29 Dec IVUS-GUIDED Multivessel PCI with RCA CTO PCI: A Practical Case Walkthrough
Chronic total occlusions of the right coronary artery are often deceptively simple on one view and complex on another. The procedural plan must balance anatomy, collateral supply, and the risk of losing important branches such as the posterior descending artery. This case illustrates a stepwise approach to a multivessel intervention that combined IVUS guidance, careful wire selection, antegrade escalation, and selective retrograde microcatheter injections to resolve ambiguity at the distal cap and preserve the PDA.
Table of Contents
- Case snapshot
- Initial anatomic assessment and strategy
- Why treat the donor vessel first?
- Antegrade strategy and early escalation
- When the wire is in the vessel but far from the true lumen
- Knuckle technique: when and why
- Retrograde microcatheter injection to unmask the distal cap
- Integrated antegrade-retrograde strategy
- Crossing and exchange technique
- IVUS-guided optimization
- Understanding misleading angiographic courses
- Key takeaways and procedural pearls
- Recommended antegrade wire escalation algorithm for ambiguous RCA CTO
- Common pitfalls
- Examples of confusing RCA courses
- Conclusion
- When should I treat the donor vessel before attempting the CTO?
- How does a selective retrograde microcatheter injection help?
- When should I use a knuckle wire?
- Which wires should I use in ambiguous courses?
- How essential is IVUS in CTO PCI?
- Does CT overlay always solve angiographic ambiguity?
Case snapshot
A 55-year-old man with type 2 diabetes and hypertension presented with Canadian Cardiovascular Society class III effort angina for one month and recent rest angina. He had a diagnosis consistent with non-ST elevation myocardial infarction and preserved left ventricular systolic function. Renal function was normal. The left coronary system had significant disease requiring PCI, and the right coronary artery (RCA) had a short CTO with an uncertain distal cap and favorable distal vessel quality.
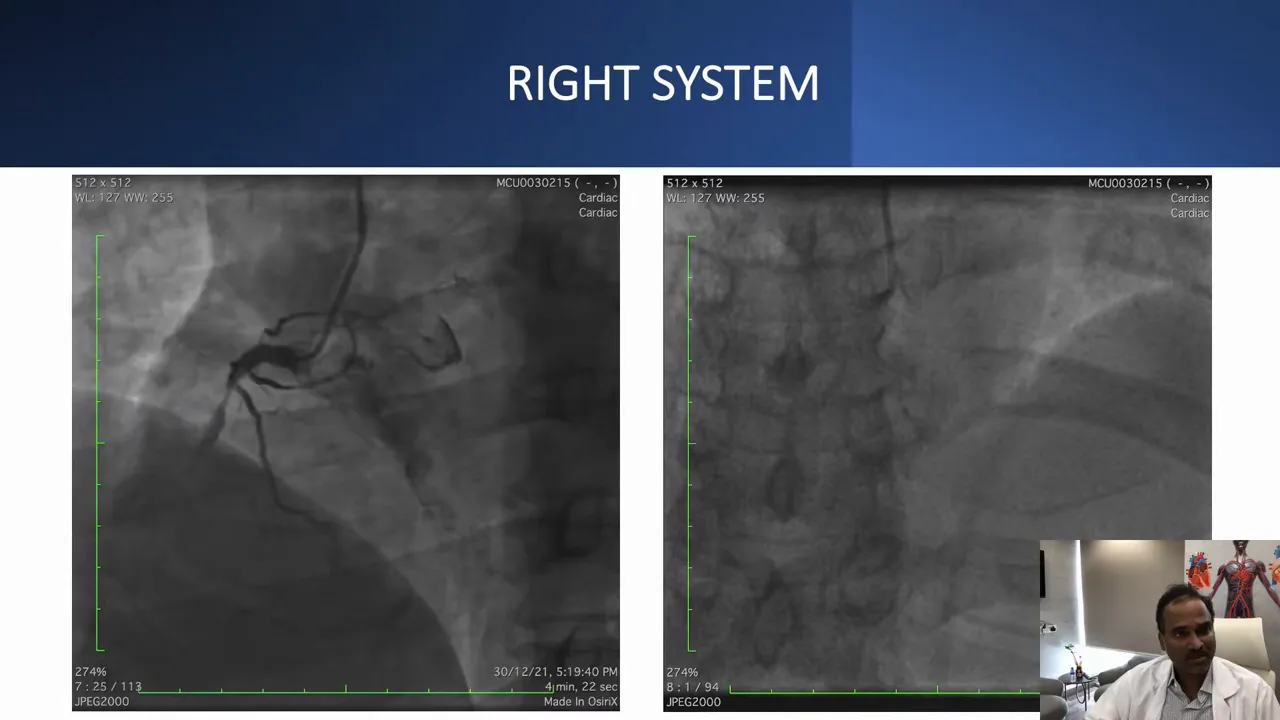
This angiographic projection suggested a short RCA CTO. At first glance the lesion looked straightforward on one projection, but other angiographic angles revealed a more complex course.
Initial anatomic assessment and strategy
Before crossing any CTO it is critical to review three things: the proximal cap, the length and course of the occlusion, and the distal landing zone. In this case:
- Proximal cap was blunt but well defined and amenable to antegrade entry.
- Occlusion length appeared short on some views but hidden angulation made the course unpredictable.
- Distal vessel was healthy, but the collateral that supplied the PDA joined at an obtuse angle with a branch, making retrograde wiring into the true distal RCA challenging.
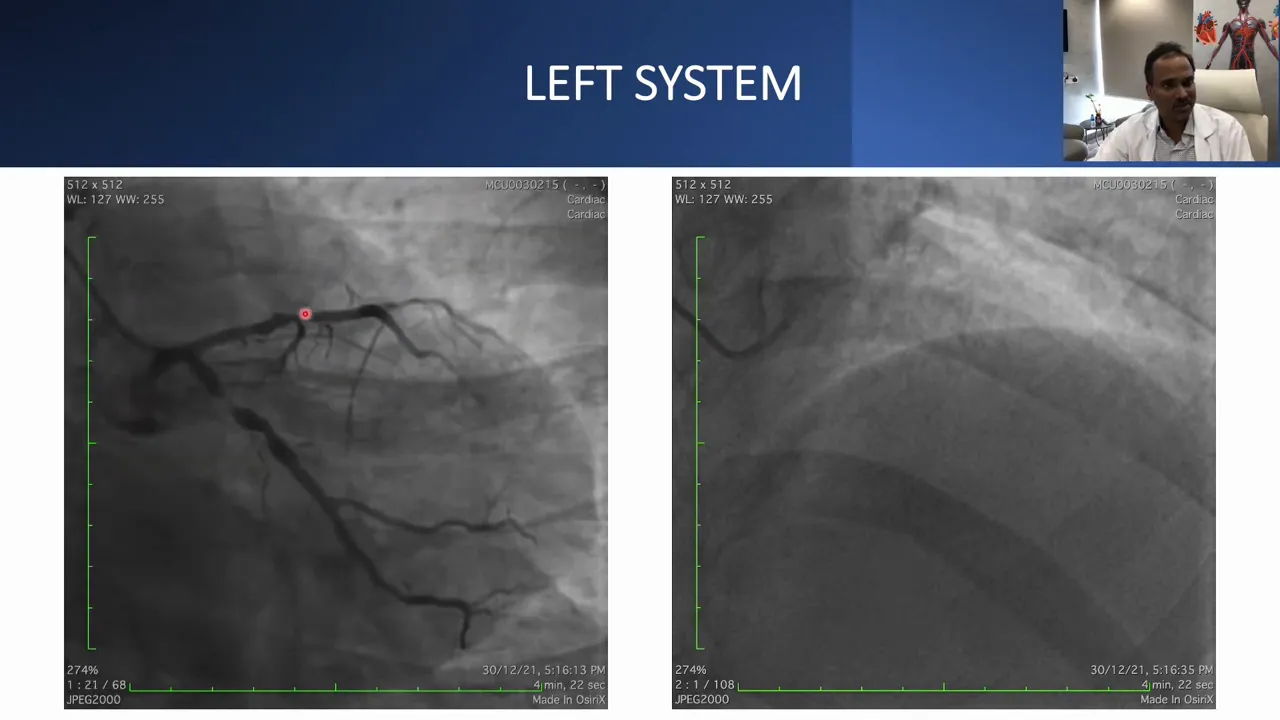
The left coronary system had significant lesions in the LAD and LCX and acted as the donor for collateral supply to the RCA. The plan was to treat the left system first to provide a stable donor circulation, then tackle the RCA.
Why treat the donor vessel first?
Treating the donor vessel (in this case the LAD and LCX) before attempting a complex CTO has several advantages:
- Improved hemodynamic stability during prolonged attempts.
- Better visualization of collaterals after optimized flow in the donor vessel.
- Reduced ischemic risk if the CTO attempt temporarily compromises flow through collaterals.
In this case, the left system was stented with good IVUS-measured lumen areas before proceeding to the RCA.
Antegrade strategy and early escalation
After revascularizing the left system, the RCA CTO attempt began. Dual injection showed a short CTO and two proximal lesions that needed ballooning to avoid getting “stuck” between lesions during antegrade escalation. Lesion preparation with a 2.5 mm balloon opened these proximal stenoses and improved guidewire access to the cap.
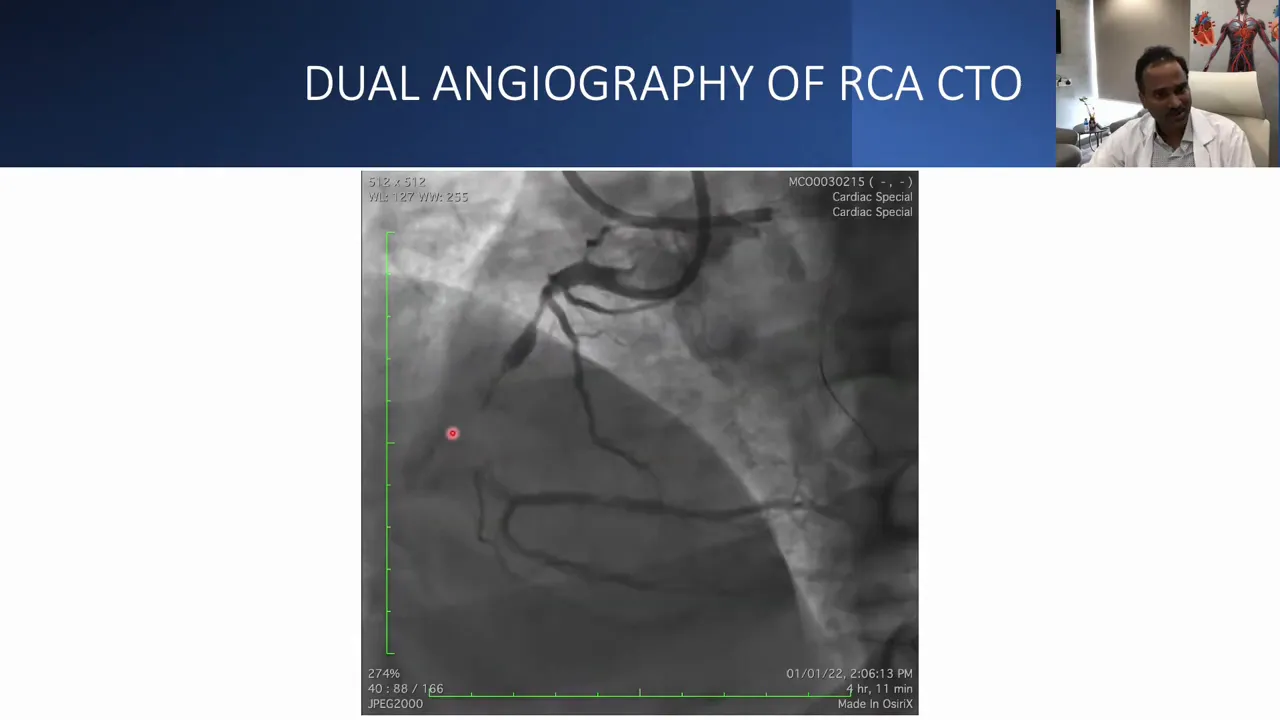
Dual injections help by simultaneously visualizing both proximal and distal segments to understand the exact course of the vessel and the position of the distal cap.
Initial antegrade wiring used a Corsair microcatheter for torque transmission and wire support and a Gaia 2 wire for penetration and control. Gaia wires are excellent for controlled tip load and steerability in fibrous caps. In this case Gaia 2 could not be advanced beyond a certain point, so escalation to Gaia 3 was attempted.
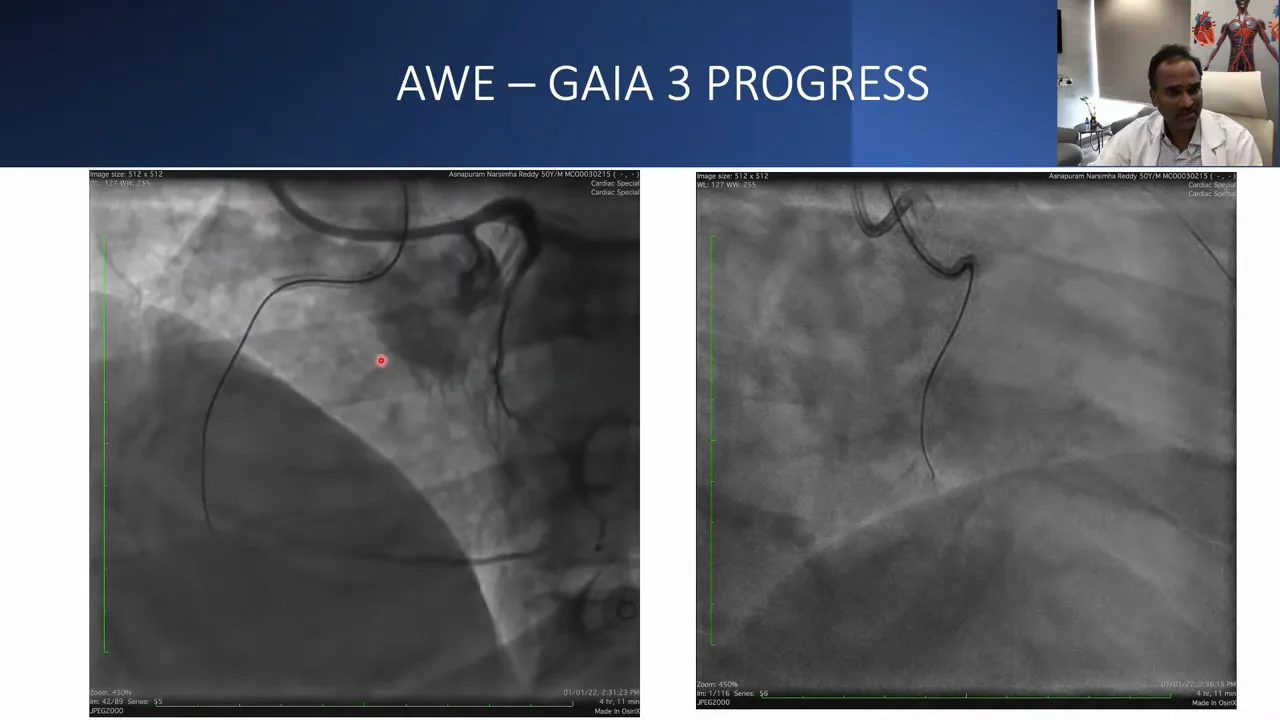
Gaia 3 advanced further but appeared to be exiting the vessel wall on orthogonal views. Wire mobility and position were reviewed in both left anterior oblique and right anterior oblique projections to confirm intraluminal vs extraluminal positions.
When the wire is in the vessel but far from the true lumen
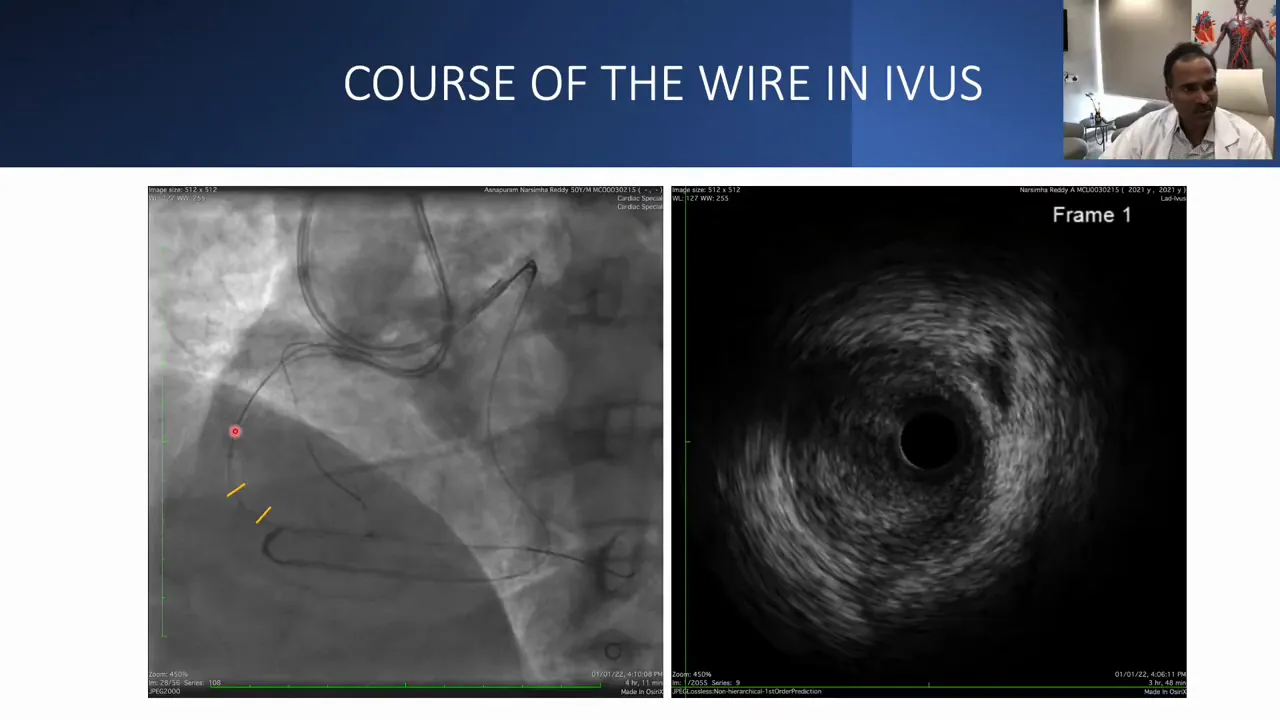
Even when a wire appears to be inside the vessel architecture, distance to the true lumen matters. Here the wire was mobile and appeared intramural on both projections, but it lay more than 1 mm away from the lumen—too far for safe reentry techniques and risky because a major side branch lay nearby. That distance complicates use of targeted reentry devices and increases the chance of side branch loss.
Knuckle technique: when and why
Because stiff wires could not penetrate and a reasonable reentry zone existed proximal to the PDA, a knuckle strategy using a polymer-jacketed Pilot wire was attempted. Knuckling can help follow the vessel path and enlarge a controlled subintimal track before reentry. Microcatheter trapping was used to enhance push support to the knuckling wire.
Despite these attempts, the knuckle did not progress likely due to calcific resistance in the proximal cap—consistent with the initial difficulty in advancing Gaia wires. At that point the team switched to a retrograde approach, primarily to visualize the distal cap more clearly rather than to complete a retrograde crossing.
Retrograde microcatheter injection to unmask the distal cap
When antegrade attempts are limited by ambiguity at the distal cap, selective retrograde microcatheter injection through a septal or epicardial collateral can reveal the true distal cap location and angle. In this case a Corsair (or similar microcatheter) was advanced retrograde through a septal route, and a Sion or similar wire was used to cross the collateral rapidly into the distal RCA territory.
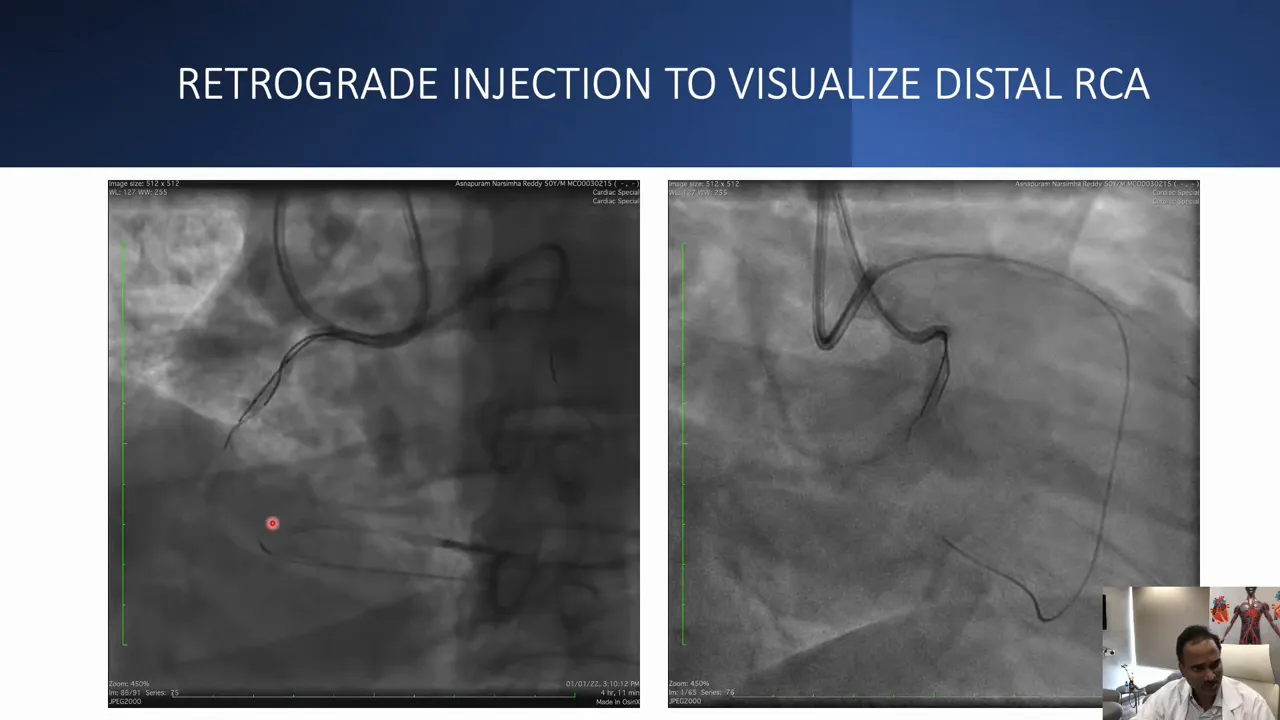
The retrograde microcatheter injection made the distal cap visible—information that was not apparent during a non-selective retrograde injection. With the cap unmasked, it became possible to direct antegrade penetration attempts more precisely.
Integrated antegrade-retrograde strategy
After visualizing the distal cap with a selective retrograde injection, the operator returned to an antegrade approach but used the retrograde microcatheter injections as a directional guide. The Gaia wire could then be steered more accurately toward the distal true lumen.
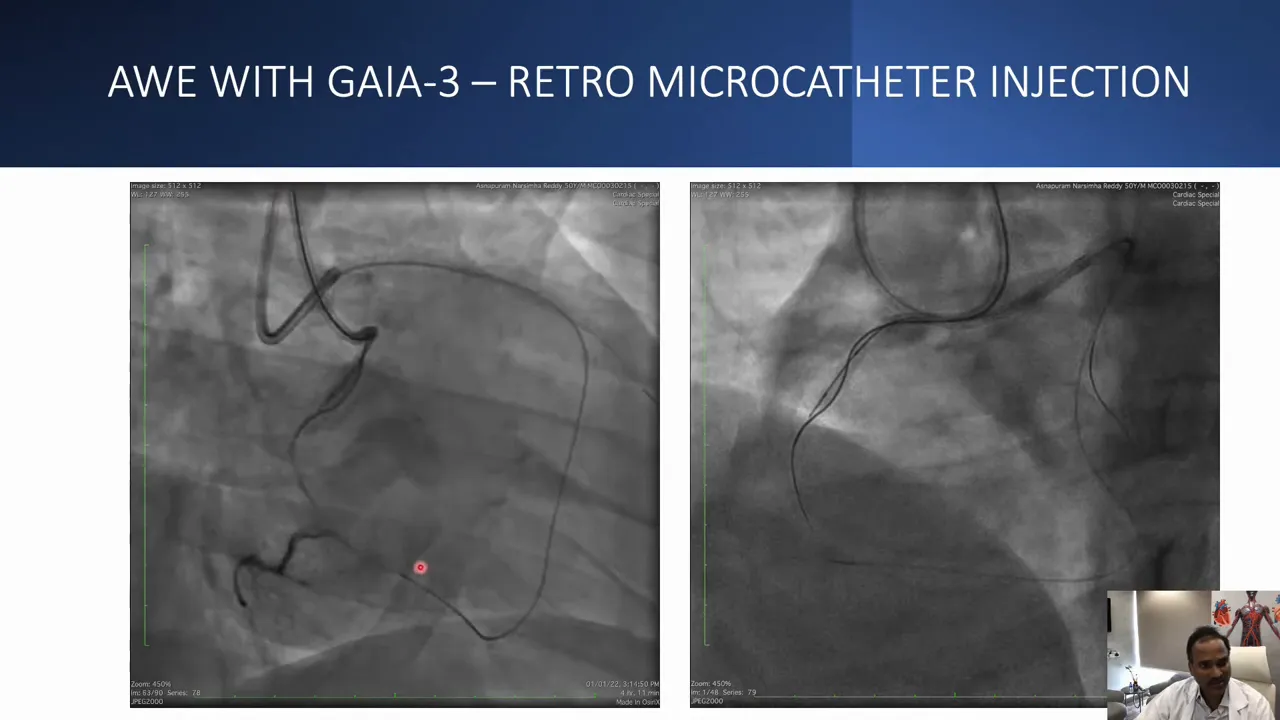
Using orthogonal views—allocranial and allocaudal—was essential to confirm that the retrograde wire and antegrade wire were within the true lumen. These projections eliminate foreshortening and unmask loops, bends, and angulation that otherwise create ambiguity.
Crossing and exchange technique
Pre-dilation with a 1.0 mm balloon was used at the point where the Corsair had become stuck. This small balloon created a channel and allowed exchange to a workhorse wire. The operator identified that a subintimal track had been created and that re-entry into the true lumen occurred prior to the PDA origin—so the PDA was preserved.
After confirming true-lumen position with intravascular ultrasound, the lesion was treated with stenting: a 3.0 x 28 mm stent distally and a 3.5 x 38 mm stent proximally, providing a continuous scaffold across the previously occluded segment.
IVUS-guided optimization
IVUS measurements are pivotal for sizing and optimization. The distal reference lumen area measured about 6.5 mm squared. Stent areas across the treated segment were between approximately 8 and 9.7 mm squared—representing good expansion relative to the reference vessel. IVUS confirmation ensured adequate apposition and minimized the risk of underexpansion and restenosis.
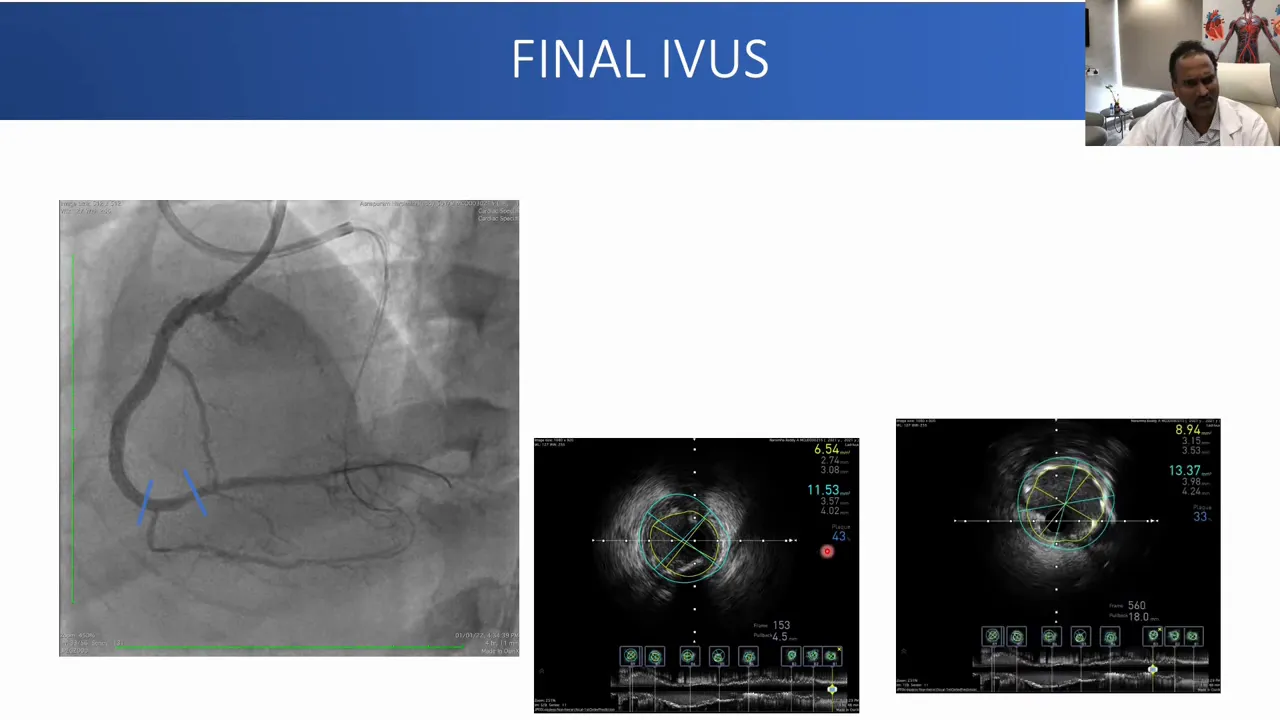
IVUS not only helps with stent sizing but also confirms that important branches such as the PDA remain patent after stent deployment.
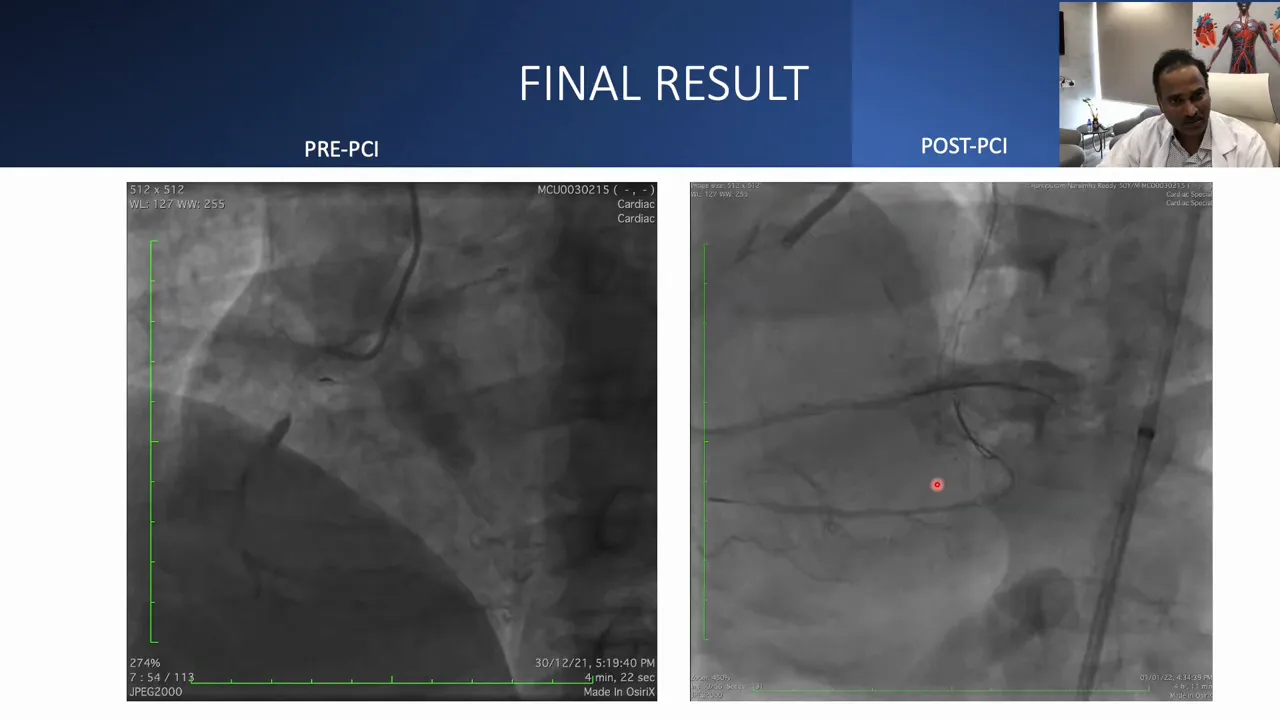
The final angiogram demonstrated preserved PDA flow and an excellent angiographic result.
Understanding misleading angiographic courses
One recurrent theme is that RCA anatomy can be deceptive. A vessel that seems straight in a right anterior oblique projection may reveal multiple loops in a left anterior oblique or level view. These loops and funny bends create wire ambiguity during both antegrade and retrograde attempts.
Always choose projections that best reveal loops and tortuosity before starting wiring. For many RCA CTOs, a level view can show multiple loops that are invisible in an oblique projection.
Key takeaways and procedural pearls
- Mental 3D mapping is essential. Do not rely on a single projection. Use orthogonal views to understand loops and angulation.
- Treat donor vessel first. Revascularizing donor arteries improves collateral flow and safety during CTO attempts.
- Balloon proximal stenoses. Open or dilute proximal lesions before antegrade escalation to avoid being trapped between lesions.
- Use selective retrograde microcatheter injection to reveal the distal cap. This can change your antegrade puncture site and angle and convert a failed antegrade attempt into a success.
- Wire selection matters. In ambiguous courses start escalation using polymer-jacketed wires (pilot or Fielder family) for trackability, then use Gaia wires to penetrate once a path is made. The “pilot-first, Gaia-second” or “pilot to create a channel then Gaia to cross” approach is often useful.
- Knuckle technique is helpful but not universal. Useful when a controlled subintimal track is acceptable, but calcified proximal caps can prevent knuckle progression.
- IVUS guides optimization. Use intravascular ultrasound to confirm true lumen re-entry, assess stent expansion, and protect important side branches such as the PDA.
- CT overlay can help. When ambiguity persists, CT overlay may provide additional 3D orientation for antegrade wiring.
Recommended antegrade wire escalation algorithm for ambiguous RCA CTO
- Start with a polymer-jacketed, low-tip-load wire (pilot/Fielder) to probe and create a track when course is uncertain.
- Advance a microcatheter (Corsair or similar) for support and torque transfer.
- If resistance persists, escalate to a mid-tip-load wire such as Gaia 2 for controlled penetration.
- Use Gaia 3 or high-tip-load wire only if path is confirmed and calcification is not preventing progression.
- If wire appears intramural but far from true lumen, consider knuckle or retrograde visualization to guide reentry.
- Always confirm position in multiple orthogonal projections and with IVUS when possible.
Common pitfalls
- Relying on a single projection, especially in the RCA where loops are common.
- Failing to treat proximal lesions first, which can trap the operator mid-course.
- Escalating to stiff penetration wires without establishing a safe reentry zone.
- Not using selective retrograde microcatheter injections when the distal cap is ambiguous.
- Skipping IVUS confirmation after crossing and stenting—this may leave underexpanded or malapposed stents undetected.
Examples of confusing RCA courses
Below are angiographic patterns that frequently cause confusion during integrated antegrade-retrograde attempts:
- Apparent straight vessels on RAO that reveal multiple loops on left anterior oblique.
- Acute bends or “bands” in the mid RCA that challenge torque transmission.
- Collateral takeoffs that join the PDA at an obtuse angle, steering retrograde wires away from the distal true lumen.
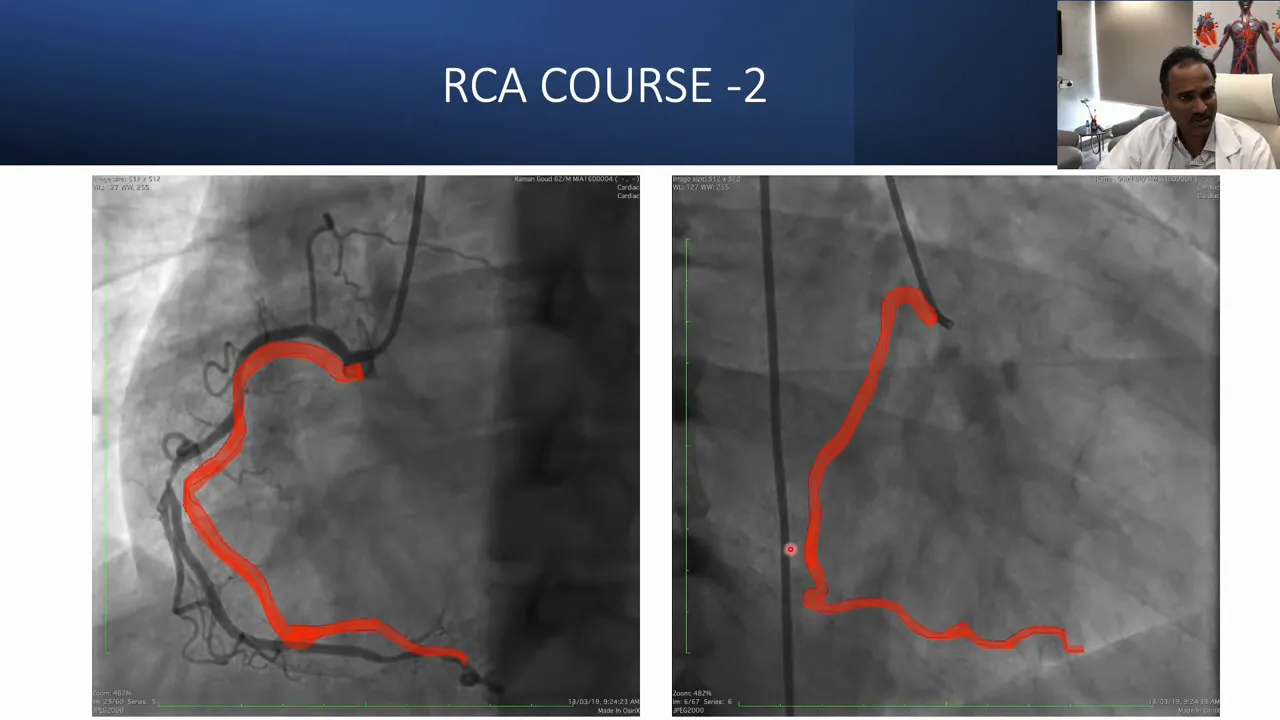
Identify these patterns before the first wire attempt to reduce wasted time and prevent unnecessary subintimal dissection.
Conclusion
Successful CTO PCI is as much an exercise in imaging and planning as it is in technique. This case demonstrates how combining multivessel PCI with IVUS guidance, treating the donor vessel first, careful antegrade wire escalation, and selective retrograde injections can resolve distal cap ambiguity and preserve critical branches such as the PDA. When confronted with a short RCA CTO that looks simple but behaves otherwise, pause, obtain additional projections, consider selective retrograde microcatheter injection, and use IVUS to guide your final result.
When should I treat the donor vessel before attempting the CTO?
Treat the donor vessel when it supplies significant collaterals to the CTO territory or when treating it improves hemodynamics and visualization. Treating the donor first reduces ischemic risk during prolonged CTO work and can make collateral mapping clearer.
How does a selective retrograde microcatheter injection help?
Selective retrograde microcatheter injection opacifies the distal cap and landing zone precisely. This unmasking often reveals the true cap location and angle, converting an ambiguous antegrade target into a clear one for controlled penetration.
When should I use a knuckle wire?
Use a knuckle technique when creating a controlled subintimal track is acceptable and a safe reentry zone exists proximal to important branches. Avoid knuckling if heavy calcification blocks progression or if the reentry zone is too small or too distal.
Which wires should I use in ambiguous courses?
Start with a polymer-jacketed, low-tip-load wire such as a pilot or Fielder to create a track. Once a track is established, use GaIa series wires (Gaia 2, Gaia 3) for controlled penetration. The pilot-first, Gaia-second tactic balances trackability and penetration.
How essential is IVUS in CTO PCI?
IVUS is very helpful. It confirms true lumen position, informs stent sizing, detects underexpansion or malapposition, and helps protect branch vessels. In ambiguous re-entry situations it provides confirmation that the wire re-entered the true lumen before committing to stenting.
Does CT overlay always solve angiographic ambiguity?
CT overlay can provide valuable 3D guidance in complicated anatomies and may reduce ambiguity, but it is not always available. When available and fused properly, it can direct antegrade puncture and reduce contrast and radiation use.


No Comments