07 Jul IVUS Guided Cap Puncture (Ambiguous Cap): A Comprehensive Guide by Dr. Sharath Reddy Annam
In the intricate world of interventional cardiology, mastering the technique of cap puncture during chronic total occlusion (CTO) interventions is crucial. Dr. Sharath Reddy Annam, in his detailed live lecture, sheds light on the nuances of IVUS guided cap puncture—especially when dealing with ambiguous proximal caps. This article distills his expert insights, providing a step-by-step guide to understanding, identifying, and safely wiring ambiguous proximal caps using intravascular ultrasound (IVUS) guidance.
Whether you are a seasoned interventional cardiologist or a trainee eager to deepen your understanding of CTO interventions, this article will walk you through everything from prerequisites to advanced wiring strategies, based on Dr. Sharath Reddy’s methodical approach.
Understanding the Importance of IVUS Guided Cap Puncture
The starting point for any CTO intervention is assessing the proximal cap. In many cases, the proximal cap can be ambiguous, making it difficult to determine the precise entry point for the guidewire. Dr. Sharath emphasizes that if the proximal cap is ambiguous, it is imperative to make it unambiguous by employing imaging techniques—primarily IVUS.
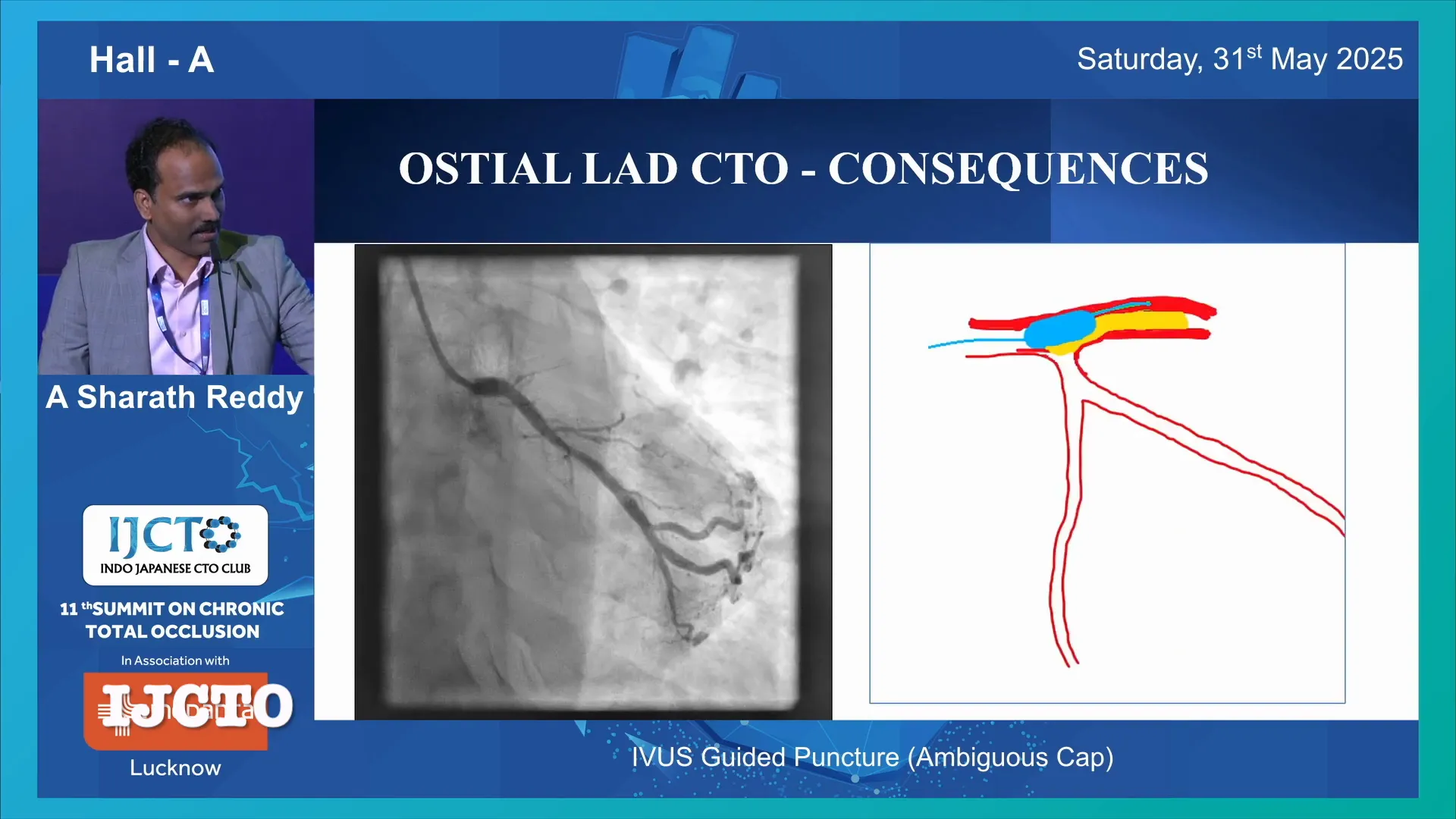
Why is this important? If cap puncture is attempted without proper imaging guidance, several complications can arise:
- Subintimal wiring can lead to lifting a flap and inadvertently closing a side branch such as the left circumflex artery (LCX), which can cause an on-table catastrophe.
- Going retrograde without adequate antegrade preparation may result in similar complications.
- Performing an extended reverse controlled antegrade and retrograde subintimal tracking (CART) technique, especially in cases with significant side branches, is contraindicated.
Therefore, the safest and most appropriate approach in ambiguous cap cases is to first perform an IVUS guided cap puncture. If the distal lumen is reached successfully, the procedure can proceed antegrade; if not, a retrograde approach can be employed to complete the case.
Prerequisites for IVUS Guided Cap Puncture
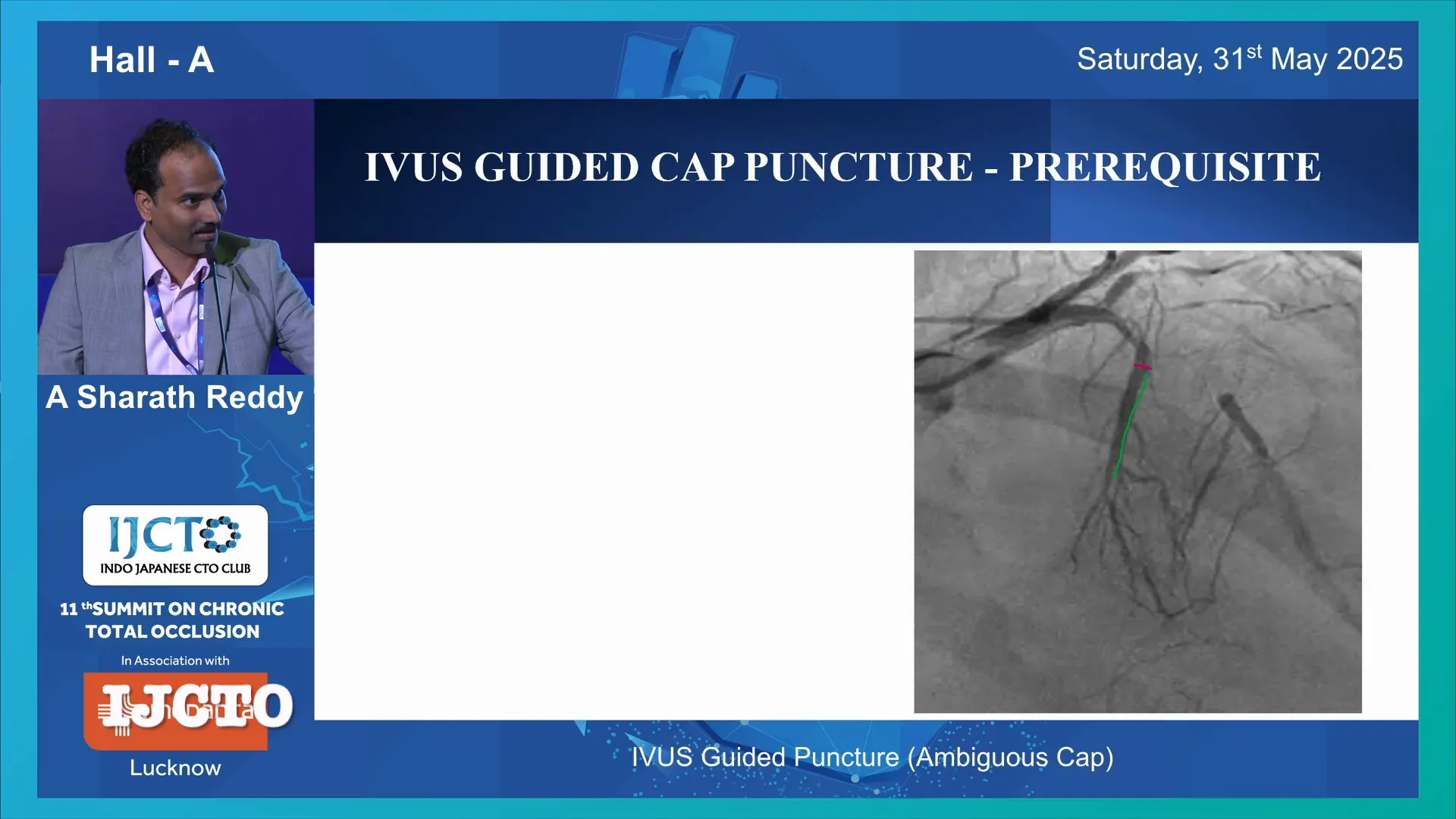
Before diving into the procedure, certain anatomical and technical prerequisites must be met to ensure successful IVUS guided puncture:
- Presence of a Suitable Side Branch: A good-sized side branch with sufficient length is essential. This branch acts as the conduit for the IVUS catheter.
- Side Branch Length: The length of the side branch must be longer than the tip-to-transducer distance of the IVUS catheter being used. For example, the Boston Scientific IVUS catheter requires approximately 20 mm, while the Terumo Avant catheter requires around 9 mm (though this is not widely available in India).
- Angulation: The angulation between the side branch and the main vessel should ideally be less than 60 degrees. More severe angulation impairs imaging quality and catheter navigation.
- Side Branch Tortuosity: Even if the size is adequate, tortuous branches pose challenges in advancing the IVUS catheter and performing precise imaging.
If these criteria are not met, IVUS guided cap puncture becomes significantly more difficult or impossible, necessitating alternative strategies.
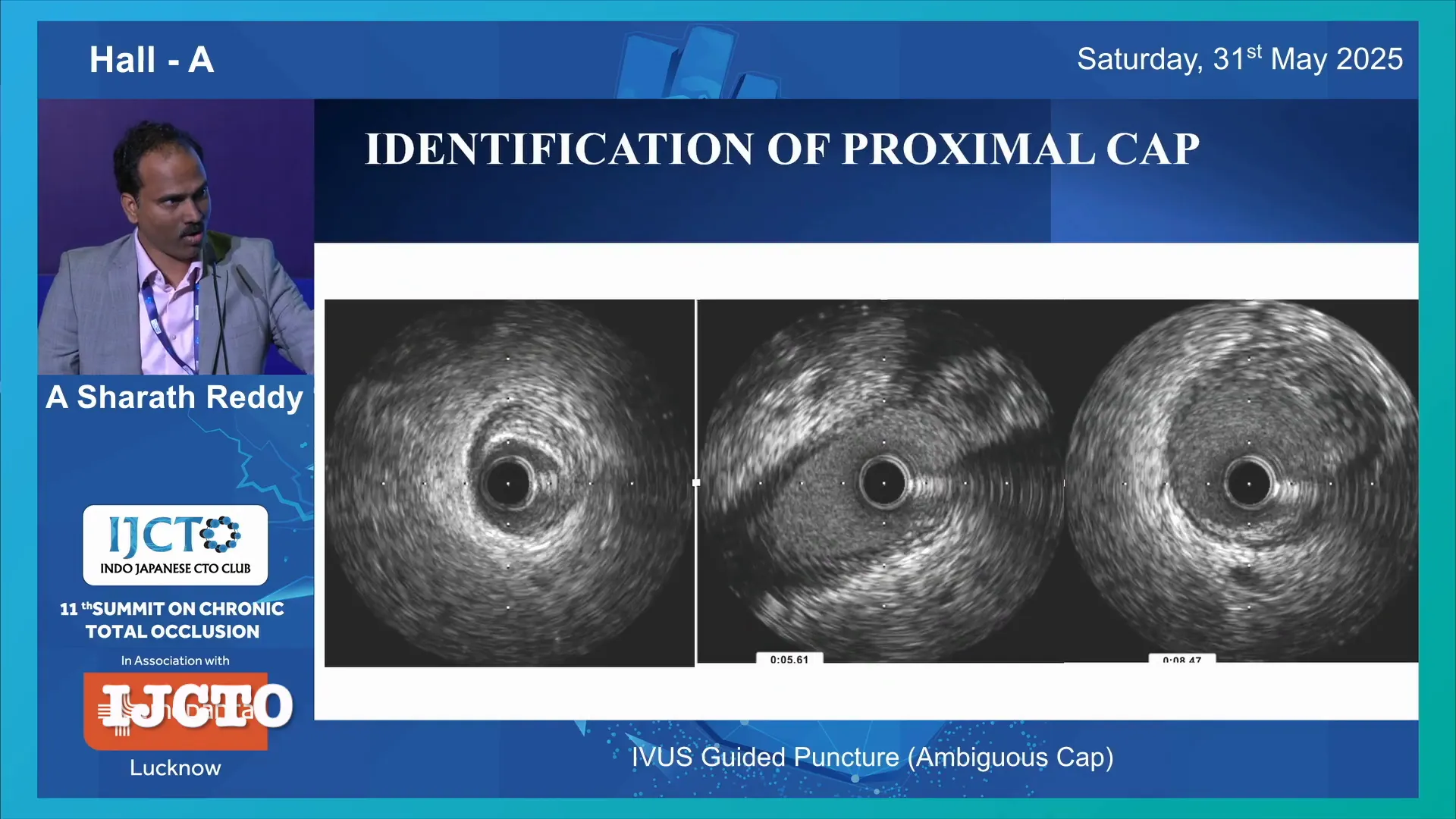
Step 1: Identification of the Proximal Cap Using IVUS
Once the IVUS catheter is positioned in the side branch, the next critical step is to accurately identify the proximal cap. Dr. Sharath explains that this is done by carefully analyzing the IVUS images with attention to two key markers:
- Disappearance of the Media Layer: The media layer of the vessel wall disappears at the site of the occlusion, marking the cap location.
- Jump in Vessel Size: There is a noticeable increase in the vessel diameter distal to the occlusion, which helps localize where the cap ends and the distal lumen begins.
On the IVUS image, the proximal cap often appears as a confluence point where the vessel narrows or the media layer is disrupted. Dr. Sharath points out that the presence of side branches and heavy calcification can obscure these markers, making the identification more challenging.
In cases with unfavorable anatomy—such as calcified or severely angulated side branches—IVUS imaging may be less reliable, requiring heightened operator experience and alternative imaging strategies.
Step 2: Wiring the Proximal Cap
After confirming the proximal cap location, the next step is to wire the cap safely and effectively. Dr. Sharath discusses several important considerations during this phase:
Choosing the Appropriate Equipment
- Guide Catheters: A 7 French system can accommodate IVUS catheters like the Finecross, while the Opticross HD6 catheter requires a 6 French compatible system. Using the right system ensures smooth catheter manipulation.
- Microcatheters: Devices like Corsair are used in 8 French systems to support guidewire advancement.
- Wiring Techniques: Operators can employ 3D wiring, tip detection wiring, or simple wire positioning guided by IVUS.
Choosing the Right Guidewire
Dr. Sharath compares different guidewires based on their tip bend stiffness and behavior when pushed against the cap:
- Gaia Wire: Has less tip bend stiffness, meaning it tends to bend on pushing.
- Haret or Conquest Pro Wire: Exhibits higher tip bend stiffness and is better for penetrating ambiguous caps.
The key takeaway is that a stiffer tip wire is preferable for initially entering the cap, but it is not advisable to use a stiff wire for further advancement beyond the cap to avoid vessel injury.
Optimizing Wire Shape
The shape of the wire tip is crucial. Dr. Sharath recommends a primary curve of about 1 mm and a secondary curve tailored to match the angle of attack at the cap. This customization facilitates precise wiring and reduces the risk of subintimal passage.
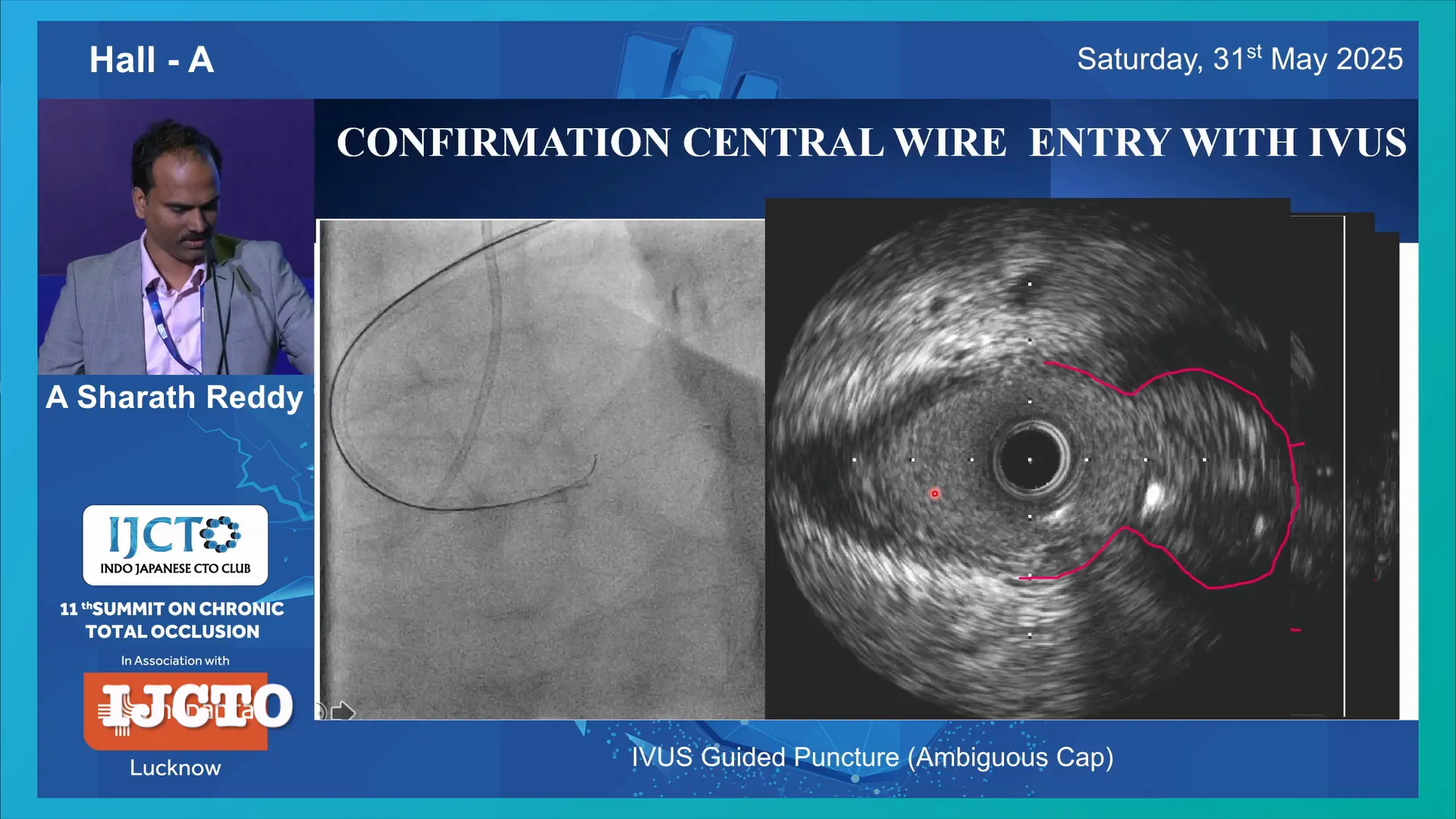
Confirming Wire Position
Once the wire is advanced, it is essential to confirm its central position within the media layer using IVUS. The wire must be within the vessel media in all angiographic views. At vascular confluences, the wire should lie between the “goalposts” formed by the media layer of adjacent branches.
Failing to confirm wire position can lead to subintimal wiring and procedural complications. Dr. Sharath highlights a case where the first wire was suboptimal and could have led to catastrophe if continued, emphasizing the importance of IVUS confirmation and rewiring if necessary.
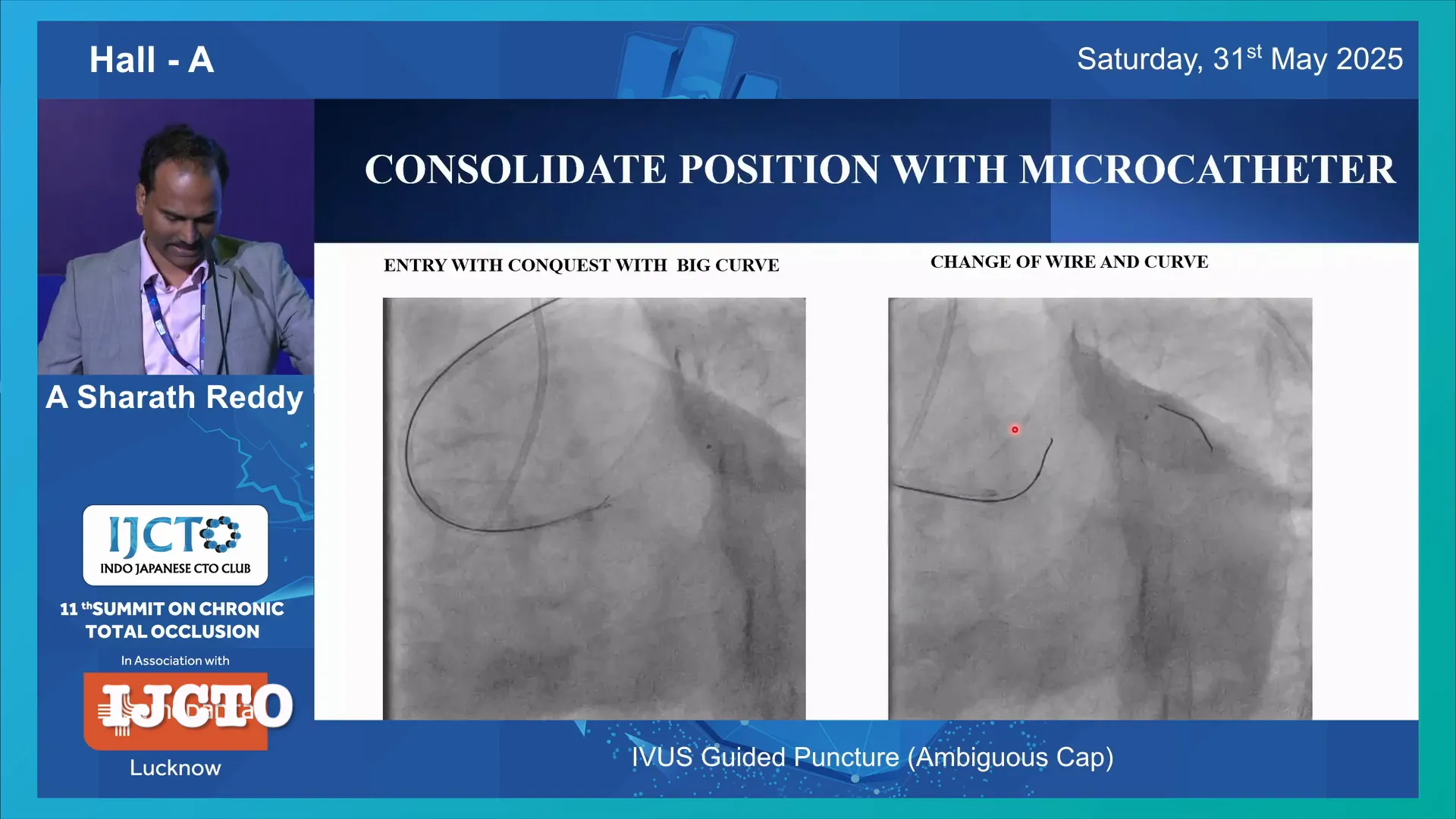
Step 3: Securing and Downgrading the Wire
After successful cap puncture with a stiff wire (such as Conquest), Dr. Sharath advises securing the wire position by advancing a microcatheter over it. This consolidation prevents inadvertent wire movement or vessel injury.
Following this, the wire should be downgraded or de-escalated to a softer wire with a 1 mm tip, like the Gaia or another preferred wire. The softer wire is then advanced further to navigate the CTO segment safely.
This step protects the vessel from damage caused by stiff wires and facilitates smoother tracking through the occlusion.
Step 4: Managing Complex Cases and Alternative Approaches
Sometimes, IVUS guided antegrade cap puncture is not feasible due to extreme angulation or other anatomical challenges. In such cases, Dr. Sharath recommends the following strategies:
- Retrograde Approach: Insert an IVUS catheter into the side branch and attempt a retrograde puncture of the proximal cap.
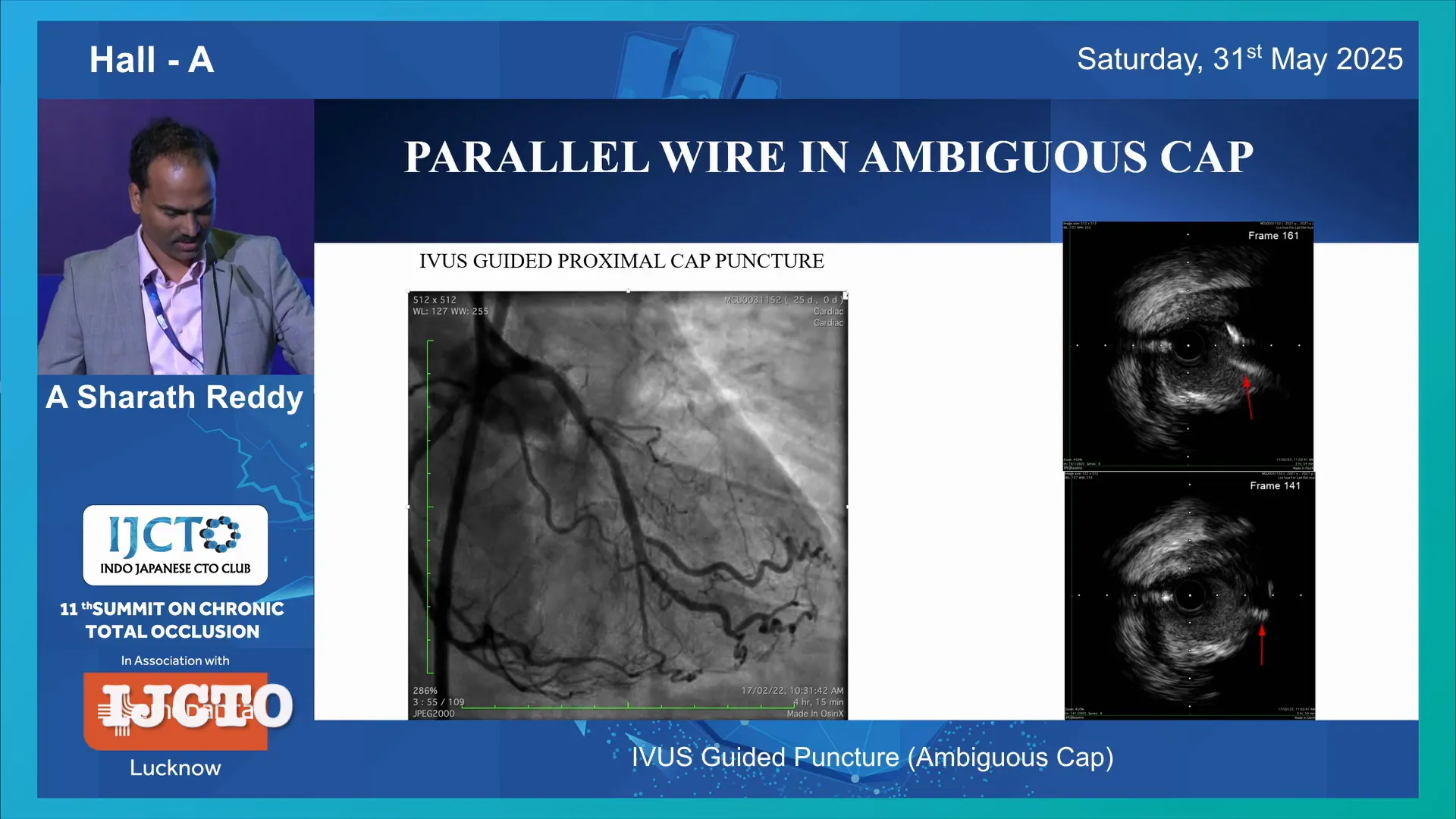
- Parallel Wiring: After confirming the first wire’s position, create a space and advance a second wire parallel to the first. This technique helps navigate through difficult occlusions while preserving side branches.
- Reverse CART: Use this technique cautiously, ensuring that the dissection plane does not extend into significant side branches like the ostium of the LCX.
Dr. Sharath stresses that even with IVUS guidance, success is not guaranteed, and operators must be prepared to adapt their strategy based on real-time imaging and wire behavior.
Additional Technical Tips and Pearls
- Slipstream System: When using a dual-lumen catheter over the same wire on which IVUS is performed, carefully pull the wire back to free the IVUS catheter, allowing its removal without disturbing the working wire.
- Preserving Side Branches: Eccentric wire entry near the carina can lead to side branch occlusion. Careful IVUS visualization helps avoid this by guiding central wire positioning.
- Catheter Compatibility: Choosing compatible catheter sizes and systems (6F, 7F, 8F) is crucial for smooth device exchanges and minimizing vessel trauma.
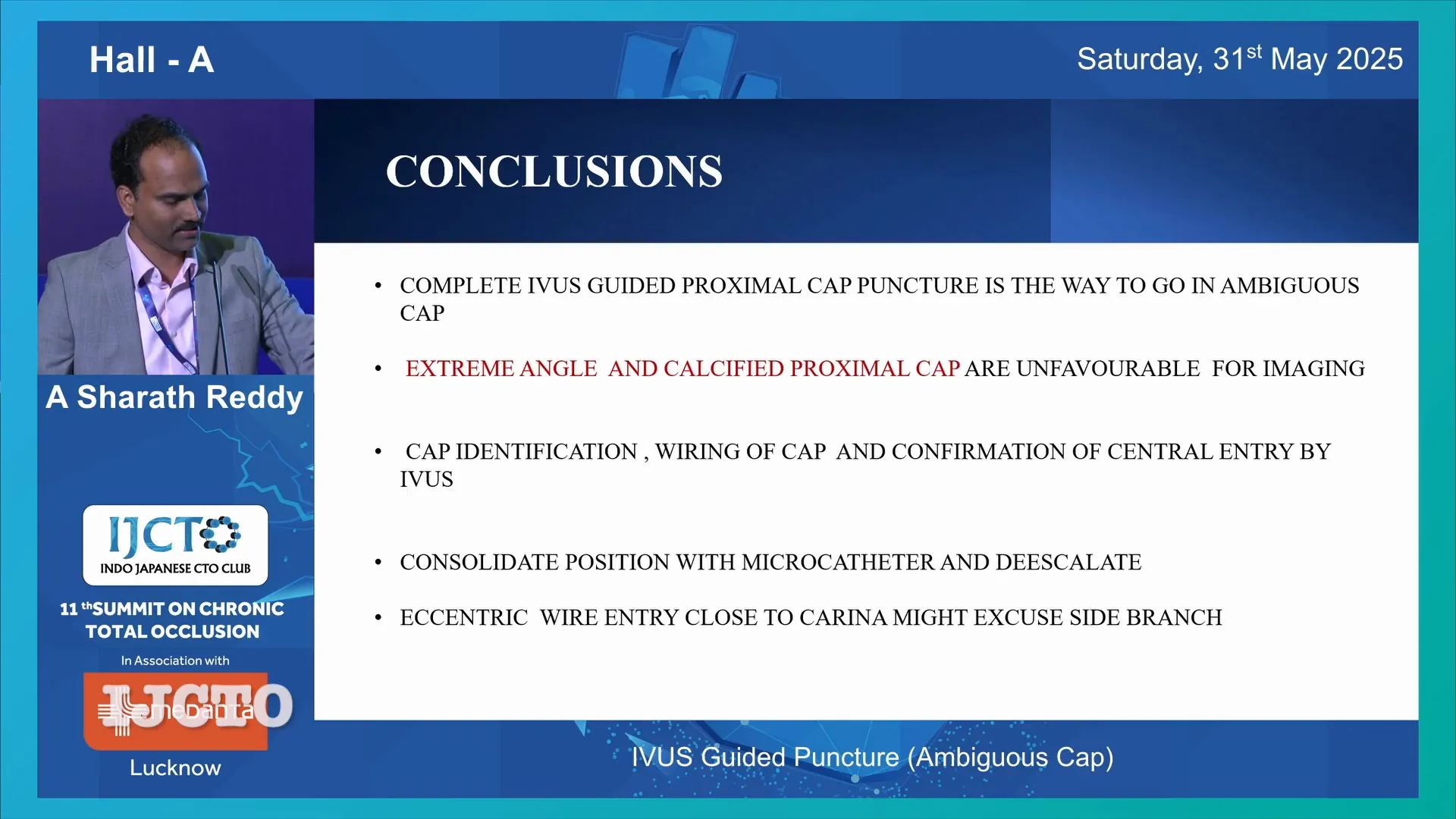
Conclusion: The Way Forward with IVUS Guided Cap Puncture
Dr. Sharath Reddy Annam’s methodical approach to IVUS guided proximal cap puncture is a valuable advancement in CTO interventions, especially for ambiguous caps. The technique enhances safety by enabling precise cap localization, central wire entry, and preservation of side branches.
Key points to remember include:
- Ensure the presence of a suitable side branch with adequate length and favorable angulation for IVUS catheter placement.
- Identify the proximal cap by noting the disappearance of the media and jump in vessel size on IVUS.
- Use appropriate wiring techniques with stiff tip wires for initial cap entry, followed by de-escalation to softer wires for further advancement.
- Confirm wire position within the media in all views to prevent subintimal wiring and complications.
- Secure wire position with microcatheters and be ready to use alternative approaches like retrograde puncture or parallel wiring when antegrade IVUS guided puncture is not feasible.
While IVUS imaging may be limited in cases of extreme angulation or heavy calcification, careful planning and technical expertise can overcome many challenges. This technique represents a significant step forward in the safe and effective management of complex CTO lesions.
Frequently Asked Questions (FAQ)
Q1: Why is IVUS guidance necessary for ambiguous proximal caps?
IVUS helps visualize the vessel wall layers and occlusion site, allowing precise localization of the proximal cap. This reduces the risk of subintimal wiring and complications such as side branch occlusion or vessel dissection.
Q2: What are the anatomical prerequisites for IVUS guided cap puncture?
A good-sized side branch with a length exceeding the catheter’s tip-to-transducer distance and an angulation of less than 60 degrees are essential for proper IVUS catheter placement and imaging.
Q3: Which guidewire is preferred for puncturing the ambiguous cap?
Wires with higher tip bend stiffness, such as the Haret or Conquest Pro, are preferred for initial cap puncture. After entry, the wire should be downgraded to a softer wire like Gaia for safer advancement.
Q4: How do I confirm the correct wire position during the procedure?
Use IVUS imaging to ensure the wire is centrally located within the media layer of the vessel in all angiographic views. The wire should lie between the media layers, especially at confluences, to avoid subintimal passage.
Q5: What if IVUS guided antegrade cap puncture is not possible?
Alternative strategies include attempting retrograde cap puncture using IVUS guidance, parallel wiring techniques, or cautiously performing reverse CART beyond significant side branches.
Q6: How can side branches be preserved during wiring?
Central wire positioning confirmed by IVUS helps avoid eccentric entry near the carina, which can jeopardize side branches. Parallel wiring also aids in preserving important branches.
Q7: What are common pitfalls to avoid during IVUS guided cap puncture?
Avoid advancing stiff wires without consolidation by microcatheters, prevent subintimal wiring by confirming wire position, and be cautious of extended dissections near major side branches.
By understanding and applying these principles, interventional cardiologists can enhance their success rates and patient safety during challenging CTO procedures.


No Comments