08 Oct Imaging Guided Double Bifurcation PCI
n this blog, we delve into a complex live case of imaging-guided double bifurcation percutaneous coronary intervention (PCI) performed by Dr. Sharath Reddy Annam. The case focuses on a 45-year-old patient with significant coronary artery disease, showcasing the systematic analysis of intravascular ultrasound (IVUS) images to inform stenting strategies.
Table of Contents
Anatomical Considerations and Initial Questions
Understanding the anatomy of the coronary arteries is crucial for effective intervention. In this case, we observe a proximal lesion accompanied by significant calcification. The imaging reveals both medial and deep calcification, which can complicate treatment strategies.
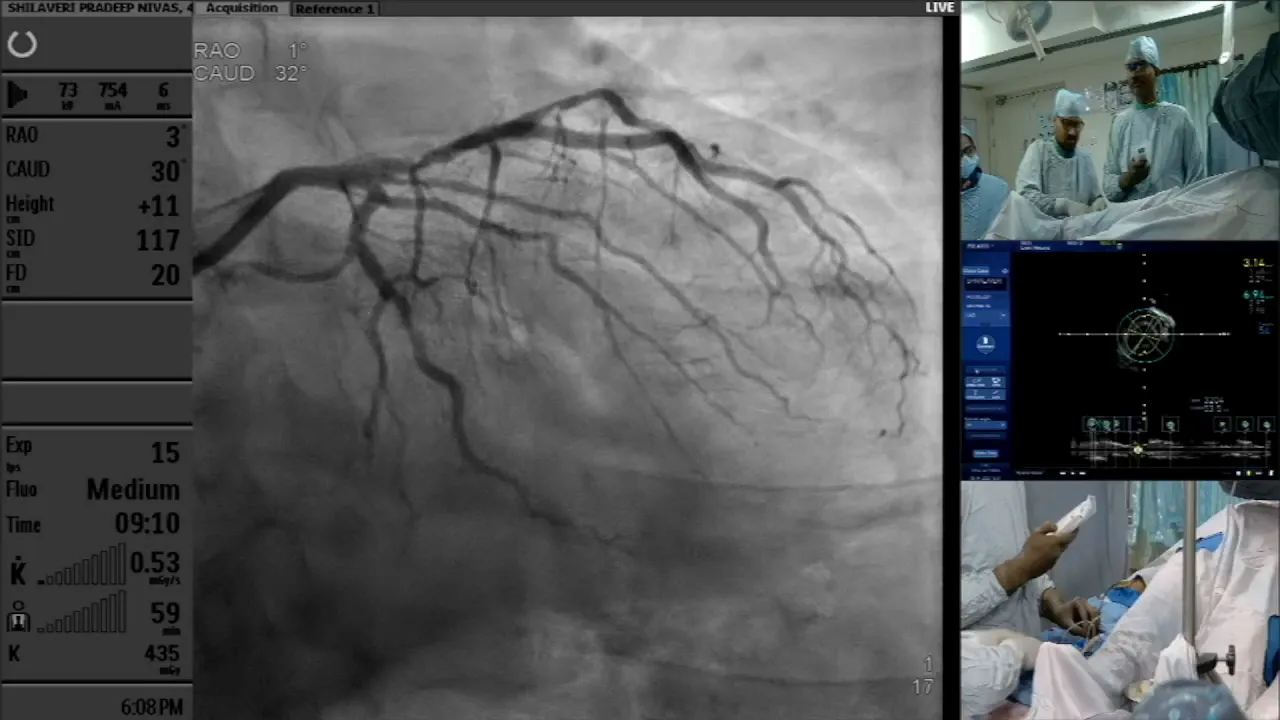
As we analyze the lesions present, we raise several critical questions. Firstly, identifying the distal reference point is essential for determining the landing zone in the left anterior descending artery (LAD). Additionally, we must consider the approach for the ostial diagonal artery. Should we protect the ostial diagonal or proceed with a provisional stenting strategy?
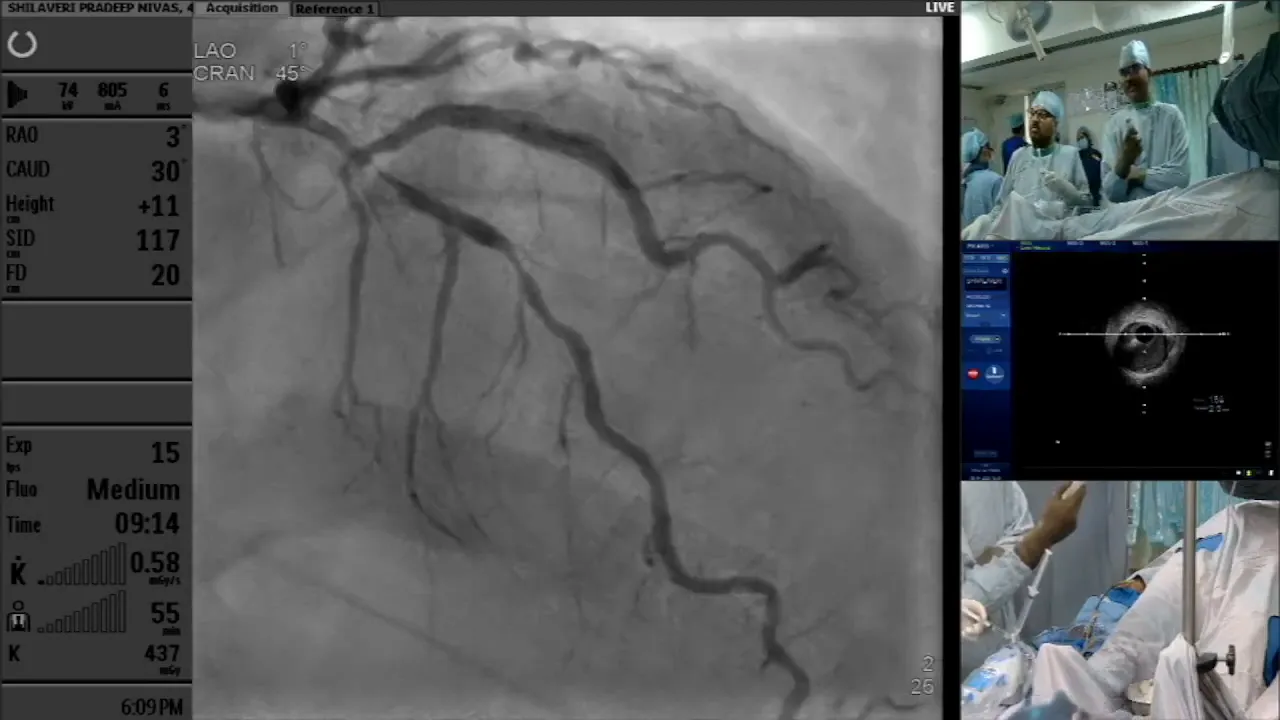
Another vital query revolves around the proximal ostium. Can we successfully land a stent in the LAD? We need to analyze the minimum lumen area (MLA) and assess if there is any plaque extension into the left main coronary artery (LMCA). These questions guide our imaging efforts and strategy development.

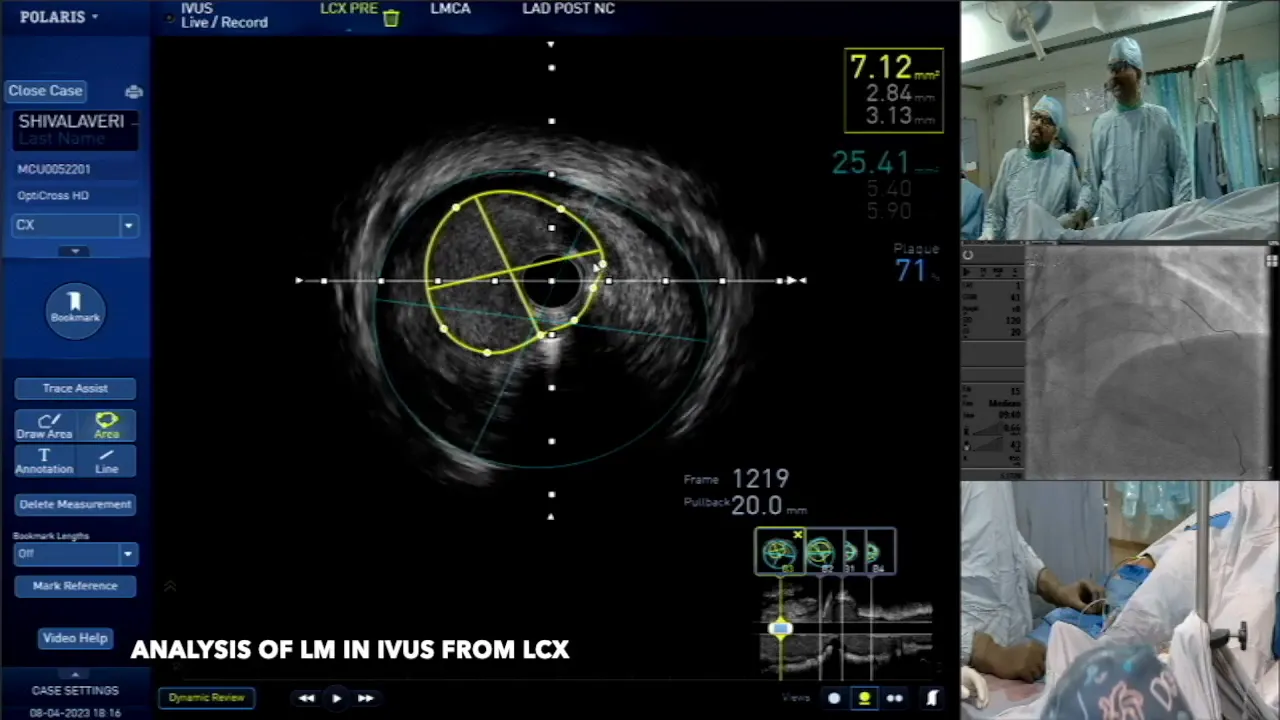
Analyzing the LCX with IVUS
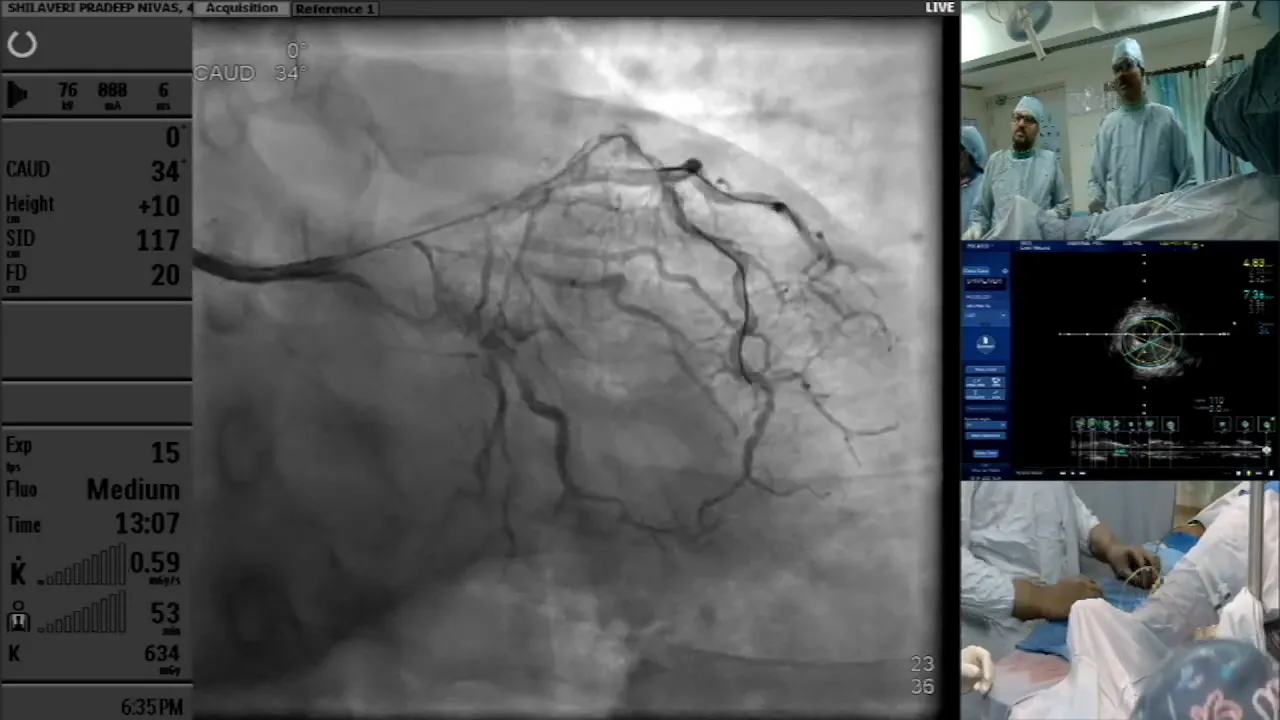
To begin answering these questions, we first analyze the left circumflex artery (LCX) using intravascular ultrasound (IVUS). This imaging technique allows us to visualize the anatomy and pathology within the artery effectively.

As we pull back through the LCX, we observe a branch joining at approximately the 2 o’clock position. This is crucial for understanding the relationship between the LCX and the LAD. Identifying these branches helps in planning the intervention and determining the best approach for stenting.
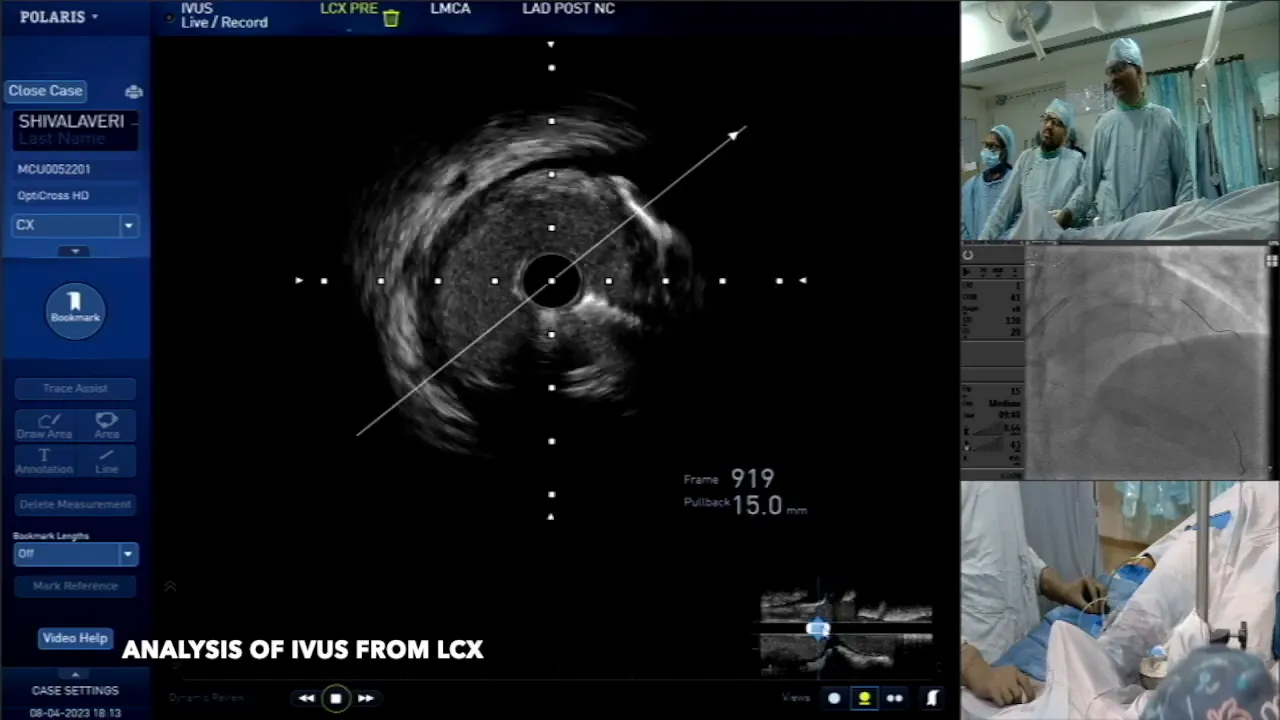
The hosal LCX area measures approximately 7.6 mm², with a plaque area of 38%. Given this lumen area, there is typically no need for protective measures on the LCX, allowing us to focus on the diagonal artery while planning the intervention.
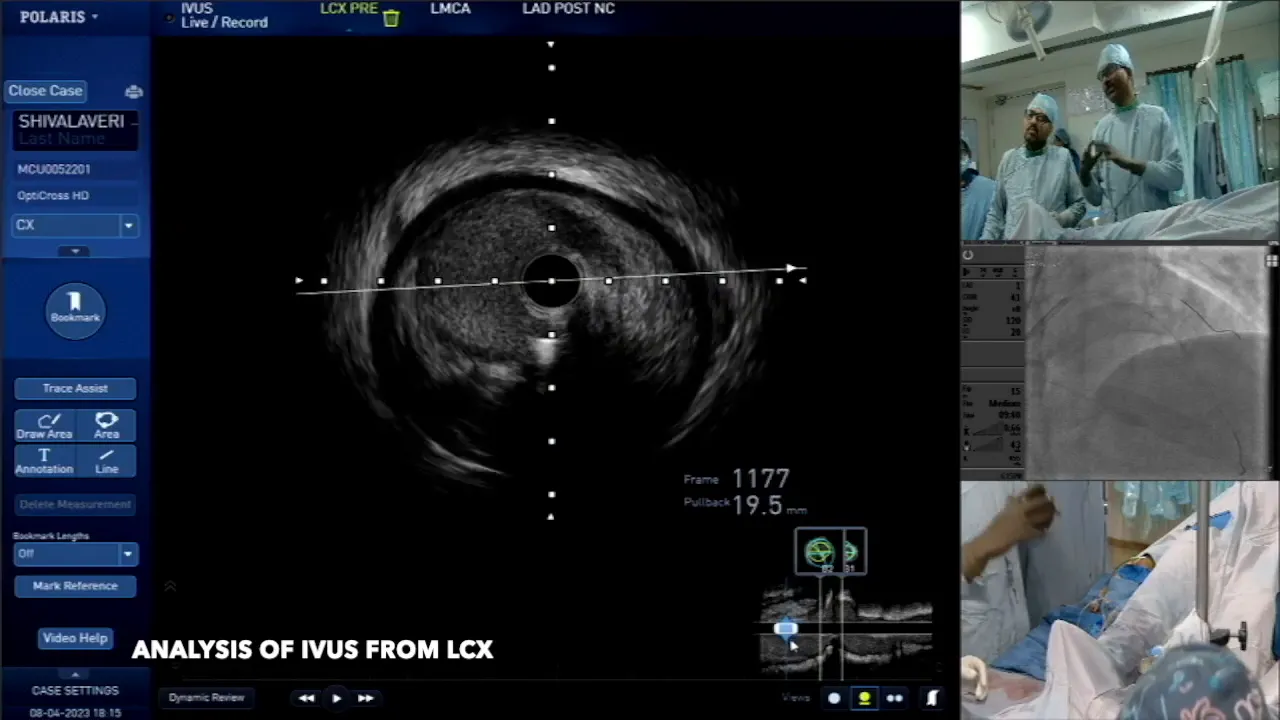
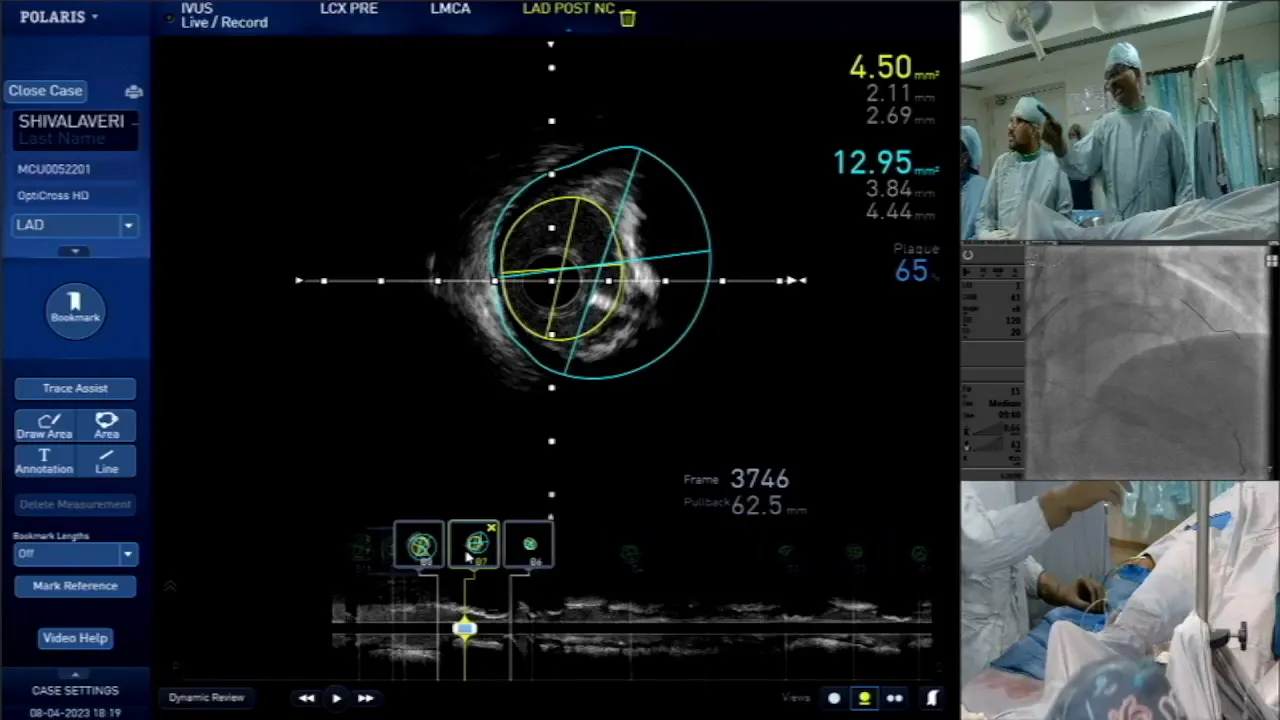
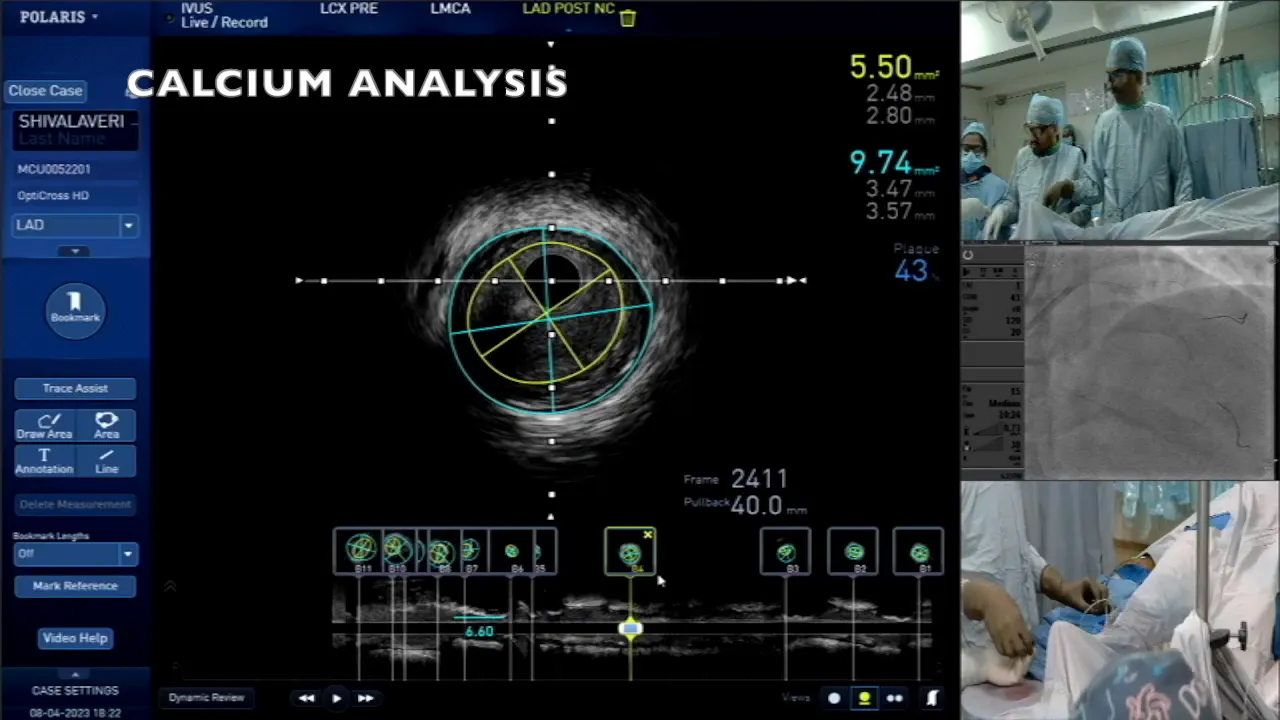
Assessing the MLA and Proximal Lesion in LED
Next, we shift our focus to the LAD. The MLA observed from the LCX is around 6.9 mm², indicating a plaque area of 72%. This suggests that we need to evaluate the LAD’s proximal lesion closely before making any decisions regarding stenting.
Switching to the LAD IVUS, we discover an MLA ranging from 7.4 to 9.9 mm². These measurements are critical as they inform whether intervention is necessary. If the MLA is beyond 6 mm², it may not warrant treatment, but the extent of plaque in the LMCA must also be considered.

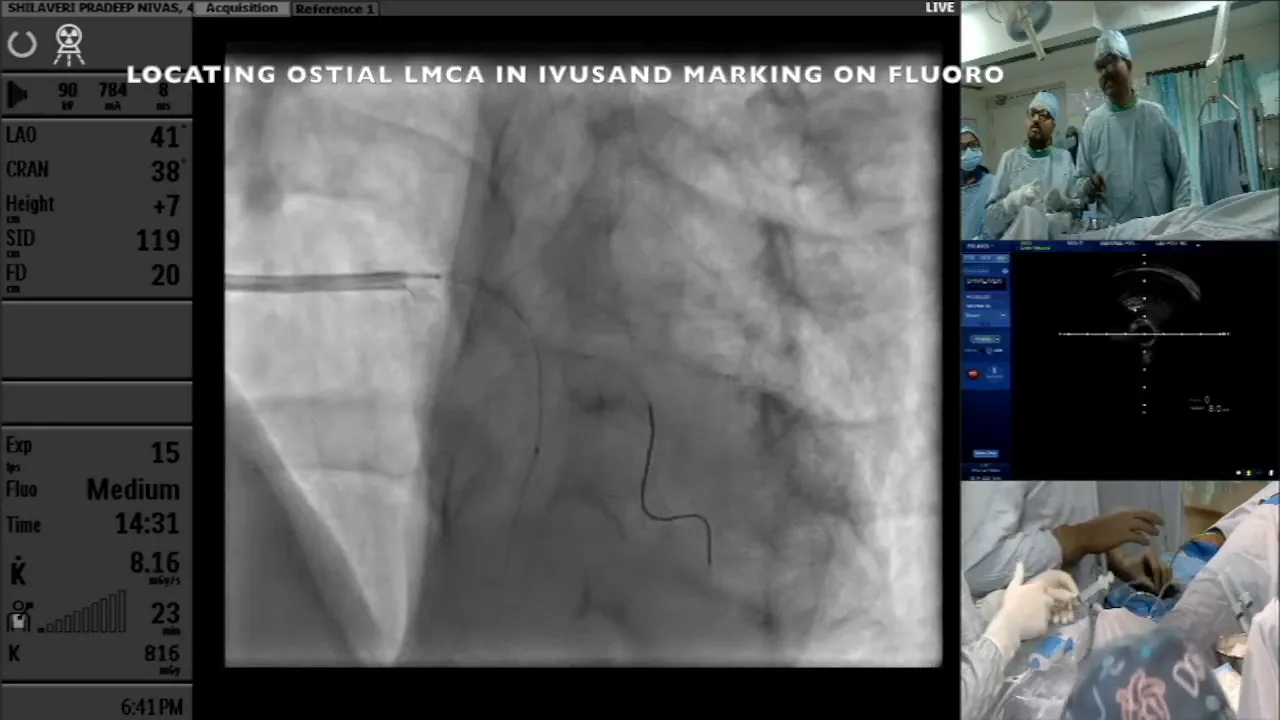
Understanding the Block Extension into LMCA
As we analyze the plaque extension into the LMCA, we note that the block extends significantly. The minimum lumen area is 6.9 mm², but the extension into the LMCA raises concerns about the overall integrity of the artery.
Evaluating the block extension is essential for planning the stenting strategy. If the block extends more than 3 mm into the LMCA, it becomes imperative to consider extending the stent from the ostial LMCA into the LAD to ensure comprehensive coverage and minimize the risk of future interventions.
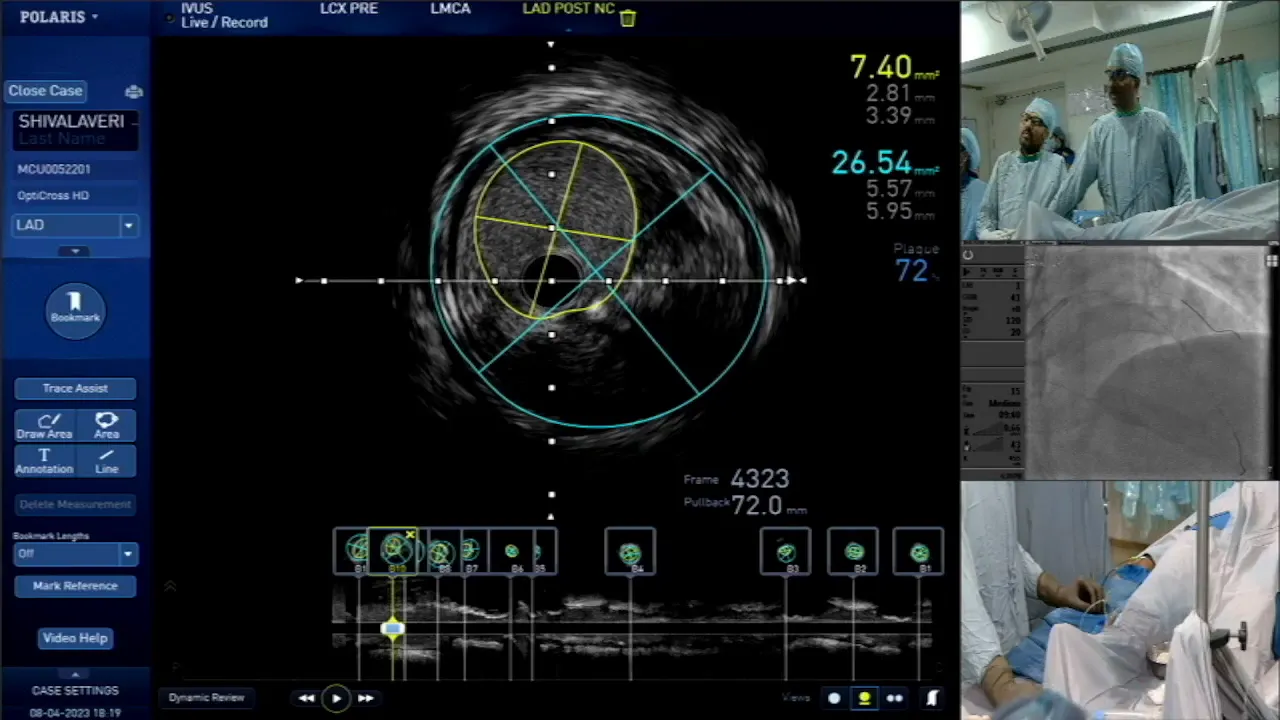
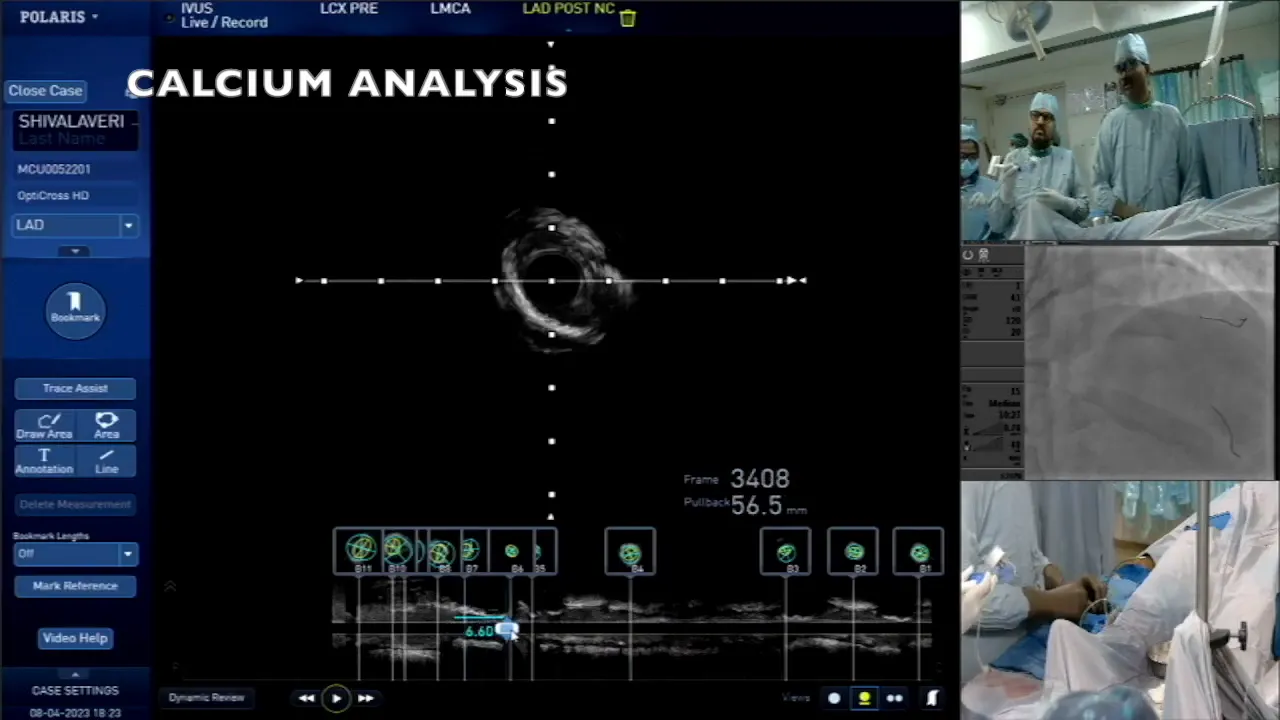
Calcium Assessment in Proximal LED
Calcium presence significantly impacts the treatment approach. In the proximal LED, we observe extensive calcification, characterized by an arc of calcium greater than 180°. This finding is crucial as it influences the need for calcium modification techniques during stenting.
Our IVUS calcium scoring indicates a score of 2, suggesting the need for some form of calcium modification. The length of the calcium is approximately 5 mm, which further complicates the intervention strategy.
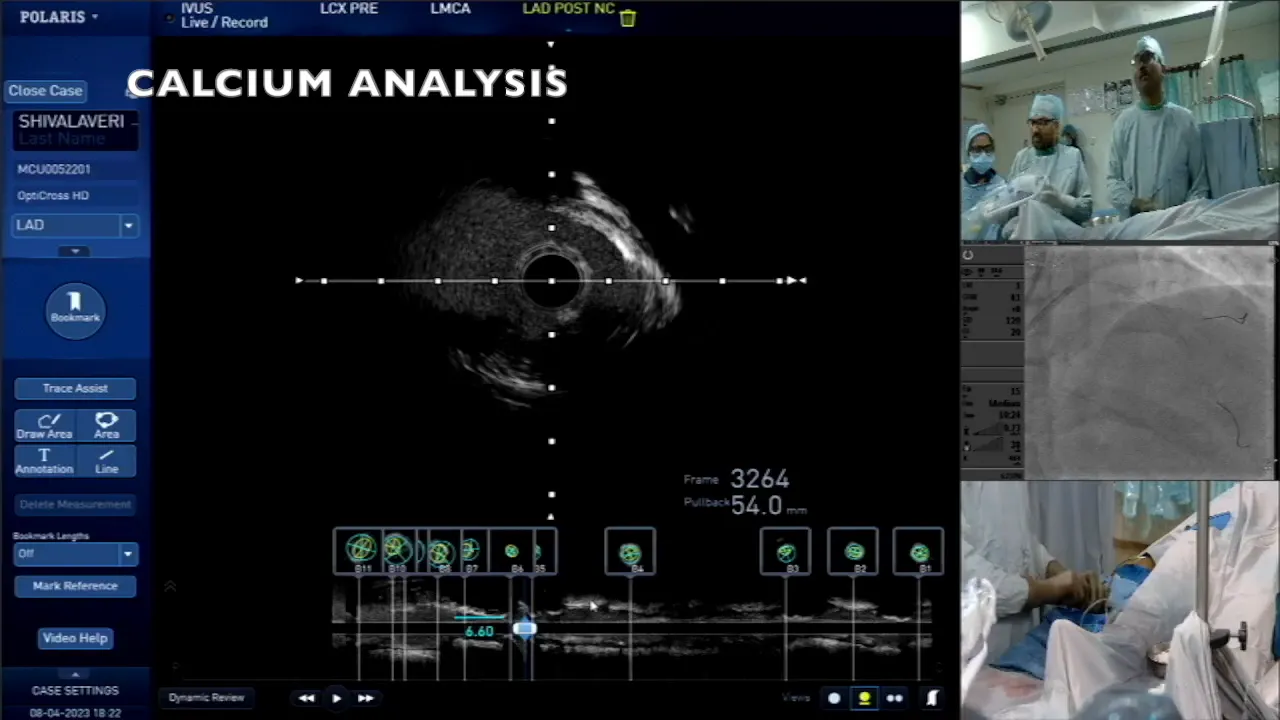
Understanding the distribution and depth of calcium helps determine the best approach for stenting. Both superficial and deep calcification must be addressed to ensure the success of the procedure and reduce the likelihood of restenosis.
Deciding on Calcium Modification Strategies
When faced with significant calcification during a PCI, selecting the right calcium modification strategy is crucial. In this case, the use of a cutting balloon is considered essential due to the extensive calcification observed in the proximal LED.
Typically, the size of the cutting balloon should be slightly smaller than the average diameter of the vessel. In this instance, the average diameter measured is 3.4 mm, leading to the choice of a 3.0 mm cutting balloon. This size allows for effective dilation while minimizing the risk of complications.

As the procedure progresses, it becomes vital to assess the ostial diagonal artery. The diameter measured here is 3.6 mm, indicating that careful evaluation is needed before proceeding with stenting. The operator must remain vigilant, especially when navigating areas of significant calcification.
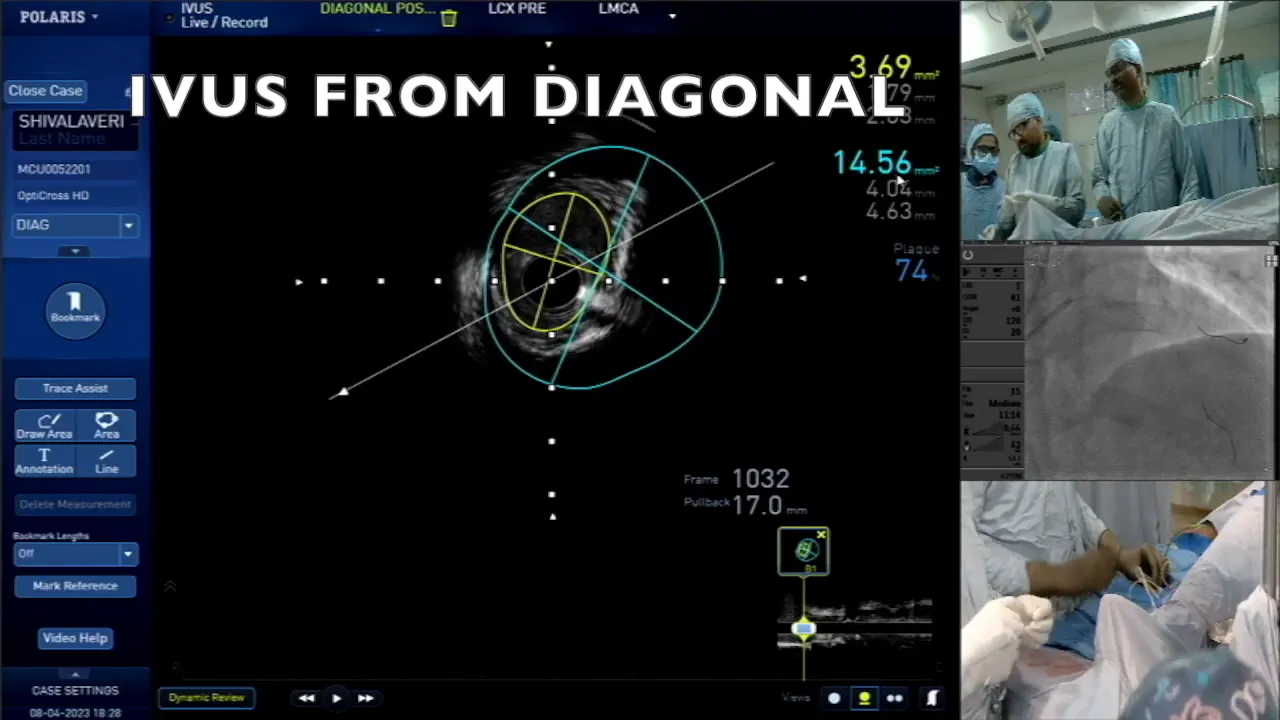
Evaluating Diagonal Lesion and Its Implications
The assessment of the diagonal artery is critical, given its size and potential implications for the overall procedure. Measurements indicate a lumen area of 3.6 mm², which is satisfactory. However, the presence of a flap in the artery raises concerns regarding the stability of the lesion.
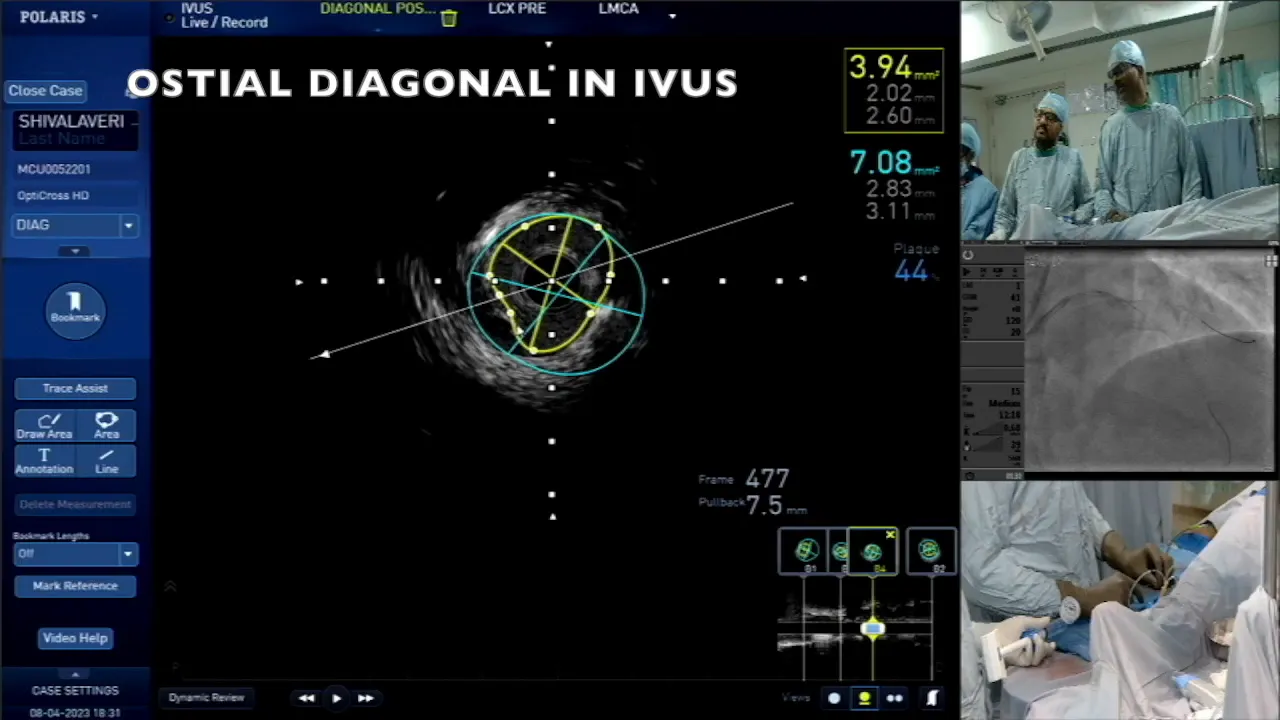
In such cases, the operator must decide whether to proceed with provisional stenting or to adopt a more aggressive approach. The flap’s short length and the overall angle of the dissection, which is around 30°, suggest that a conservative approach may be warranted. This decision balances the risk of complications against the need for effective treatment.
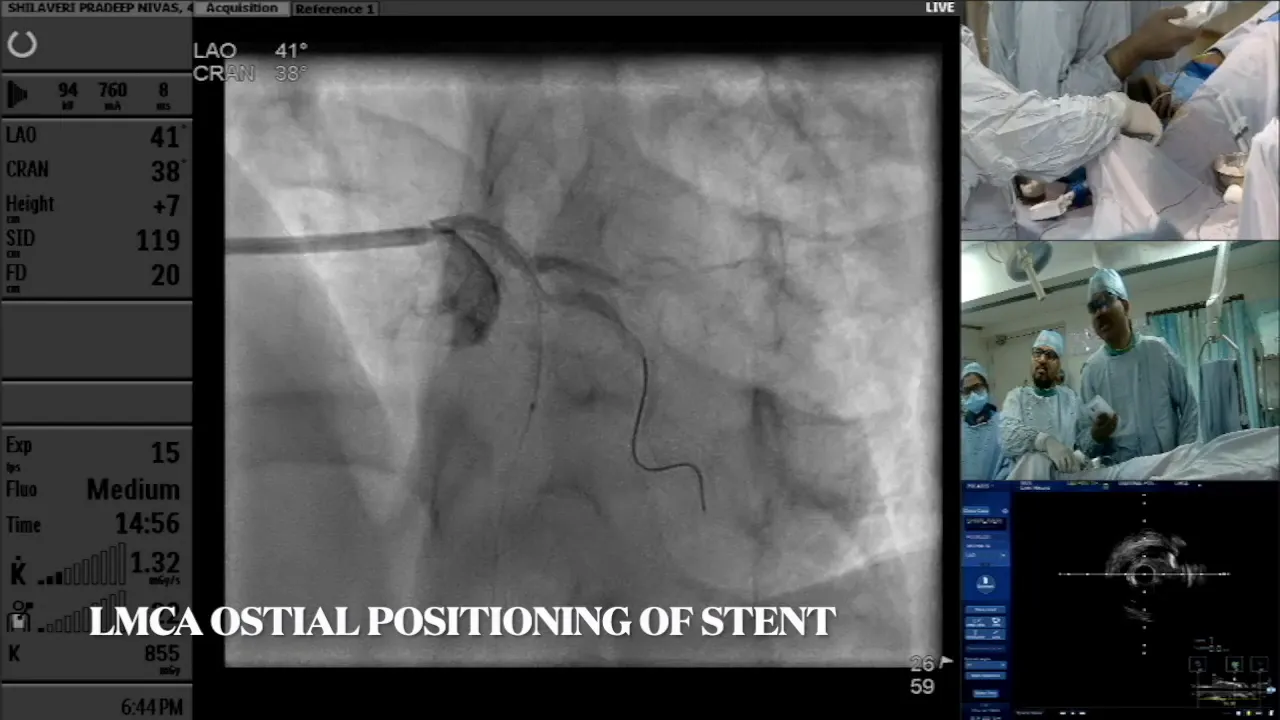
Final Stenting Strategy and Execution
As the procedure nears its conclusion, establishing a clear stenting strategy becomes paramount. The proximal stent is placed first to secure the arterial integrity before addressing the distal area. This approach minimizes the risk of overlapping stents on the diagonal artery, which could compromise its function.
With the proximal stent in place, the focus shifts to the distal segment. The diameter measurements obtained indicate a need for a 3.5 mm stent in this region. Careful deployment is essential, especially considering the presence of significant calcification.
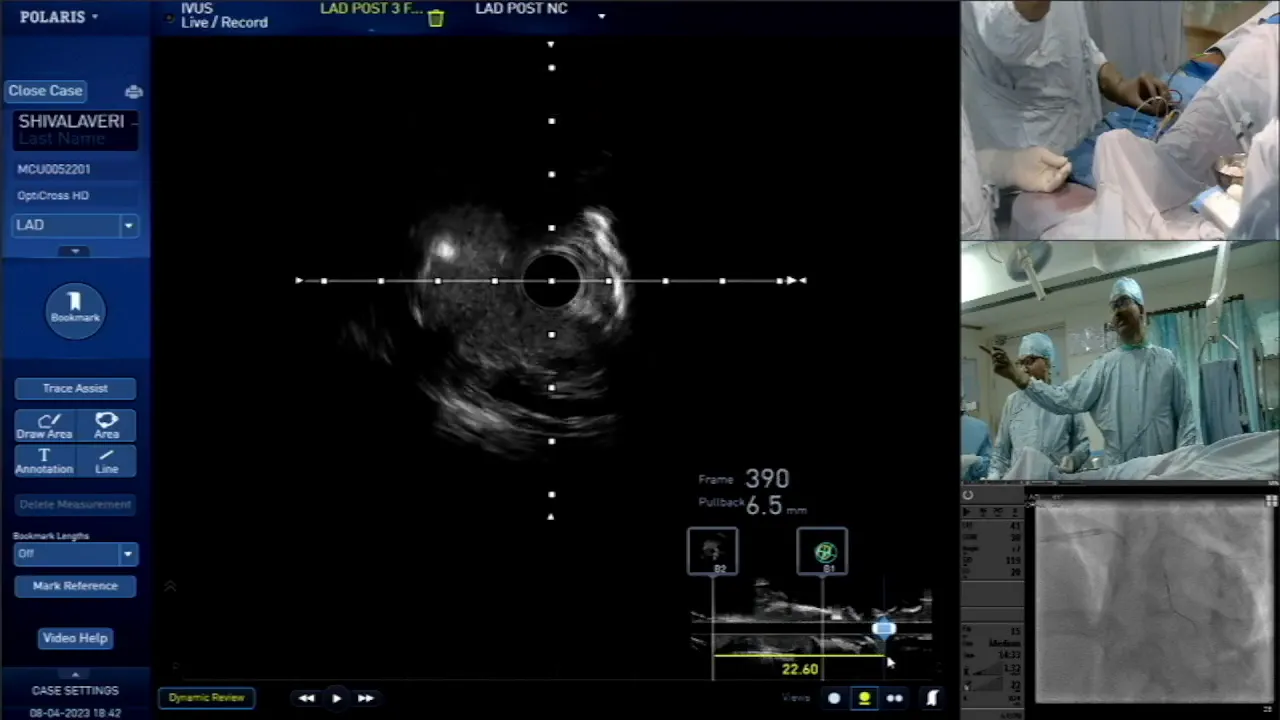
Throughout the stenting process, continuous imaging guidance is employed to ensure precise placement. The operator must be prepared to adjust the strategy based on real-time observations of the arterial response to the stents.
Post-Deployment Considerations
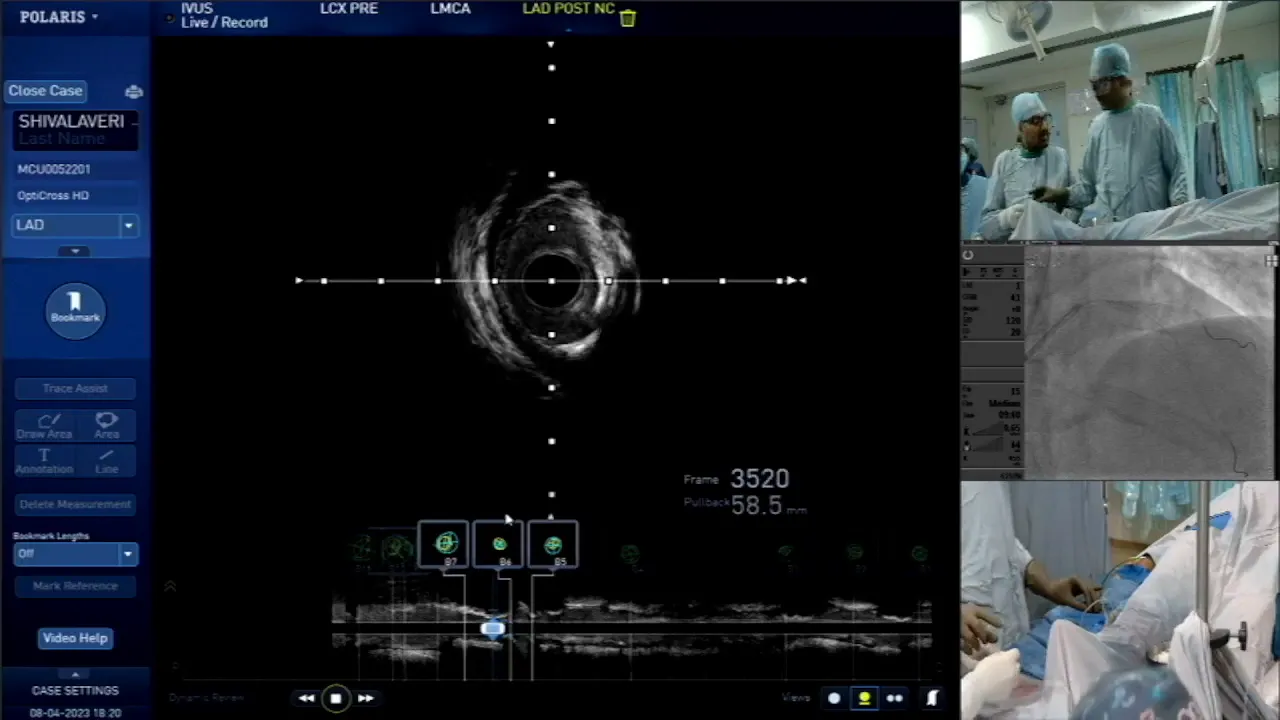
Once the stents are deployed, post-deployment evaluation is critical. This involves assessing the patency of the arteries and ensuring that there are no complications such as significant dissections or residual lesions. Continuous imaging helps monitor the outcome of the procedure effectively.
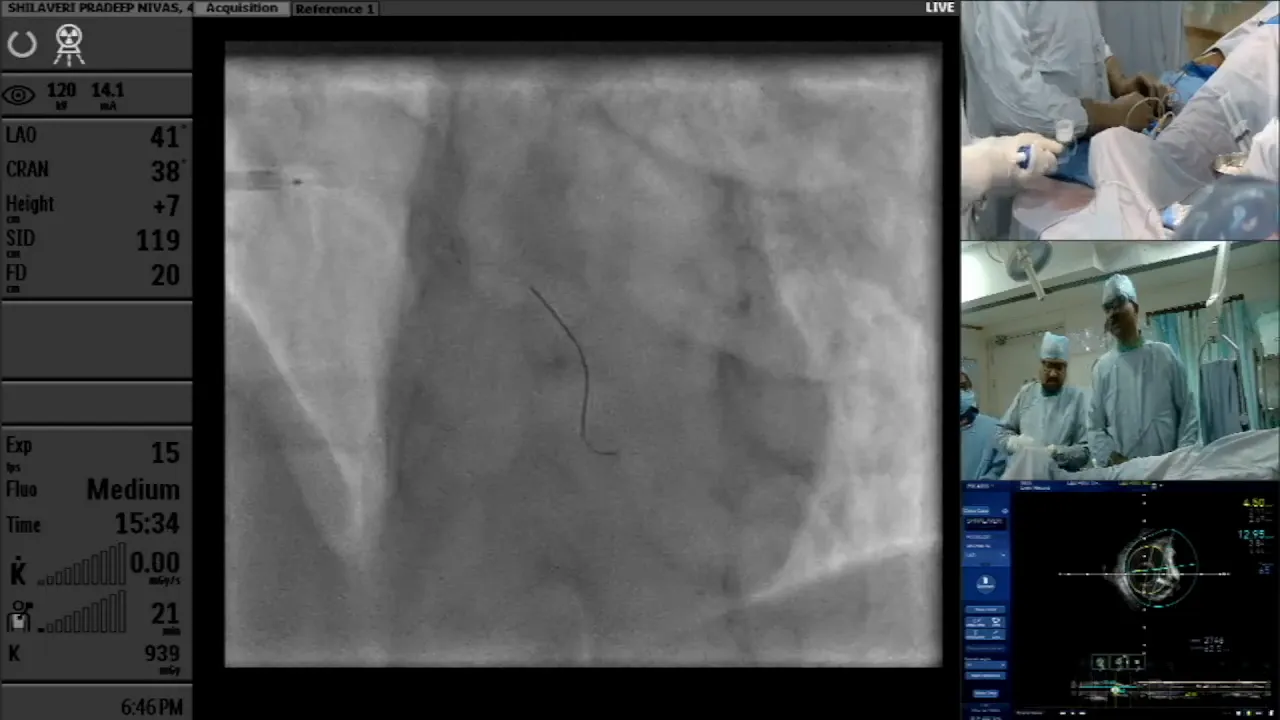
In conclusion, the management of complex bifurcation lesions requires a systematic approach. From assessing calcification to employing appropriate stenting techniques, each step is vital for optimizing patient outcomes. The integration of imaging techniques facilitates informed decision-making throughout the procedure.
FAQs
- What is the role of calcium modification in PCI? Calcium modification techniques, such as the use of cutting balloons, help to manage significant arterial calcification, facilitating better stent deployment.
- How do you decide on the size of the stent? The stent size is determined based on the average diameter of the artery measured during imaging, with a slight reduction in size to ensure a secure fit.
- Why is it important to avoid overlapping stents on side branches? Overlapping stents on side branches can impede blood flow and lead to complications; hence, careful planning is essential.


No Comments