13 Nov IVUS Guided PCI: A Comprehensive Guide to LMCA to LAD Rotablation
In this detailed exploration, we delve into the intricacies of IVUS guided PCI, specifically focusing on the rotablation technique used for treating the Left Main Coronary Artery (LMCA) to Left Anterior Descending artery (LAD) in a post-CABG patient. Join us as we break down the procedural steps, challenges faced, and the critical decisions made throughout the intervention.
Table of Contents
- Introduction to the Case
- Balloon Angioplasty Considerations
- Detailed Analysis of Calcium Scoring
- Post-Dilation and Stenting Strategy
- Final Stent Deployment
- Post-Procedure Imaging and Results
- Complications and Troubleshooting
- Finalizing the Procedure
- Conclusion and Key Takeaways
- FAQs
Introduction to the Case
The case involves a patient with a significant history of coronary artery disease, who previously underwent Coronary Artery Bypass Grafting (CABG). The current focus is on addressing severe calcification in the Left Anterior Descending (LAD) artery, which requires a meticulous approach for successful intervention. The complexity of the calcification necessitates advanced techniques such as rotablation, guided by Intravascular Ultrasound (IVUS), to ensure precision and efficacy in treatment.
Understanding the Patient’s Background
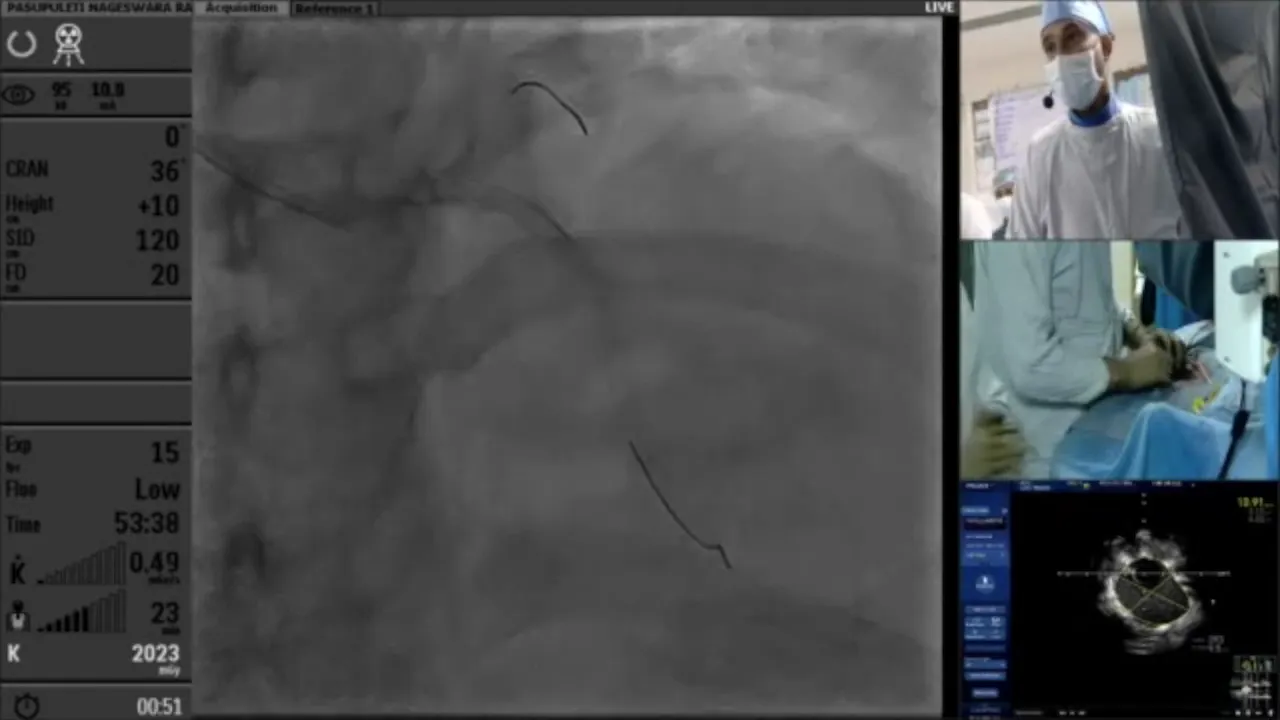
The patient, who had previously undergone CABG, presented with calcified lesions in the LAD. A CT angiogram revealed the extent of calcification, which was initially thought to be in the LAD but was instead found in the diagonal artery. This misplacement highlights the intricacies and challenges often encountered in post-CABG patients, emphasizing the need for accurate imaging and careful planning.
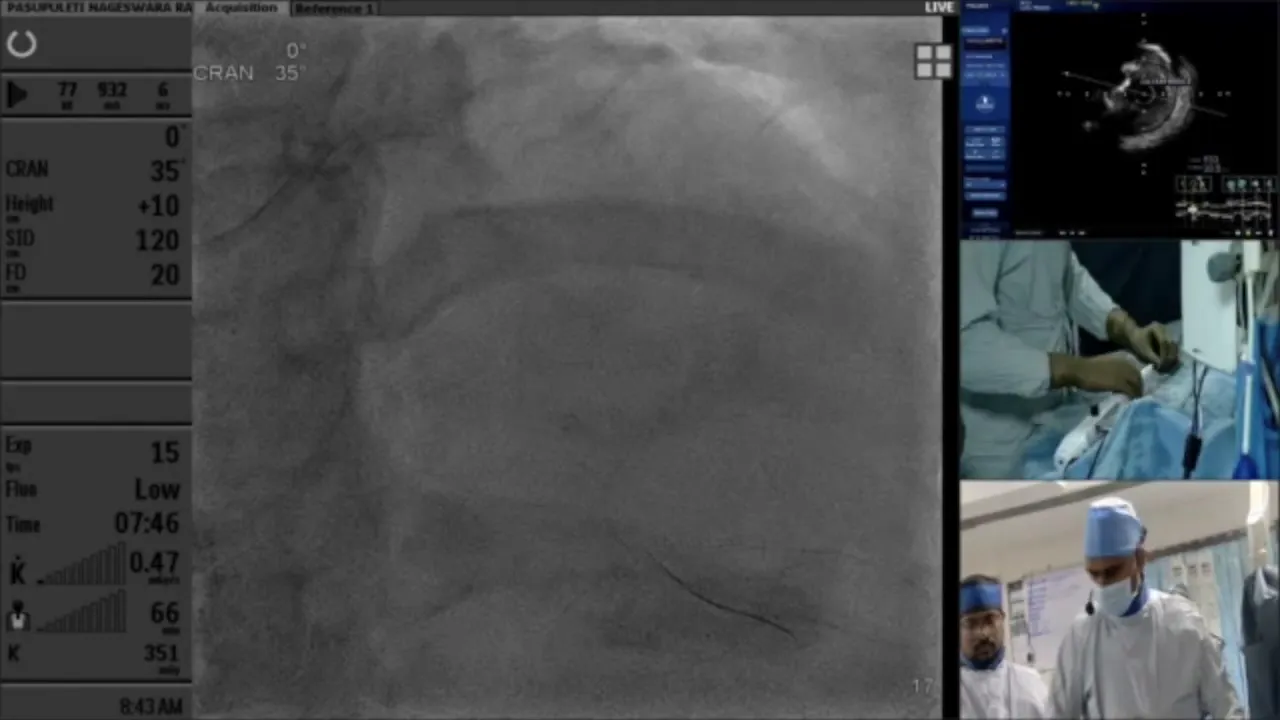
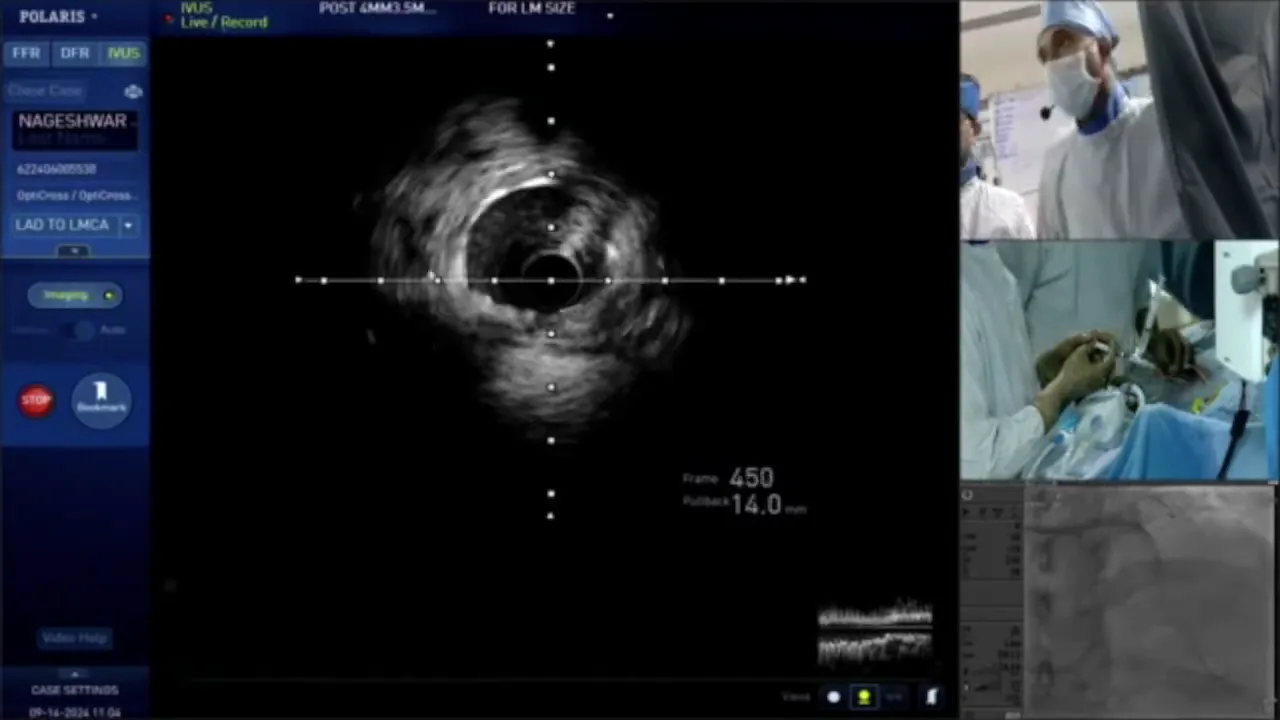
Initial Assessment and Imaging
During the initial assessment, a CT scan was performed to evaluate the coronary anatomy and the degree of calcification. The scan confirmed severe calcification, necessitating a strategy for calcium modification. IVUS was planned to further assess the lesion characteristics and guide the intervention.
Calcium Modification Strategy
The presence of heavy calcification in the LAD called for a robust calcium modification strategy. The team decided to proceed with rotablation, a technique specifically designed to tackle heavily calcified plaques by using a diamond-tipped burr to ablate the calcified lesion, thus facilitating stent delivery.
Preparing for Rotablation
Preparation for rotablation involved selecting the appropriate burr size and ensuring the correct setup of the RotaPro system. The team chose a 1.5 mm burr, considering the vessel size and the extent of calcification. The single-operator technique was employed, allowing one operator to control the procedure, ensuring precision and control throughout the process.
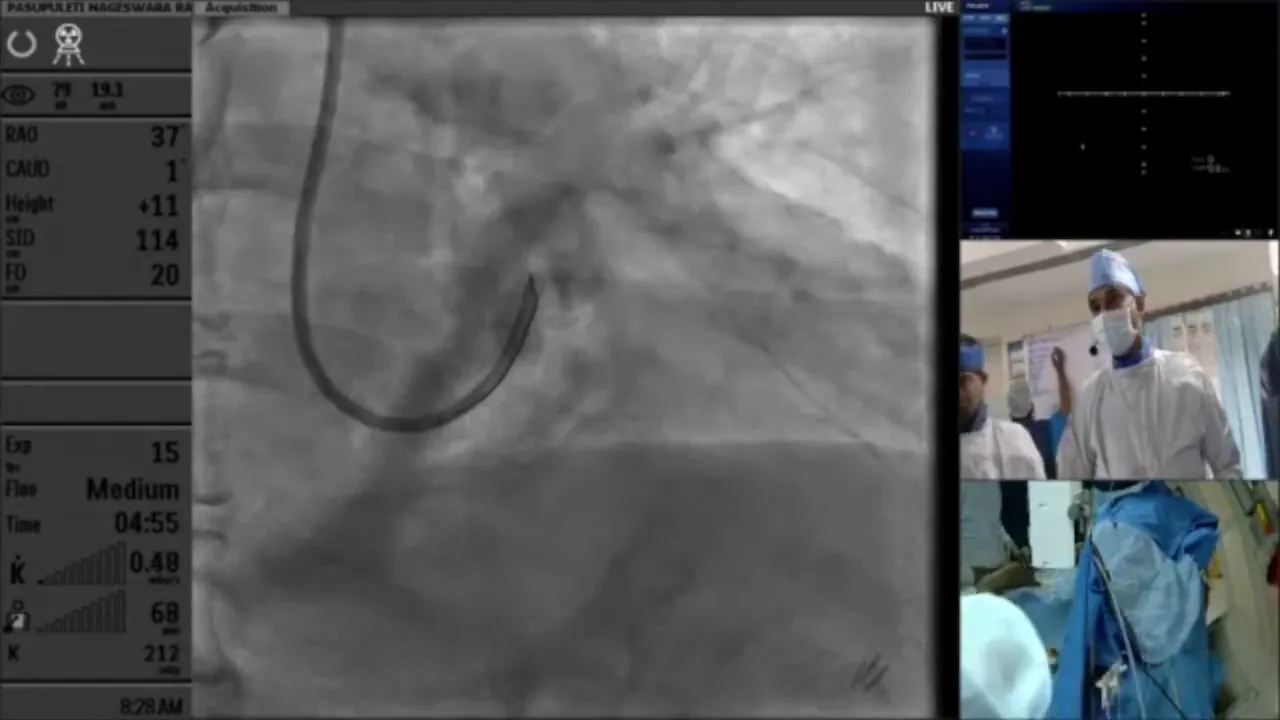
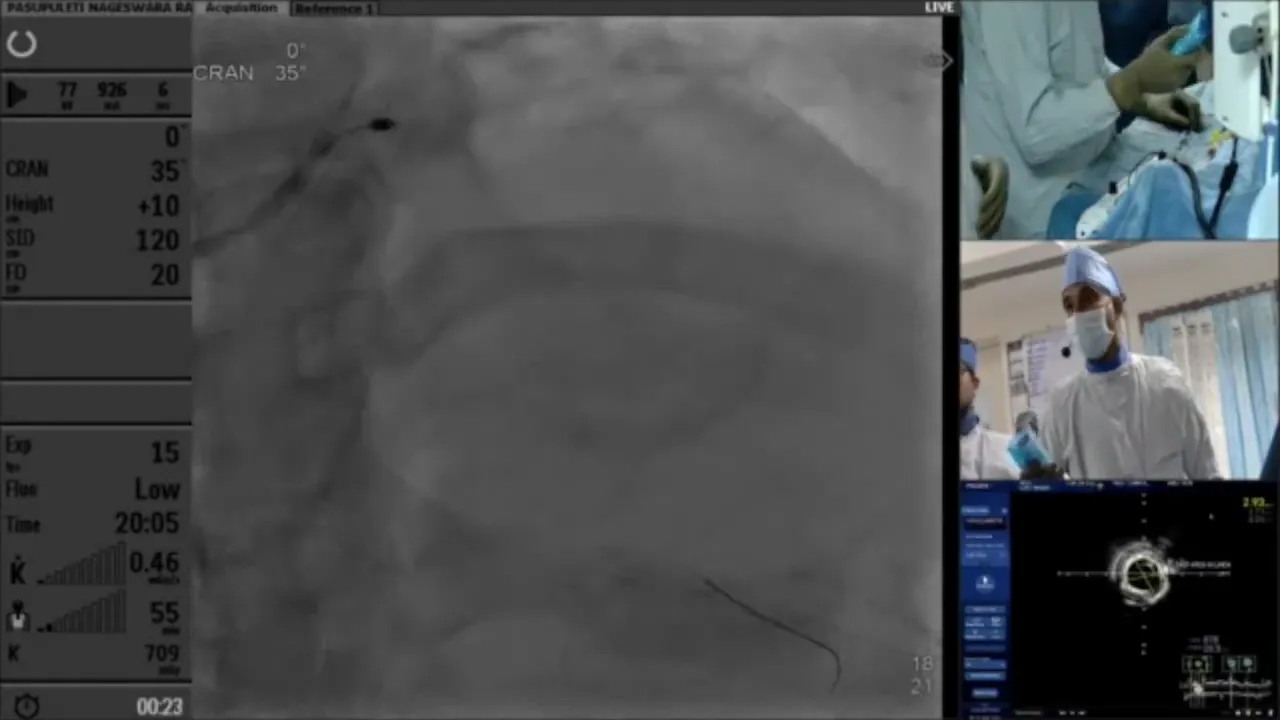
Executing the Rotablation
The rotablation procedure commenced with the insertion of the RotaWire and the advancement of the rotablation burr. The single-operator technique facilitated seamless operation, with the operator managing both the burr rotation and advancement. This approach provided enhanced control and minimized procedural complications.
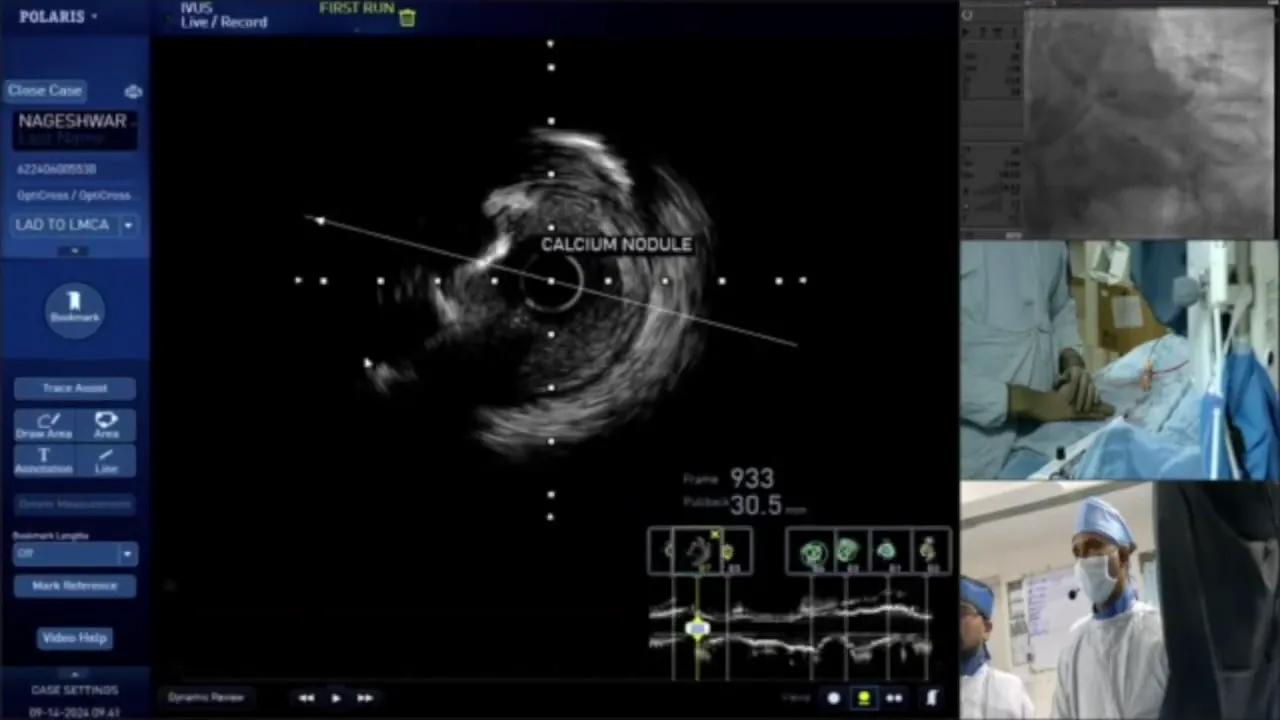
Identifying Calcium Nodules
During the procedure, IVUS imaging revealed prominent calcium nodules at specific sites within the artery. These nodules required careful navigation and precise rotablation to ensure complete modification of the calcified segments, thereby improving the likelihood of successful stent deployment.
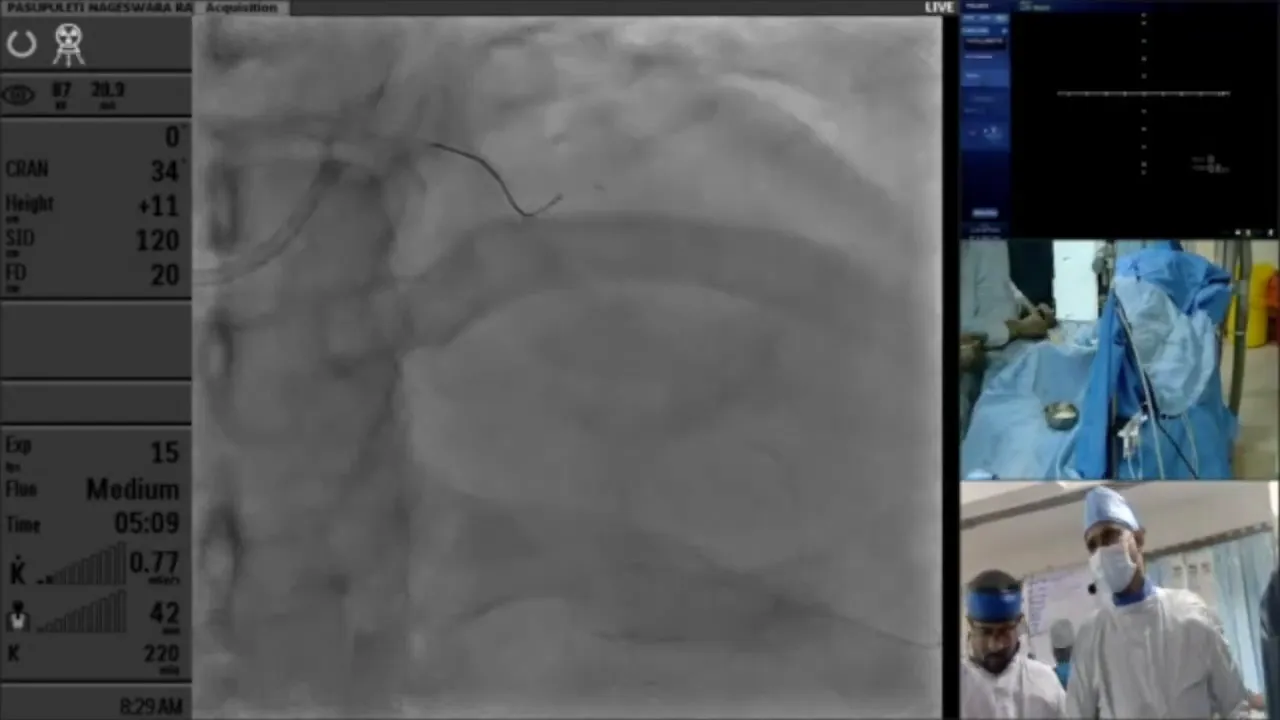
Finalizing Rotablation Techniques
After the initial rotablation passes, the team performed additional polishing runs to ensure complete plaque modification. Attention was given to areas where resistance was noted, ensuring that all calcified segments were adequately treated. This step was crucial for achieving optimal stent expansion and apposition.
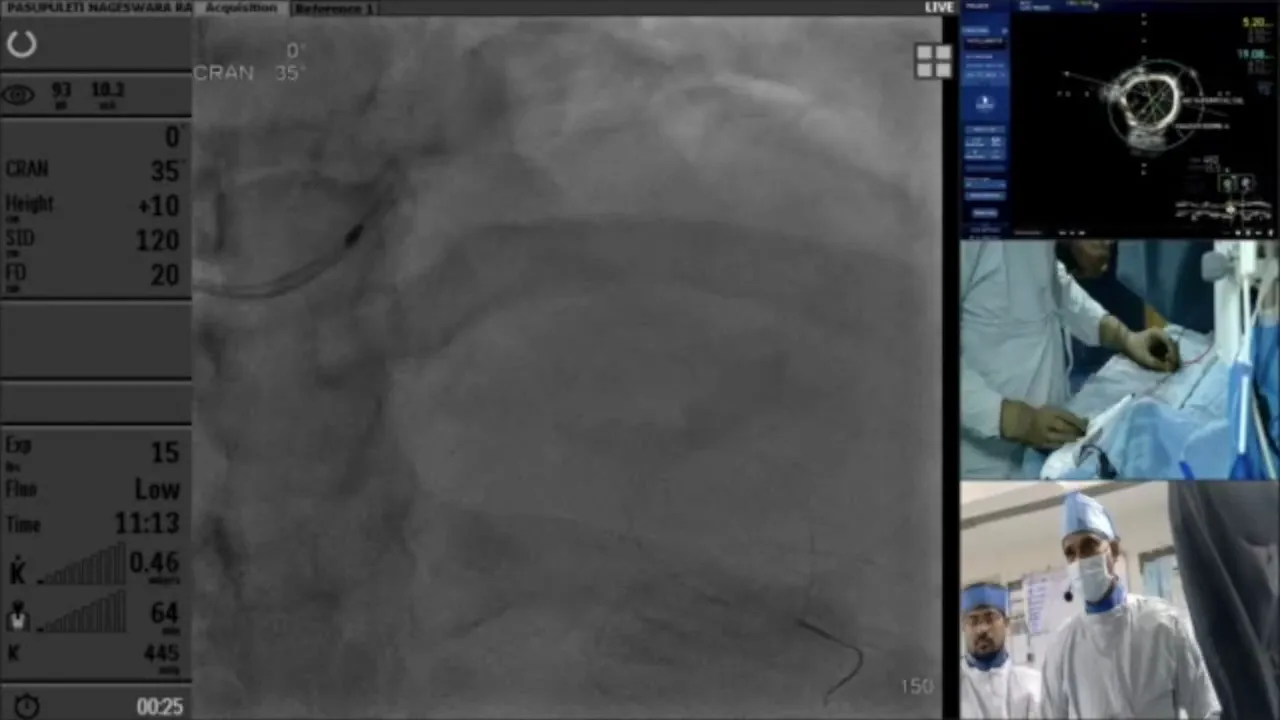
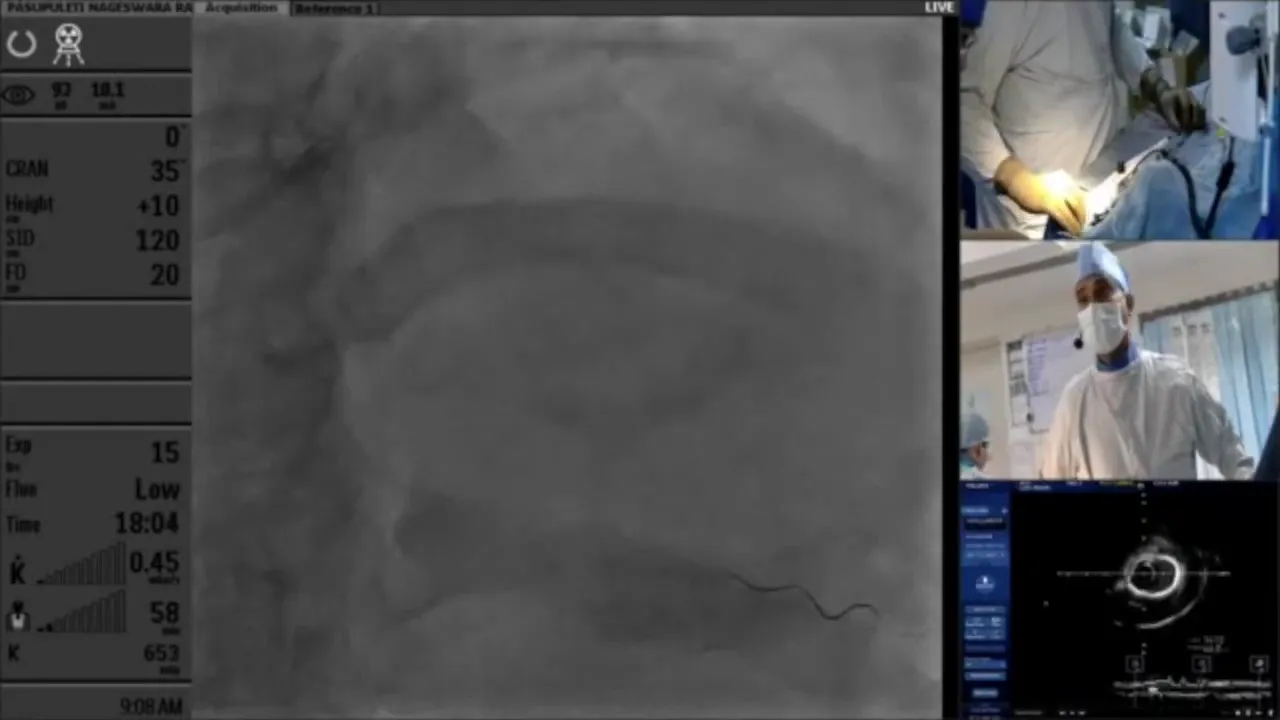
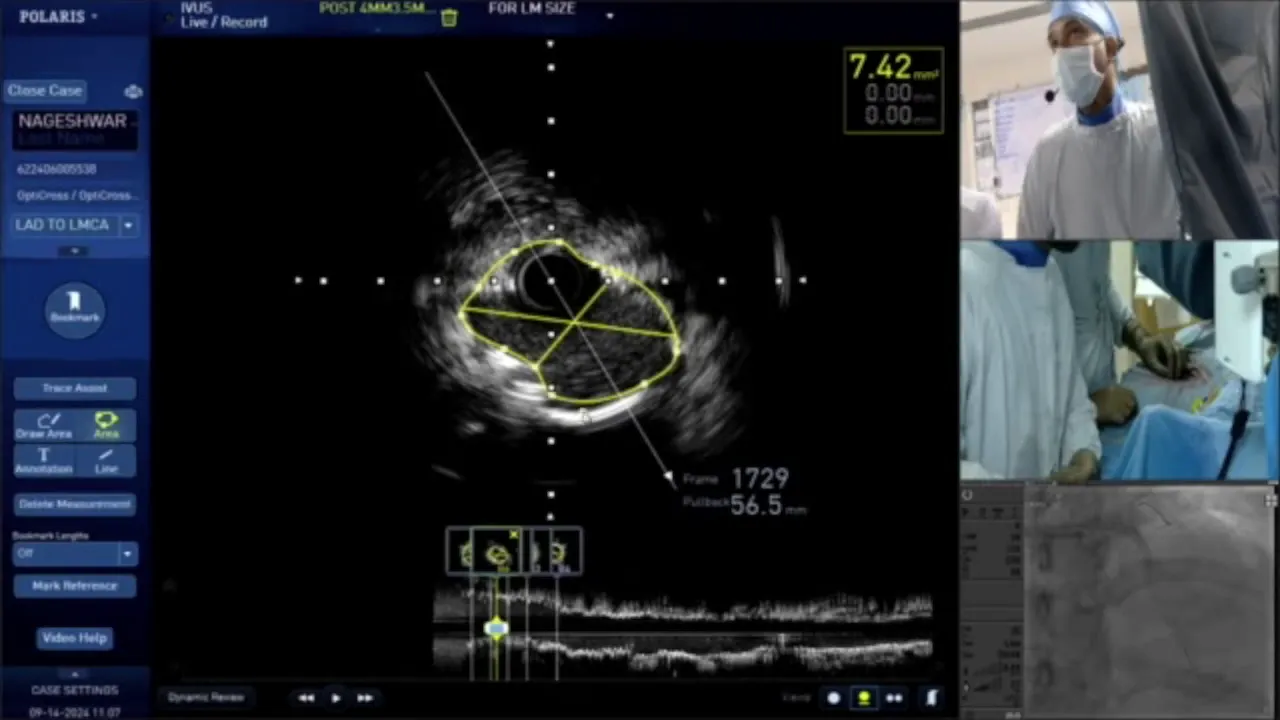
Post-Rotablation Assessment
Following rotablation, a thorough assessment was conducted using IVUS to evaluate the effectiveness of the procedure. The imaging confirmed satisfactory modification of calcified lesions, with plans to proceed with further plaque modification techniques if necessary. The team prepared for potential additional interventions, such as the use of cutting balloons, to address any residual calcification.
Balloon Angioplasty Considerations
Balloon angioplasty is a critical step in the procedure, especially when dealing with heavily calcified lesions. The choice of balloon type, whether cutting or non-cutting, is crucial as it determines the success of lesion modification and stent deployment.
In cases with significant calcification, a cutting balloon may be preferred due to its ability to create controlled incisions in the plaque, facilitating better expansion and stent apposition. However, the challenge lies in navigating through tight or tortuous lesions, where low-profile balloons might be necessary.
Detailed Analysis of Calcium Scoring
Calcium scoring plays a pivotal role in planning the intervention strategy. It involves assessing the degree of calcification, which can be quantified by the extent of calcium arc and nodule presence. A score of four, as identified in this case, indicates the need for aggressive plaque modification techniques such as rotablation.
Understanding the calcium score helps in tailoring the approach, whether to proceed with further rotablation or utilize adjunctive devices like cutting balloons to achieve optimal stent deployment.
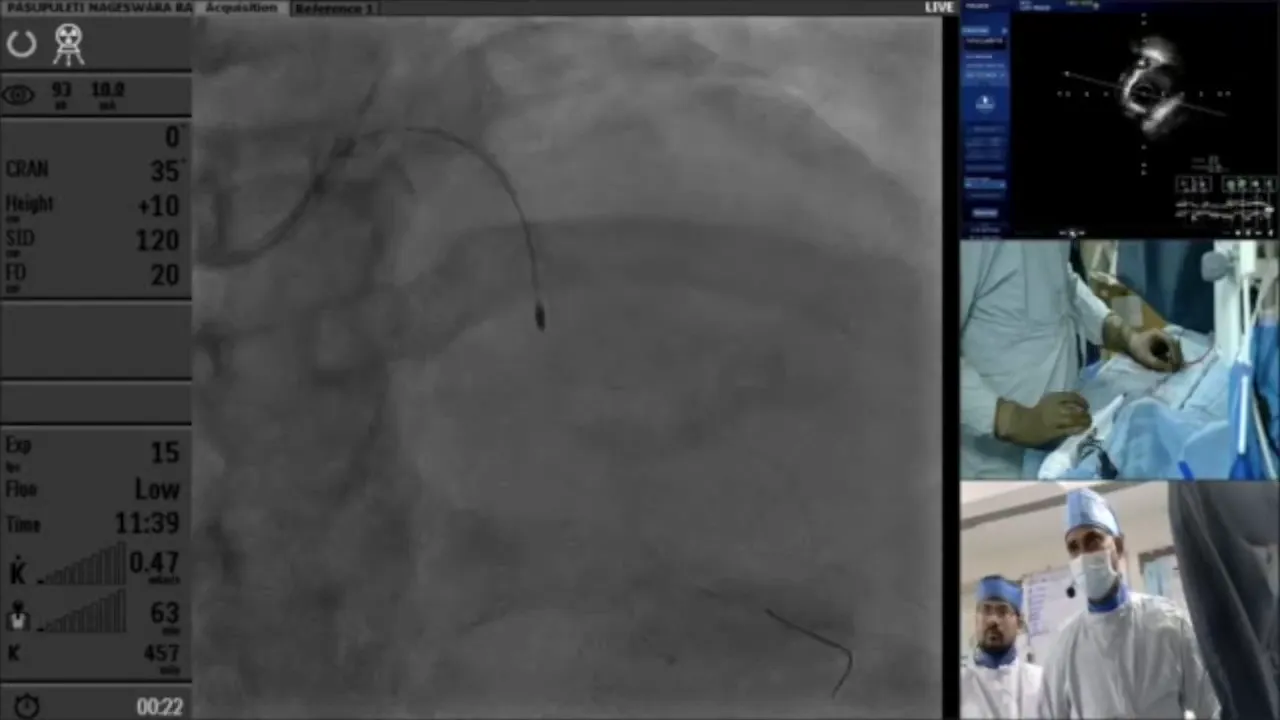
Post-Dilation and Stenting Strategy
Post-dilation is a crucial step following initial stent deployment. It ensures optimal stent expansion and apposition against the vessel wall. Selecting the appropriate balloon size and pressure is vital to achieve a satisfactory result without causing vessel injury.
In this case, post-dilation was performed using a non-compliant balloon to achieve uniform expansion. The strategy involved gradual pressure increments to avoid complications such as dissection or perforation.
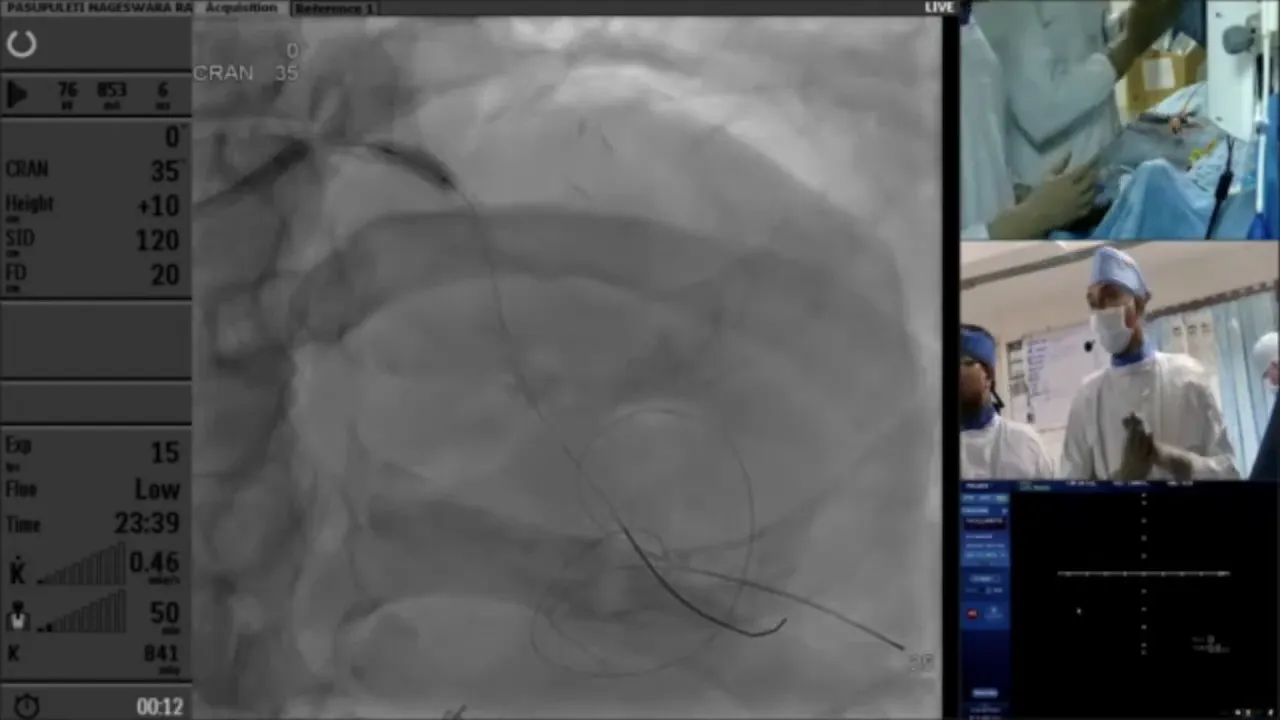
Final Stent Deployment
The final stent deployment marks the culmination of the procedural steps, where precision and careful planning are paramount. Ensuring proper landing zones and overlap with existing stents are key considerations to prevent restenosis and ensure long-term patency.
During the deployment, continuous imaging guidance is employed to verify the accurate positioning and expansion of the stent, ensuring no edge dissections or malapposition occur.
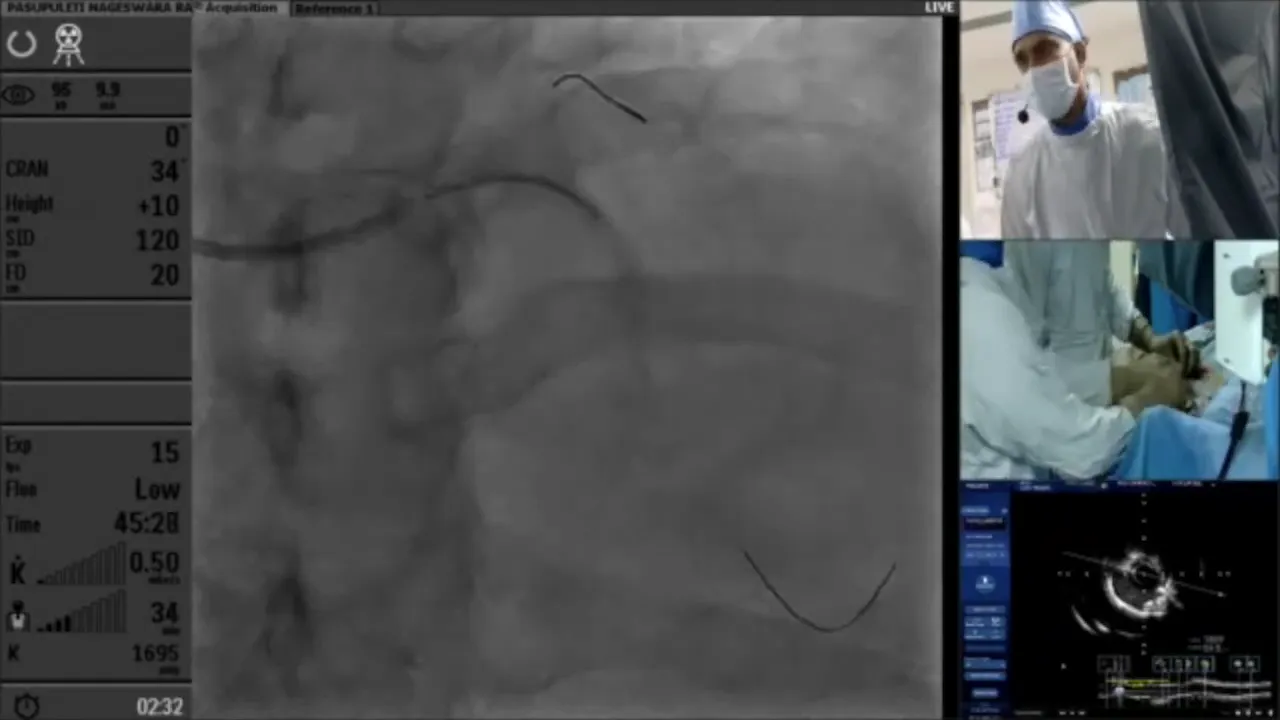
Post-Procedure Imaging and Results
Post-procedure imaging is essential to confirm the success of the intervention. Intravascular ultrasound (IVUS) or optical coherence tomography (OCT) can be used to assess stent expansion, apposition, and the presence of any residual stenosis or dissections.
The imaging in this case demonstrated satisfactory stent expansion and apposition, with no significant residual stenosis, confirming the success of the procedure.
Complications and Troubleshooting
Complications during PCI can include vessel dissection, perforation, or stent thrombosis. Prompt identification and management of these complications are crucial to patient safety.
Troubleshooting involves addressing any identified issues, such as performing additional post-dilation or deploying additional stents if necessary. Continuous monitoring and readiness to adapt the strategy are essential components of successful PCI.
Finalizing the Procedure
The procedure is finalized by ensuring hemostasis, removing all guidewires, and ensuring no immediate post-procedural complications. Patient monitoring continues in the recovery area to observe for any late complications.
Documentation of the procedure details and outcomes is critical for future reference and ongoing patient management.
Conclusion and Key Takeaways
This case highlights the complexities involved in PCI, particularly in heavily calcified lesions. The use of advanced imaging techniques and calcium modification strategies are key to successful outcomes.
Key takeaways include the importance of thorough pre-procedural planning, the selection of appropriate tools and techniques, and the need for flexibility in adapting to intra-procedural findings.
FAQs
- What is the role of IVUS in PCI? IVUS provides detailed images of the vessel and lesion characteristics, guiding the intervention strategy and confirming procedural success.
- When is rotablation preferred? Rotablation is preferred in cases of severe calcification where conventional balloon angioplasty may not suffice.
- What are the risks associated with PCI? Potential risks include vessel dissection, perforation, and stent thrombosis, which require prompt management.
- How is calcium scoring used in PCI? Calcium scoring helps in assessing the severity of calcification, guiding the choice of intervention techniques and devices.


No Comments