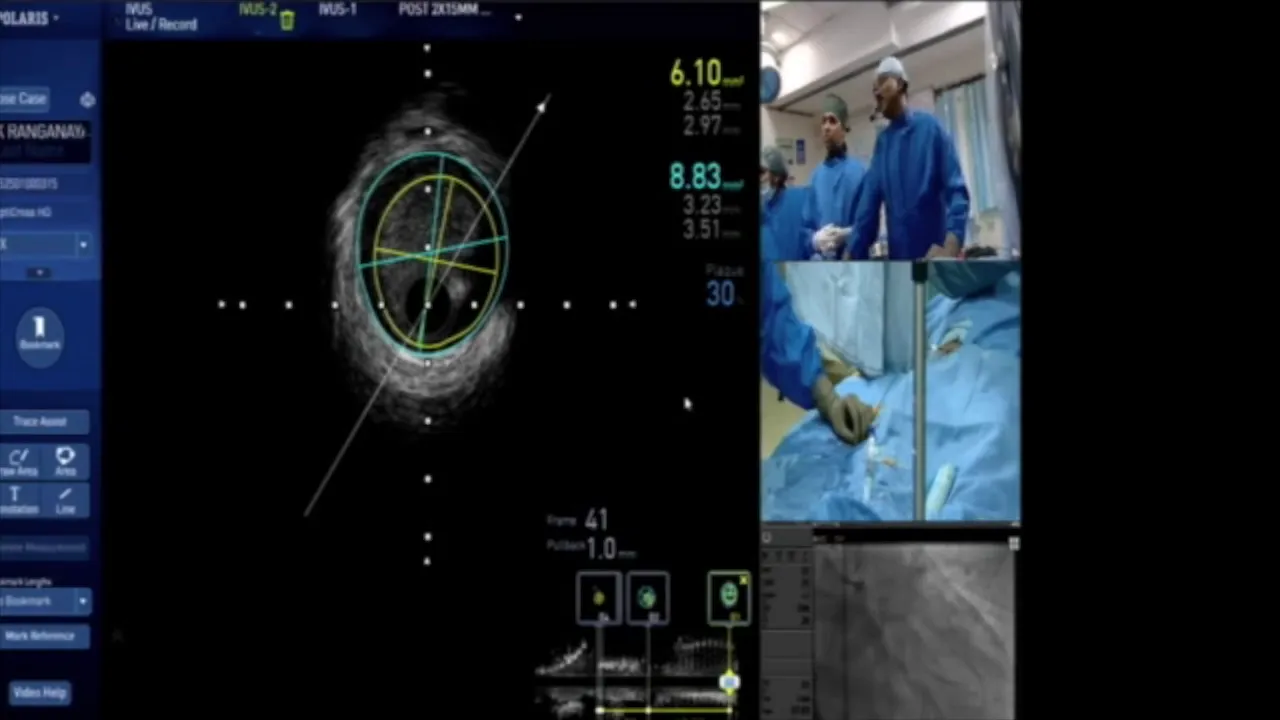
Evaluating Final Luminal Areas
After completing the procedure, it is essential to evaluate the final luminal areas to ensure they meet the expected outcomes. In this case, the final luminal areas of the LED were approximately 7.1 mm², and the LCX was around 5.5 mm². These measurements indicate a successful expansion and adequate blood flow through the treated vessels.
Ensuring optimal luminal areas is crucial for preventing future cardiac events and maintaining the long-term success of the PCI. Regular follow-up with imaging can help monitor the stent’s performance and detect any early signs of restenosis.
FAQ
What is the significance of using the Double-Kissing (DKS) strategy?
The DKS strategy is significant because it allows for optimal stent apposition and expansion in bifurcation lesions, reducing the risk of restenosis and ensuring long-term patency of the treated vessels.
Why is IVUS guidance important in this procedure?
IVUS guidance provides detailed imaging of the vessel and stent, allowing for precise assessment and optimization of the stent deployment. It helps in identifying areas of under-expansion or malapposition that may not be visible with angiography alone.
How does the final kissing balloons technique improve outcomes?
This technique ensures that both branches of the bifurcation are adequately supported, reducing the risk of restenosis and ensuring even distribution of the stent struts. It enhances the procedural success by optimizing the geometry and expansion of the stent at the bifurcation site.

No Comments