25 Jul Facilitated ADR in Post-CABG RCA CTO: A Comprehensive Live Case Review by Dr. Sharath Reddy
In this detailed clinical discussion, Dr. Sharath Reddy, a consultant cardiologist, takes us through a complex case of chronic total occlusion (CTO) of the right coronary artery (RCA) in a post-coronary artery bypass graft (CABG) patient. The focus is on the application of facilitated antegrade dissection and re-entry (ADR) technique to successfully recanalize the occluded vessel, highlighting the challenges and strategic decisions involved. This article breaks down the procedural steps, anatomical considerations, and technical nuances of this advanced interventional cardiology procedure, offering valuable insights for cardiologists and healthcare professionals managing similar high-risk CTO cases.
Table of Contents
- Introduction to the Case
- Anatomical and Angiographic Assessment
- Strategic Planning: Antegrade vs Retrograde Approach
- Procedural Steps: Primary Retrograde Wiring
- Technical Challenges and Solutions
- Imaging Confirmation and Final Result
- Key Takeaways and Conclusion
- Frequently Asked Questions (FAQ)
- Final Thoughts
Introduction to the Case
The patient in question is a 63-year-old male with a history of extensive coronary artery disease, including previous CABG surgery performed in 2009. The bypass grafts included a left internal mammary artery (LIMA) to the left anterior descending artery (LAD) and saphenous vein grafts (SVGs) to the right coronary artery (RCA) and other branches.
Recently, a coronary angiogram demonstrated:
- Native triple vessel disease with significant calcification.
- Patent LIMA to LAD graft.
- Occluded SVGs to the RCA and other vessels.
- Significant lesions in the left circumflex artery (LCX) and chronic total occlusion in the RCA.
Prior attempts at LCX stenting at another center were unsuccessful, and the patient has moderate to severe left ventricular systolic dysfunction, which further complicates procedural planning.
Anatomical and Angiographic Assessment
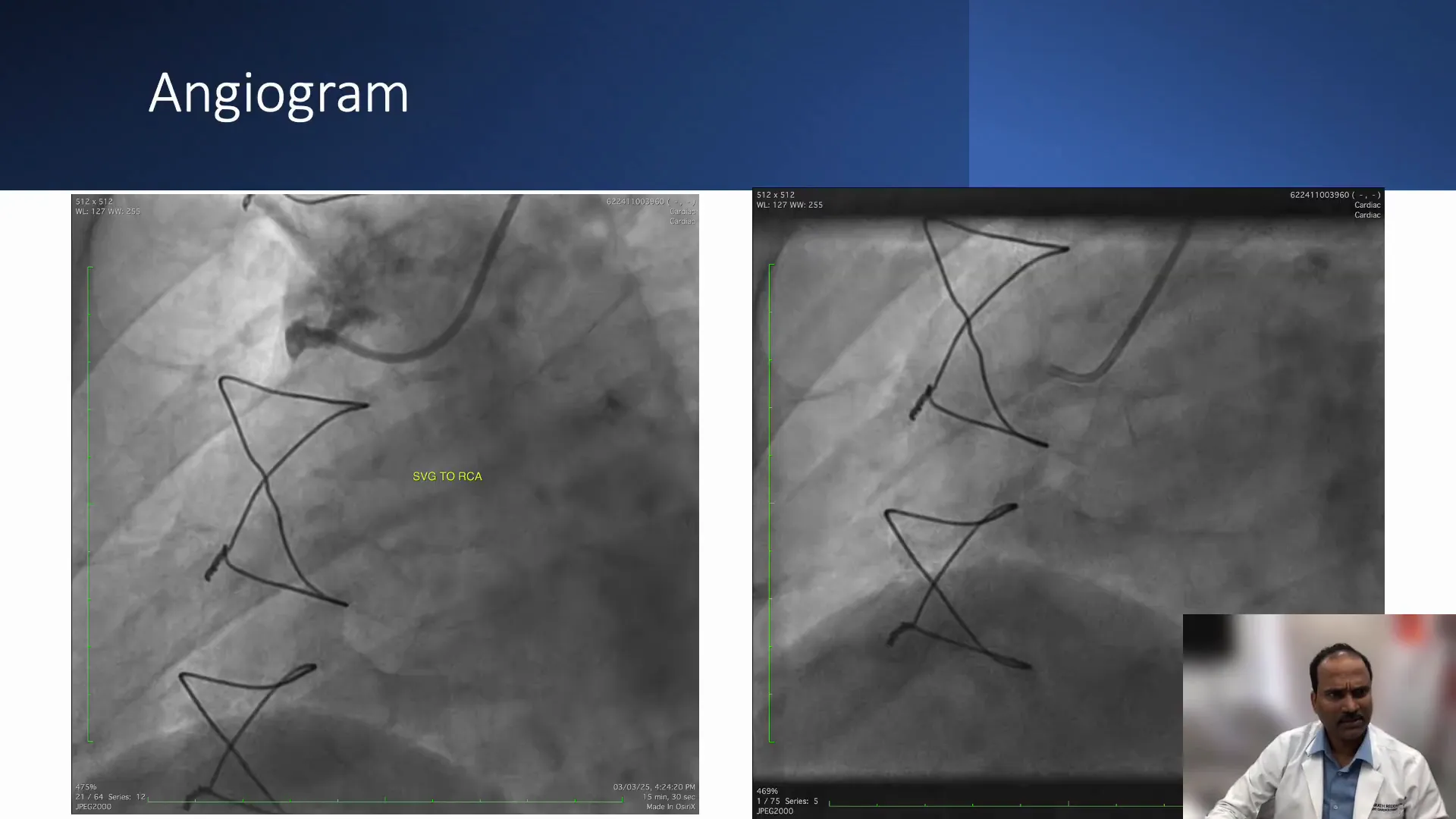
Understanding the anatomy is critical for planning the CTO intervention. The angiographic images reveal:
- SVG to RCA: Completely occluded.
- Native RCA: Significantly diseased from the origin with mid-vessel total occlusion.
- Distal RCA: Filling retrogradely via collaterals, particularly from the posterolateral branches.
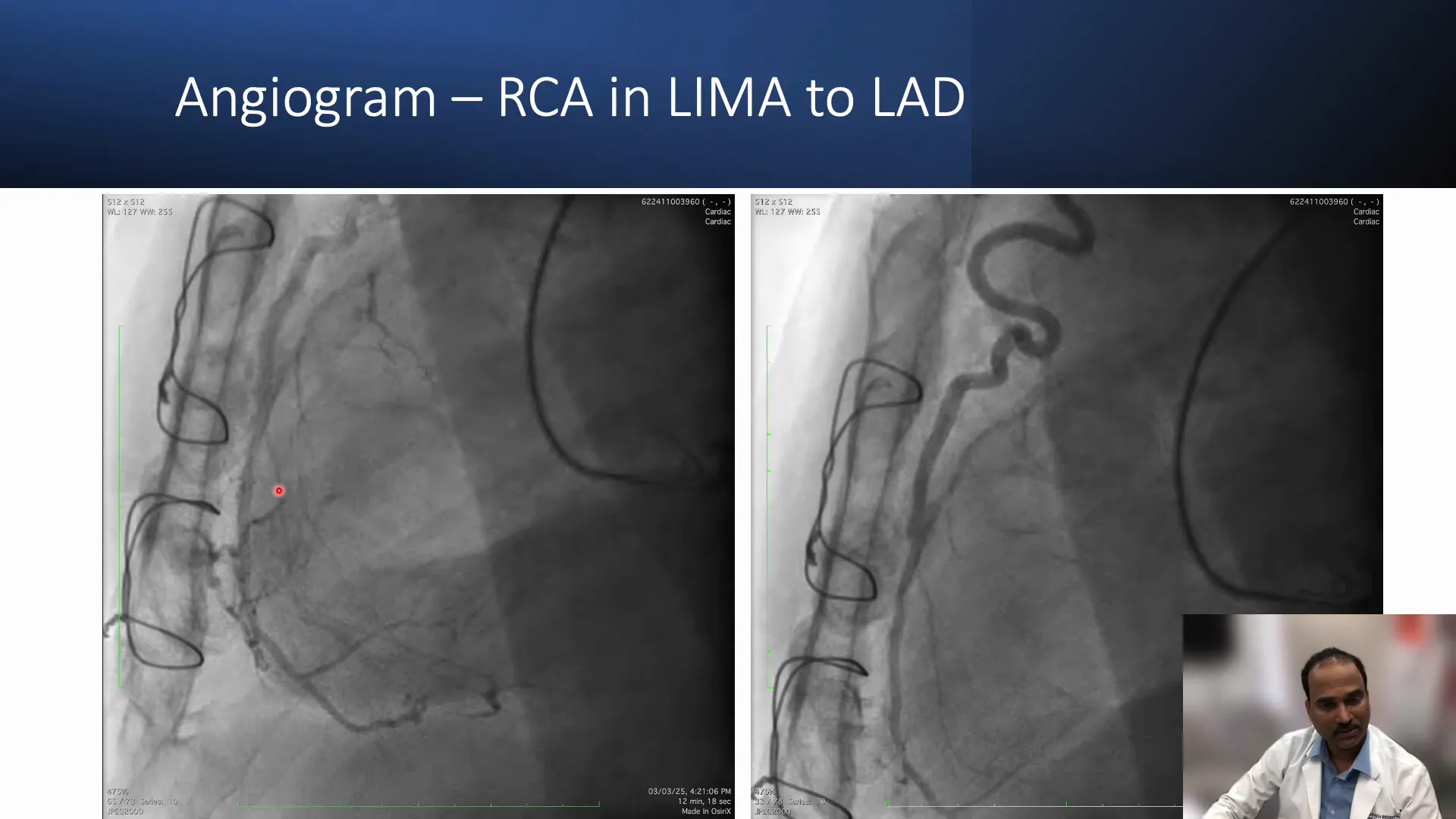
- LIMA to LAD graft: Patent and filling branches including the distal LAD and some right ventricular (RV) branches.
- Collateral circulation: Some septal collaterals are present but their connection to the posterior descending artery (PDA) is uncertain.
This anatomical complexity, combined with the presence of diffuse disease and calcification, sets the stage for a challenging CTO intervention.
Visibility and Wiring Challenges
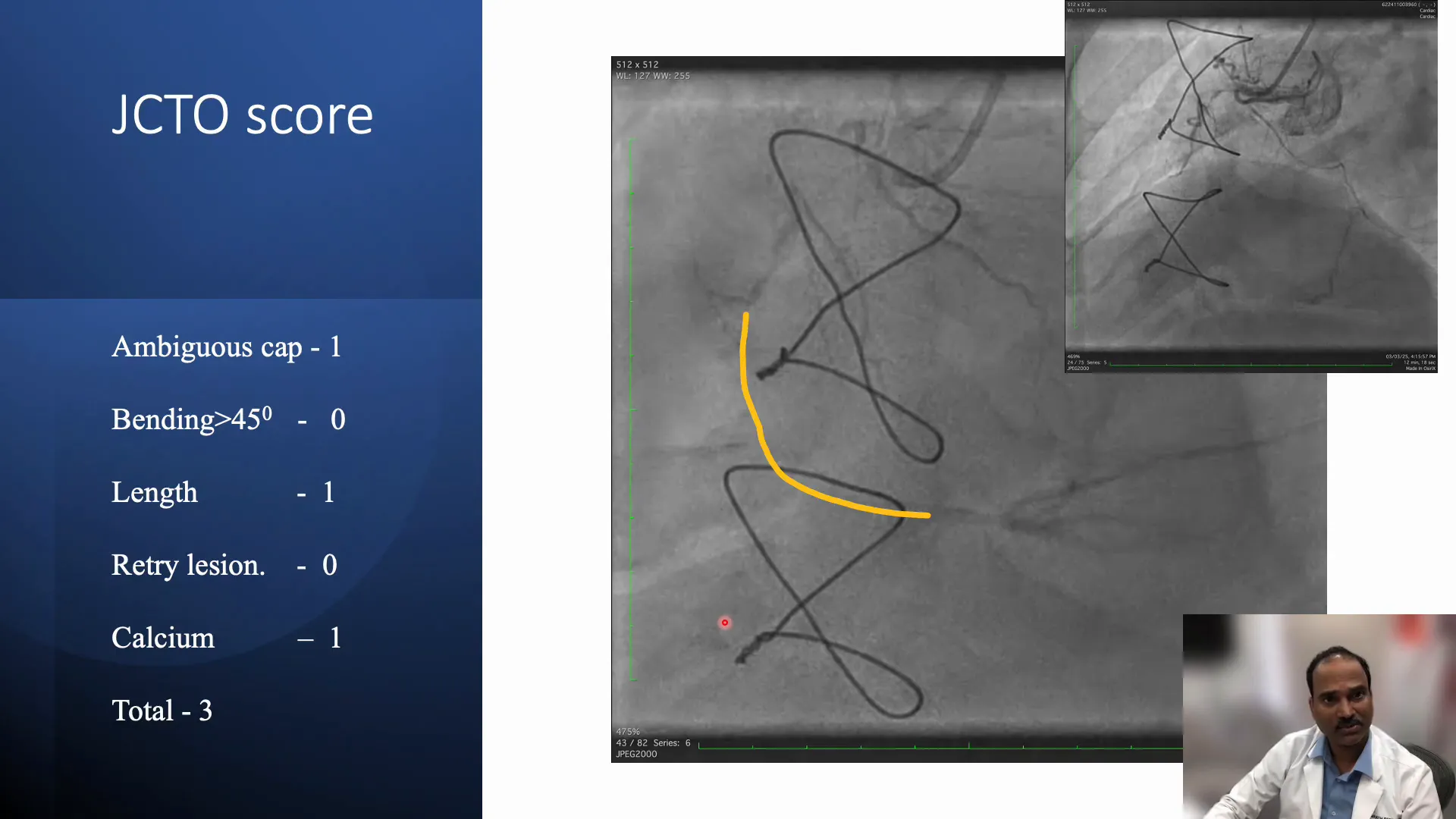
The native RCA is a very narrow, diffusely diseased vessel with poor visibility on angiography, making antegrade wiring difficult. Despite triple injections to visualize the RCA, the distal vessel remains ambiguous.
The lesion is heavily calcified, and the J-CTO score—a tool used to predict the difficulty of CTO interventions—is estimated to be 2 to 3, indicating a moderate to high level of complexity. The ambiguous proximal cap and long lesion length add to the procedural challenge.
Strategic Planning: Antegrade vs Retrograde Approach
Given the poor visibility and challenging anatomy, the decision was made to pursue a primary retrograde approach rather than antegrade wiring. Retrograde wiring involves crossing the occlusion by navigating through collateral channels or grafts in a reverse direction, which can sometimes offer better wire control and success in complex CTOs.
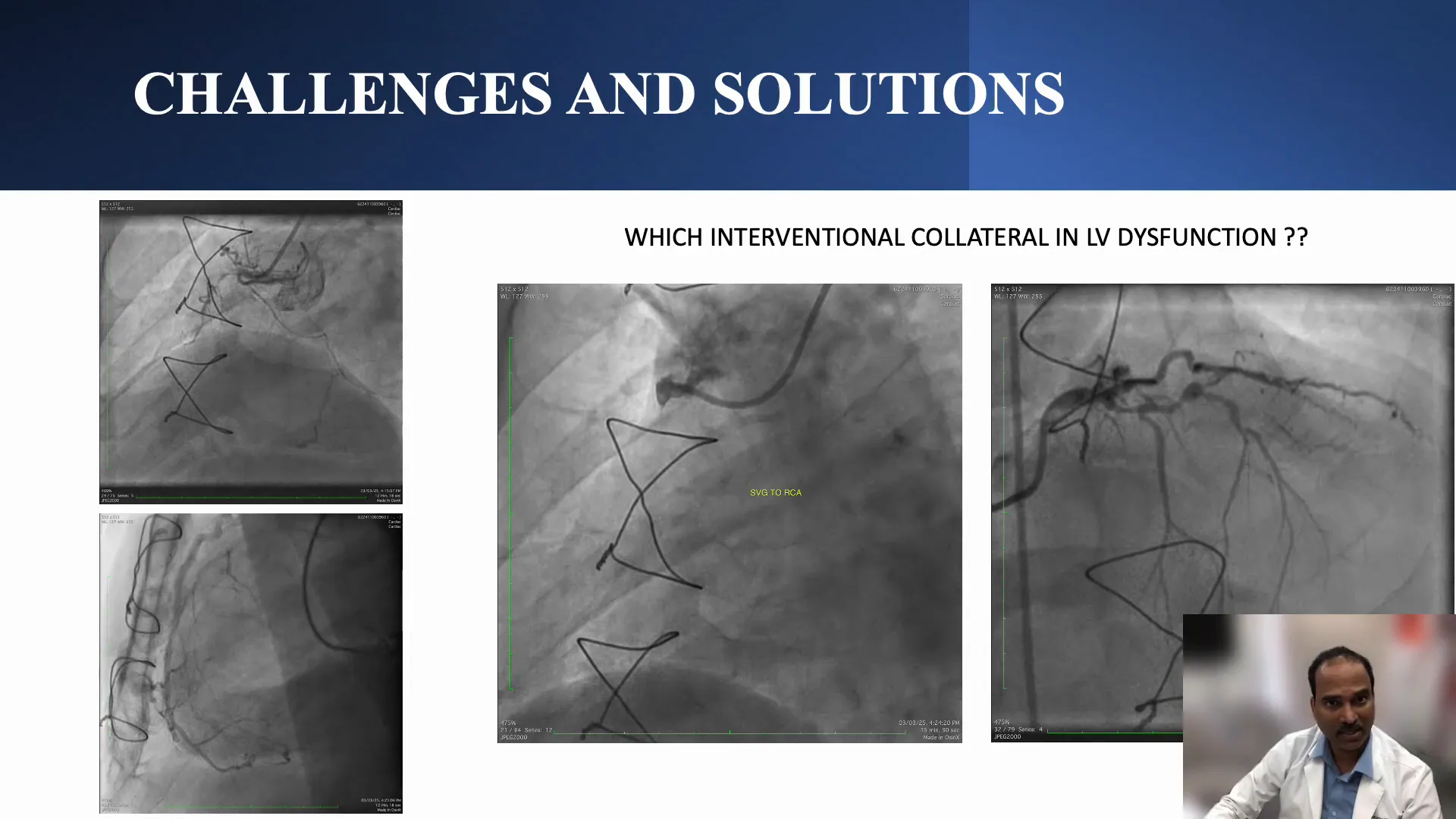
Choice of Retrograde Channel
Two main retrograde channels were considered:
- Septal collaterals: These are intramyocardial vessels that can be used as conduits for retrograde wiring.
- SVG to RCA: Although occluded, this graft could serve as a retrograde channel without causing ischemia.
Because the SVG to RCA was already occluded, using it as a retrograde channel was less likely to cause ischemia, especially important given the patient’s moderate to severe left ventricular dysfunction. In contrast, using large septal collaterals risked ischemic complications, so the SVG to RCA was selected as the retrograde route.
Procedural Steps: Primary Retrograde Wiring
The procedure began with dual angiography and antegrade injections through a microcatheter. However, it was observed that the RCA had become completely occluded up to the proximal segment, creating an ambiguous proximal cap with no clear entry point for antegrade wiring.
Therefore, the team proceeded with a primary retrograde approach:
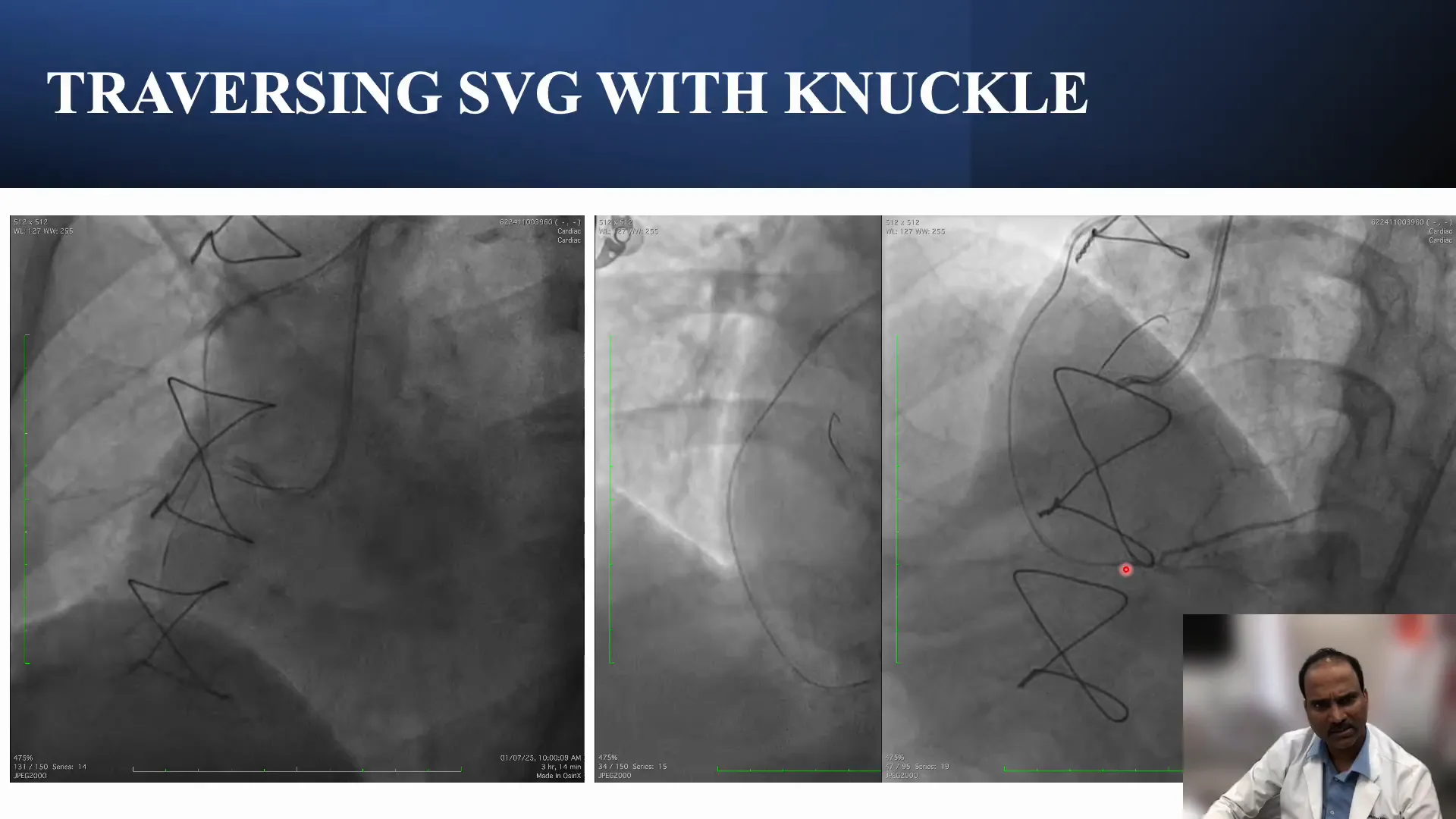
- Using a Gladius MG wire, which can be knuckled when needed, the operator entered the occluded SVG.
- A Corsair 150 microcatheter was advanced over the wire to facilitate navigation.
- The wire was knuckled and carefully advanced through the entire length of the occluded SVG graft.
- Once across the SVG, the microcatheter was advanced into the distal RCA beyond the occlusion.
Reaching the distal RCA retrogradely is a significant milestone, allowing options for subsequent wiring strategies.
Antegrade Wiring and Facilitated ADR
Upon reaching the distal RCA, the plan was to attempt antegrade wiring to cross the CTO from the proximal true lumen. However, due to the long lesion and ambiguous vessel course, antegrade wiring was likely to enter the subintimal space (beneath the vessel lining) rather than the true lumen.
When antegrade wiring results in subintimal dissection, facilitated ADR can be employed to re-enter the true lumen. This involves creating a controlled dissection plane and then re-entering the true vessel lumen using specialized techniques and devices.
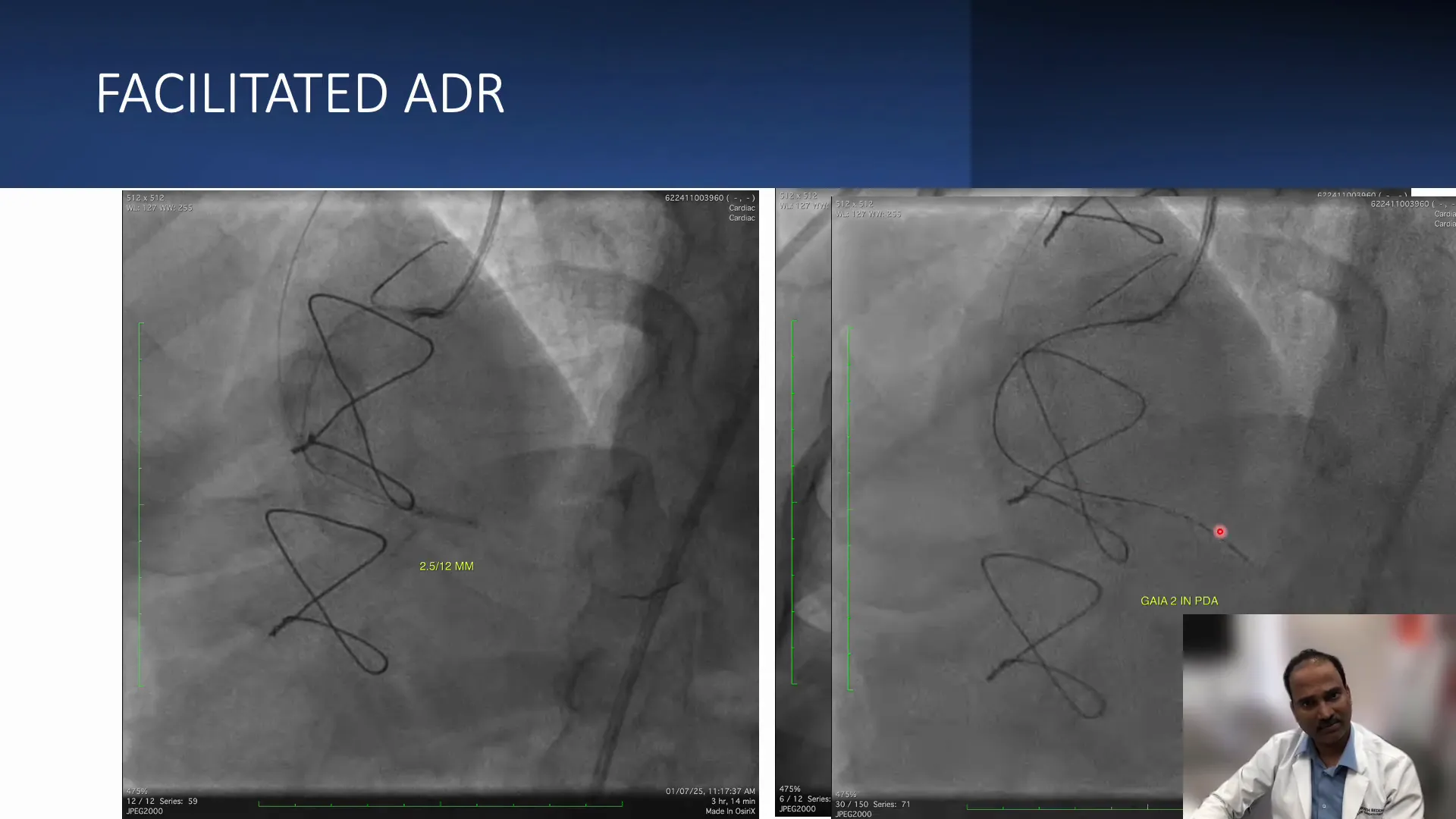
The facilitated ADR technique in this case involved:
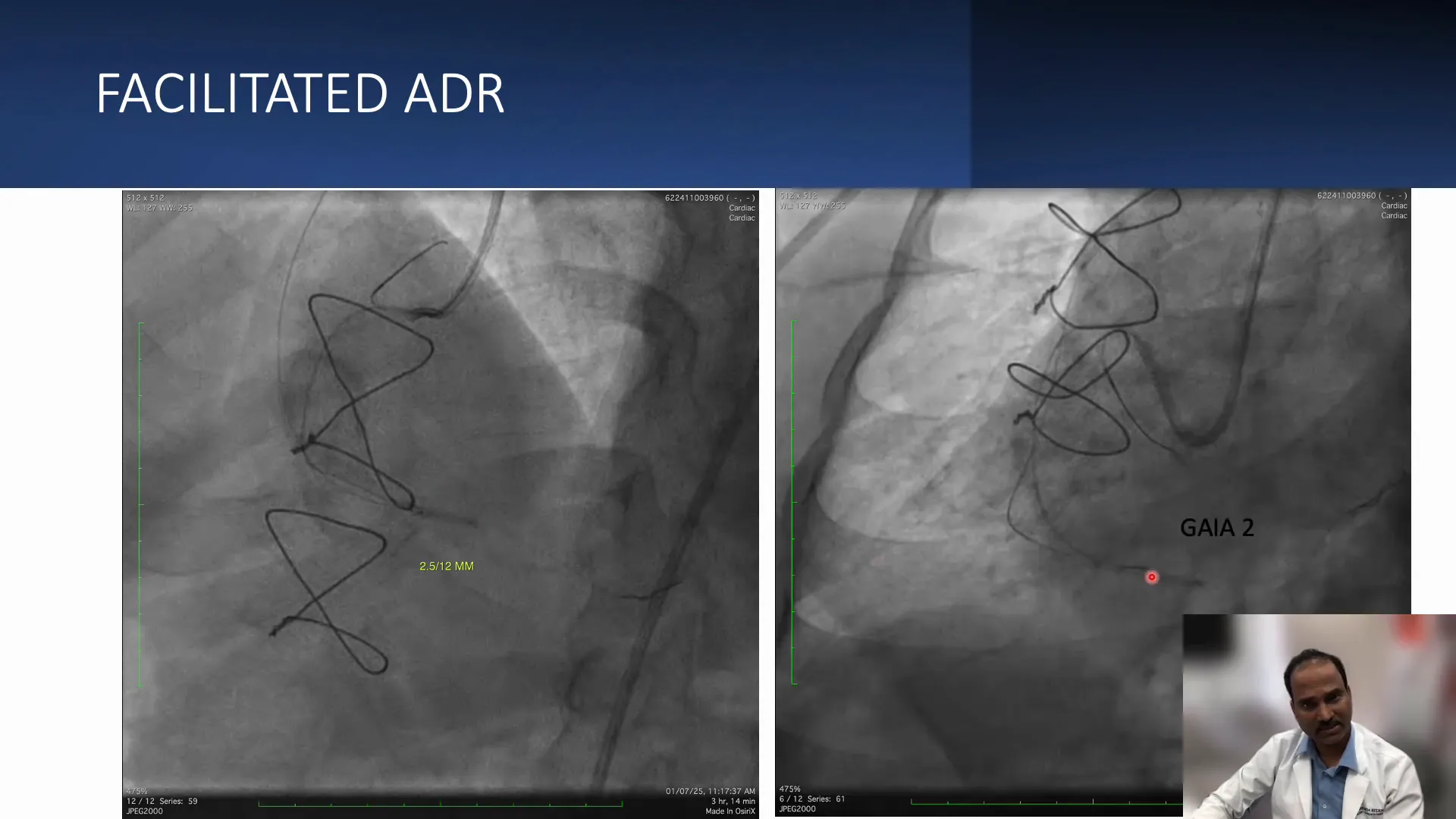
- Advancing a balloon retrogradely through the SVG graft to the distal RCA.
- Inflating the balloon to create a target for antegrade wire re-entry.
- Using a directable antegrade wire (Gaia 2) through an antegrade microcatheter (Corsair) to target the balloon and achieve re-entry.
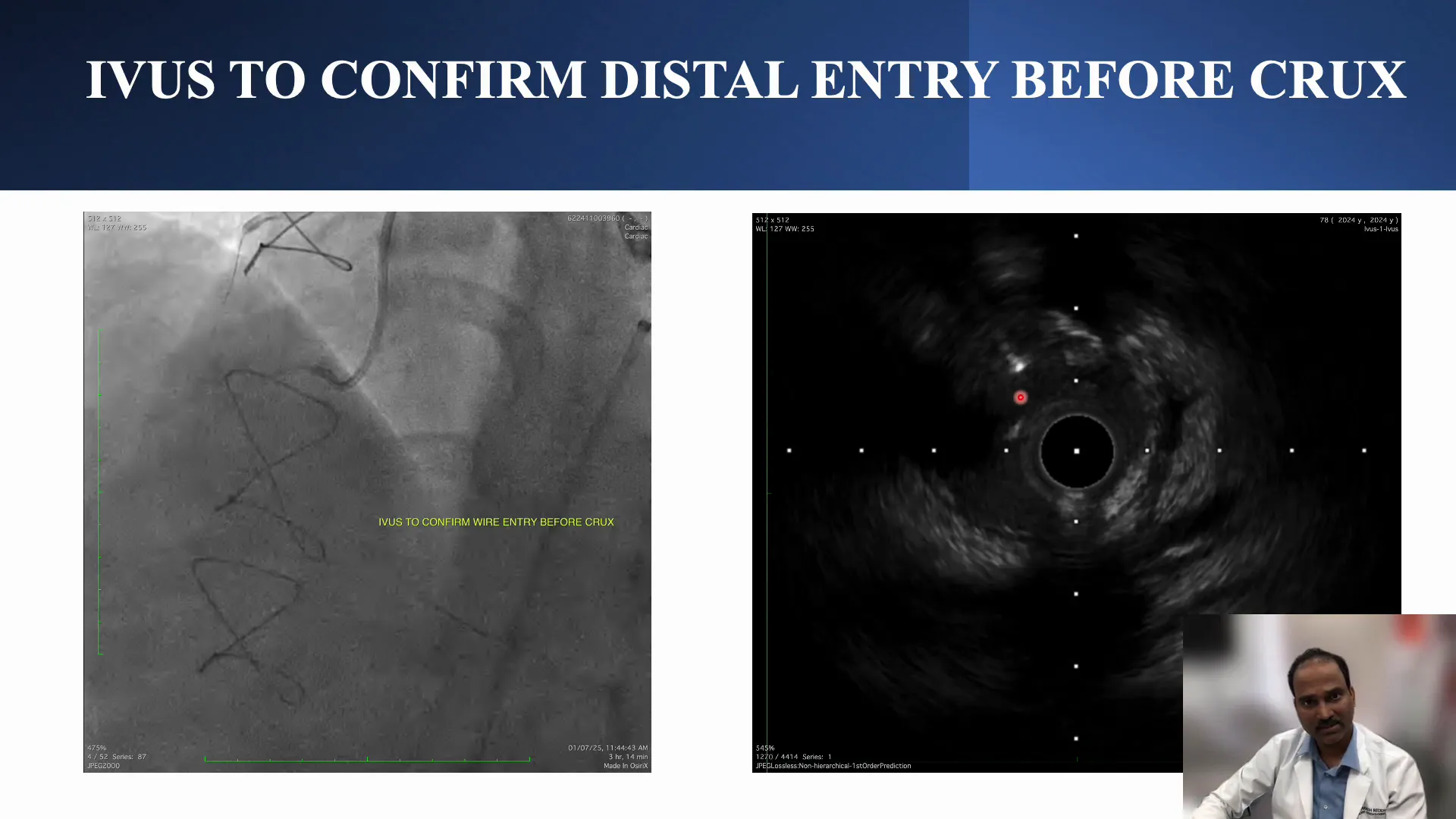
- Confirming entry into the true lumen with imaging techniques such as intravascular ultrasound (IVUS) or optical coherence tomography (OCT).
Technical Challenges and Solutions
Wire Position and Vessel Architecture
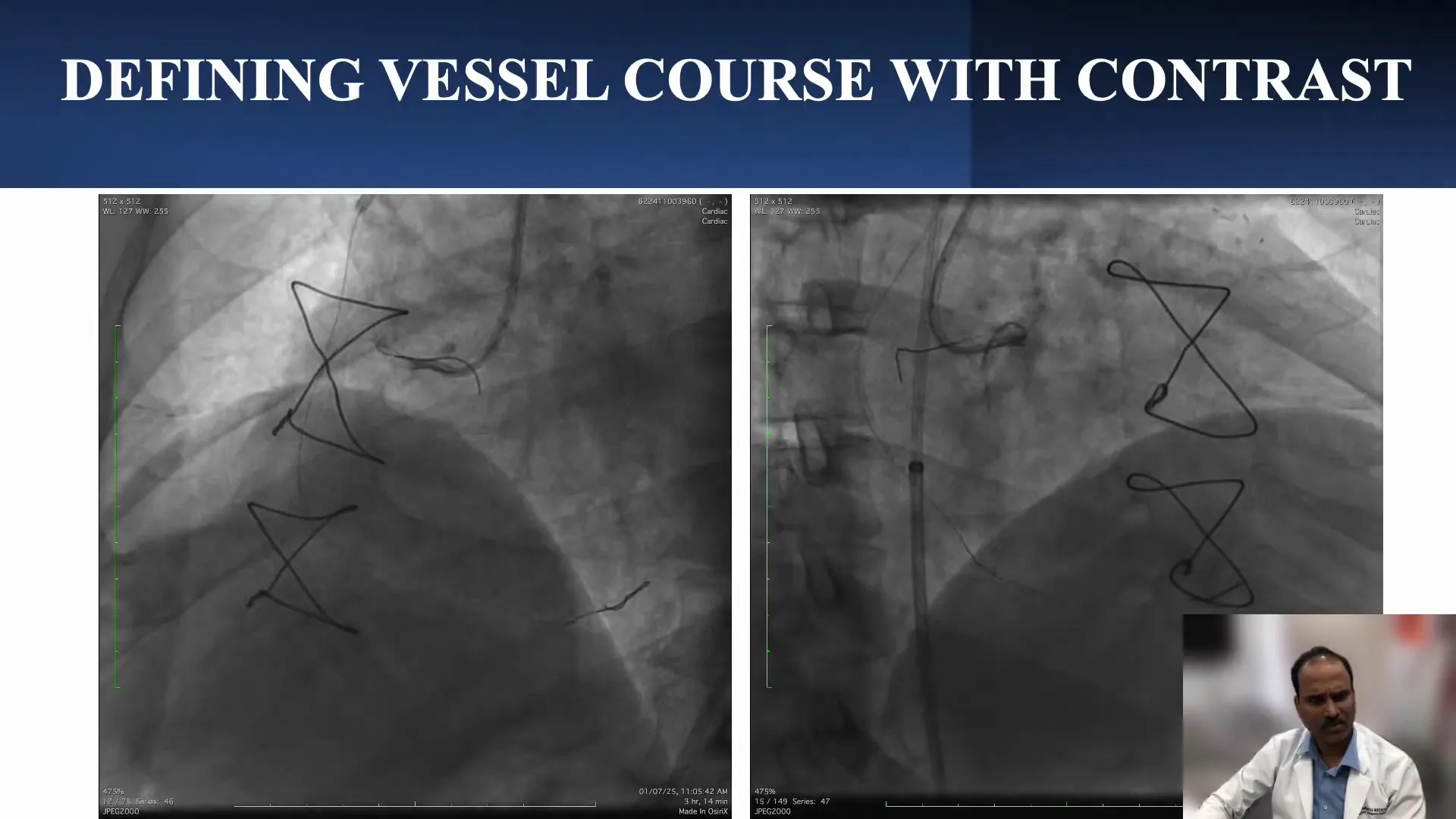
During antegrade wiring, the wire’s position within the vessel architecture is critical. The operator used two orthogonal angiographic views to ensure the wire was within the vessel wall and not outside it.
Initially, the wire appeared to be stuck, and balloon dilatation was used to advance the microcatheter further. However, upon injecting contrast, it was evident that the wire had taken a posterior course, not within the true lumen but in the subintimal or false lumen space.
Knuckle Wire Technique
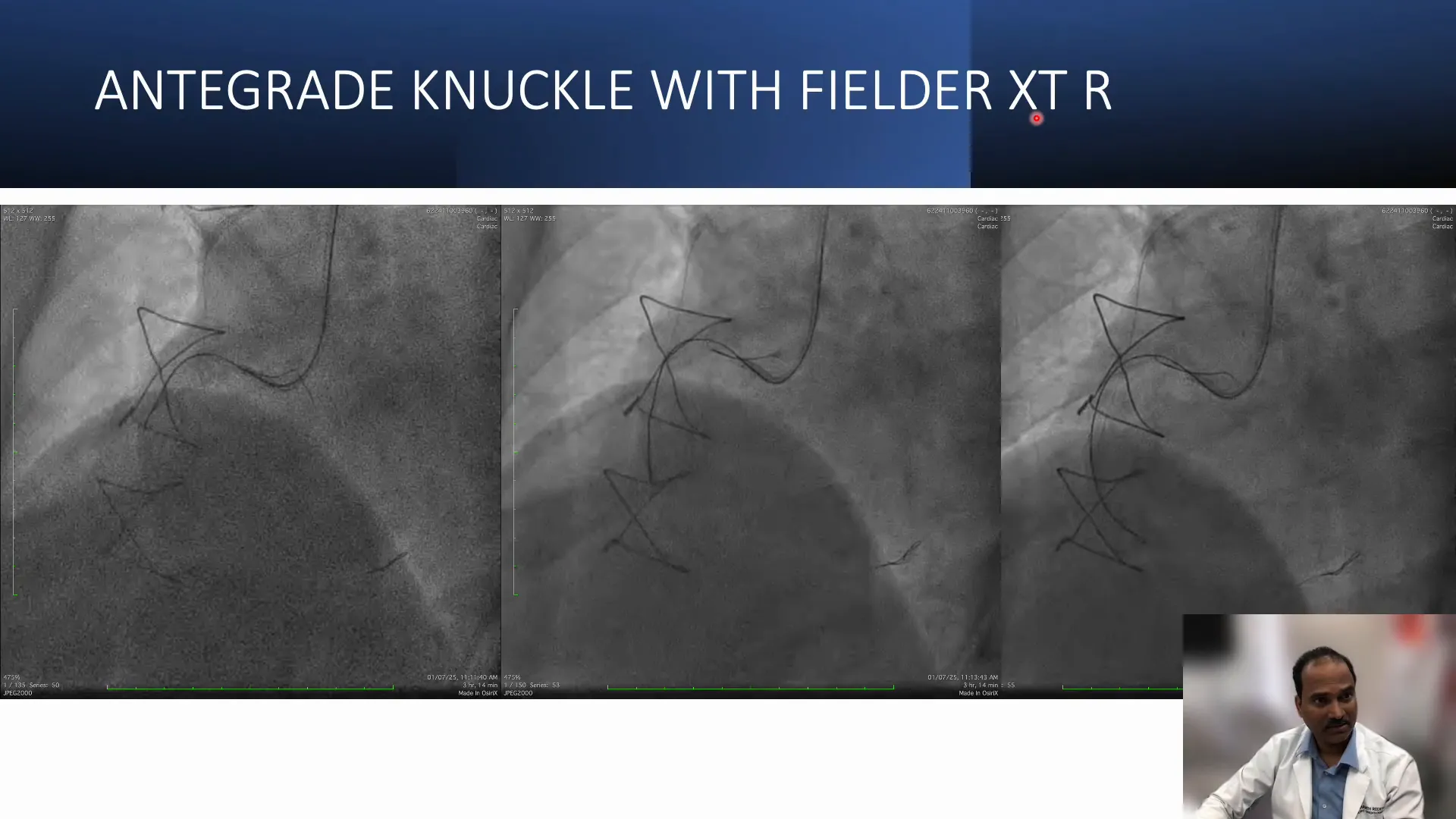
To navigate this problem, the operator used the knuckle wire technique again, this time with a Filter XTR wire, which was knuckled to safely advance within the vessel architecture and avoid perforation.
Confirmation of wire position was made in two views, ensuring the knuckle was traveling within the vessel wall architecture. The Corsair microcatheter was then advanced along the knuckle wire.
Facilitated ADR and Re-entry Proximal to Crux
One of the critical aspects of facilitated ADR, especially in the RCA, is ensuring that re-entry occurs proximal to the crux of the heart. The crux is the area where the RCA gives off important branches, and losing these branches can compromise myocardial perfusion.
Therefore, the team dilated a 2.5 mm balloon retrogradely in the distal RCA before the crux, creating a target for antegrade wire re-entry. Using the Gaia 2 wire through the antegrade Corsair catheter, the operator guided the wire toward the balloon under two orthogonal angiographic views, employing an “end balloon and side balloon” technique to facilitate re-entry into the true lumen.
Imaging Confirmation and Final Result
Intravascular imaging (likely IVUS or OCT) was used to confirm that the antegrade wire had re-entered the true lumen proximal to the crux. This confirmation is vital to ensure that the main branches are preserved.
The imaging revealed:
- True lumen entry with the wire in the proper vessel plane.
- Another branch joining the true lumen near the re-entry site.
- Progression proximally where the wire eventually entered the subintimal space, compressing the true lumen.
- The retrograde wire from the SVG remained in the true lumen, highlighting the complex spatial relationship.
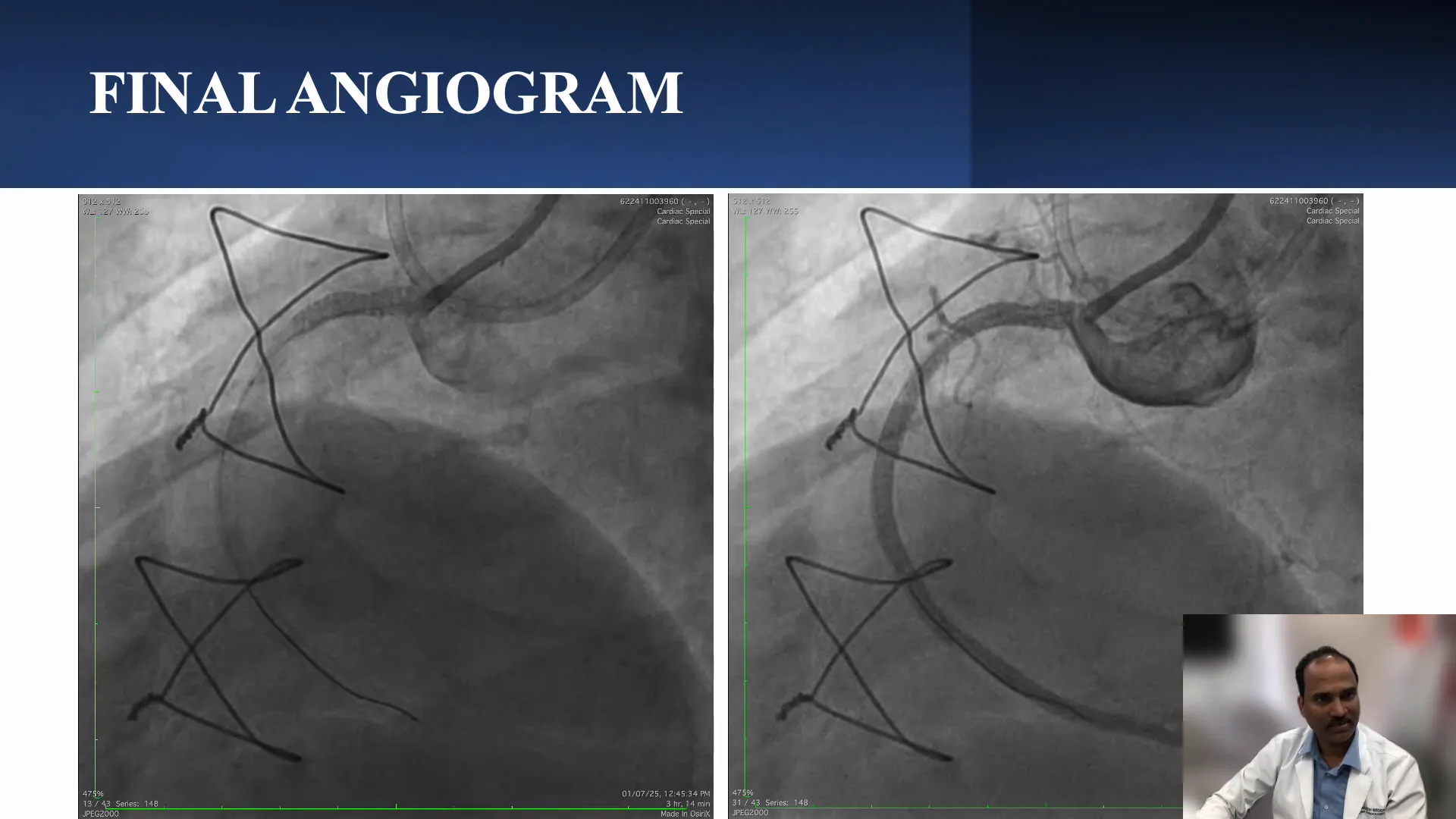
Stenting and Final Angiographic Outcome
Once re-entry was confirmed, the entire length of the RCA was stented from distal to proximal. The final angiogram showed:
- Good filling of the distal RCA and its branches.
- Preservation of most side branches except two acute marginal branches that were lost due to the subintimal course.
- These lost branches were well supplied by the LAD via the LIMA graft, mitigating clinical impact.
- Some under-expansion of stents was noted due to the subintimal route, highlighting the limitations of this approach.
The operator emphasized accepting suboptimal stent expansion in long subintimal segments to avoid complications such as vessel perforation.
Key Takeaways and Conclusion
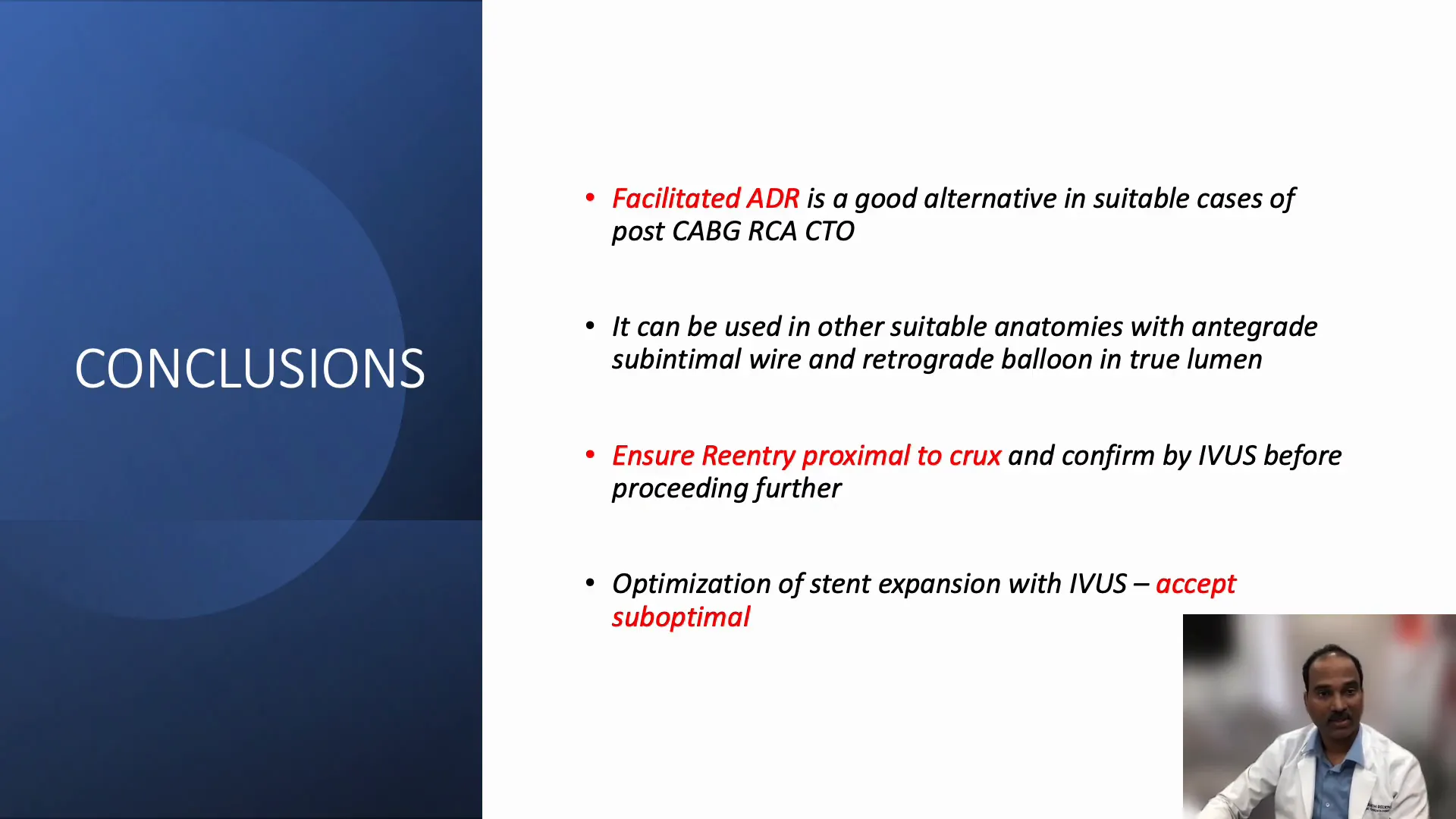
This case underscores the complexity of CTO interventions in post-CABG patients, especially involving the RCA with ambiguous proximal caps and diffuse disease. Facilitated ADR emerges as a valuable technique in these challenging scenarios, provided that certain principles are adhered to:
- Patient Selection: Facilitated ADR is particularly useful in post-CABG RCA CTOs and other anatomies where antegrade wire is in the subintimal space, and retrograde balloon delivery is possible.
- Channel Choice: Selecting the retrograde channel carefully to minimize ischemia risk, especially in patients with LV dysfunction. Occluded SVGs can be preferred over septal collaterals to avoid ischemic complications.
- Re-entry Proximity: Ensuring re-entry is proximal to the crux to preserve vital side branches.
- Imaging Guidance: Confirming wire position and re-entry using intravascular imaging is critical for procedural success and safety.
- Accepting Limitations: Suboptimal stent expansion may occur in subintimal courses; aggressive optimization should be avoided to prevent complications.
Dr. Sharath Reddy’s live lecture provides a vivid demonstration of facilitated ADR’s role in contemporary CTO interventions, offering a practical roadmap for complex cases.
Frequently Asked Questions (FAQ)
What is Facilitated ADR in CTO interventions?
Facilitated antegrade dissection and re-entry (ADR) is a technique used to cross chronic total occlusions when the antegrade wire enters the subintimal space. It involves creating a controlled dissection plane and then re-entering the true lumen using specialized wires and balloons, often assisted by retrograde balloon inflation.
Why choose a retrograde approach in CTO cases?
The retrograde approach is selected when antegrade wiring is difficult due to ambiguous proximal caps, poor vessel visibility, or long lesions. It involves crossing the occlusion from distal to proximal through collateral channels or grafts, improving wire control and success rates in complex CTOs.
What are the risks of using septal collaterals as a retrograde channel?
Using septal collaterals may cause ischemia during the procedure, especially in patients with left ventricular dysfunction. Large septal vessels are vital for myocardial perfusion, and their occlusion or injury can lead to complications, which is why occluded SVGs are often preferred.
How important is imaging during CTO interventions?
Intravascular imaging (IVUS or OCT) is essential to confirm wire position within the true lumen, guide re-entry, and optimize stent deployment. It helps prevent complications and ensures procedural success.
Can facilitated ADR be used in vessels other than RCA?
Yes, facilitated ADR can be applied in other suitable anatomies where the retrograde balloon can be delivered into the true lumen, and the antegrade wire is in the subintimal space. Each case requires careful anatomical and procedural planning.
Final Thoughts
Managing CTOs in post-CABG patients demands advanced interventional skills, meticulous planning, and adaptability. Facilitated ADR offers a powerful strategy to overcome anatomical challenges, especially in the RCA where preserving side branches is crucial. Dr. Sharath Reddy’s case exemplifies how combining antegrade and retrograde techniques, guided by imaging and careful wire manipulation, can achieve successful revascularization even in the most difficult scenarios.
For those interested in deepening their understanding of CTO interventions and complex PCI strategies, following such expert live cases and lectures can be invaluable.


No Comments