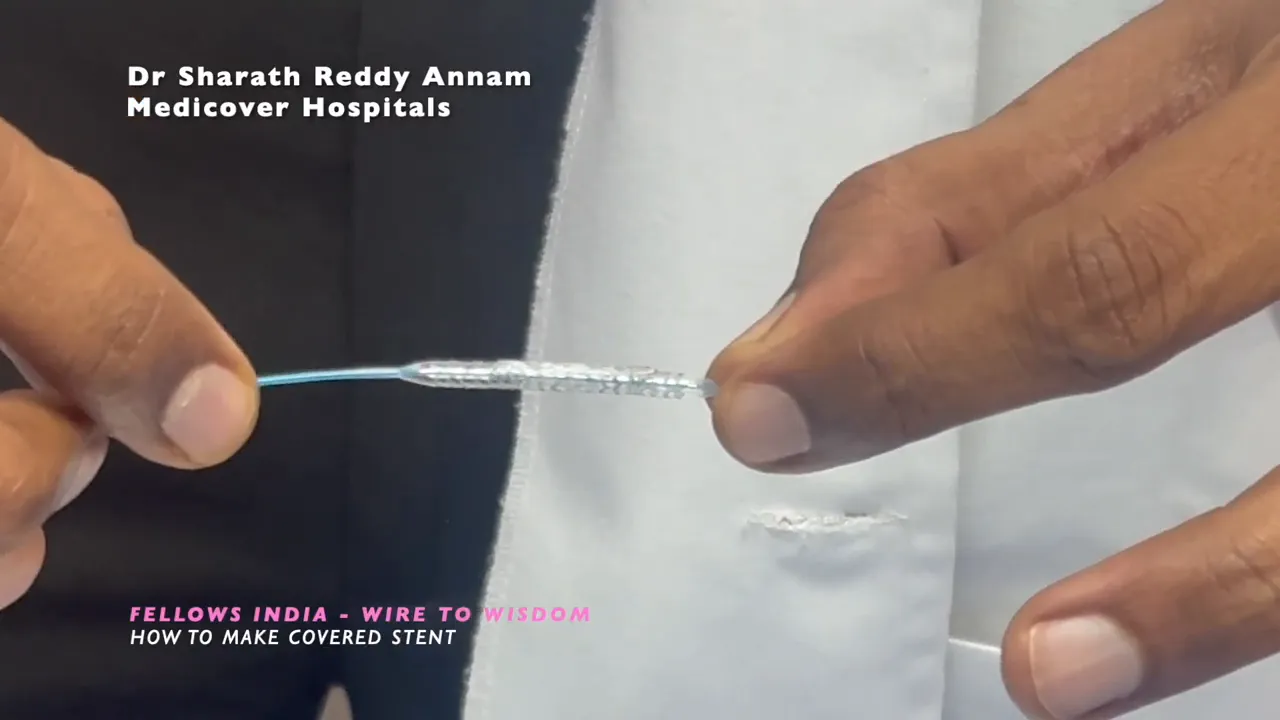
27 Jan How to Make a Covered Stent: Live Bailout Technique for Coronary Perforation
The Live Bailout Technique is a pragmatic, on-the-spot method to create a covered stent when a factory-made covered stent is not immediately available in the catheterization laboratory. I use this approach occasionally as an emergency bailout for coronary perforation. The aim is simple: convert two conventional stents and a balloon into a temporary covered stent that will seal the perforation and allow hemostasis while definitive management is arranged.
When and why to use the Live Bailout Technique
This technique is intended for urgent salvage situations—most commonly coronary perforations that require immediate sealing. It is not a routine substitute for purpose-built covered stents, but it can be lifesaving when a dedicated covered stent is not on hand.
Key principles:
- Seal the breach quickly: The shorter outer stent provides the covered layer that must overlap the perforation.
- Maintain vessel size match: Choose stent diameters compatible with artery size—typically 3 mm in many epicardial coronary settings.
- Crimp securely: The outer covered layer must be well-crimped to the inner stent to allow safe delivery.
Equipment and materials
- Two compatible stents of the same diameter (commonly 3 mm) but different lengths: one short (example 16 mm) and one longer (example 28 mm).
- One stent mounted on a balloon with balloon material beneath the stent (this balloon material will be used as the covering).
- Scissors or a fine cutting instrument suitable for trimming the balloon under sterile conditions.
- Crimper or manual technique to crimp the outer stent onto the inner stent.
- PTCA wire and standard delivery equipment.
Step-by-step Live Bailout Technique
1. Select stents and inspect
Choose two stents that fit the artery diameter. In my practice I commonly use 3 mm stents. The shorter stent will act as the covered portion; the longer stent becomes the inner support. For the demonstration I used a 16 mm short stent and a 28 mm long stent.
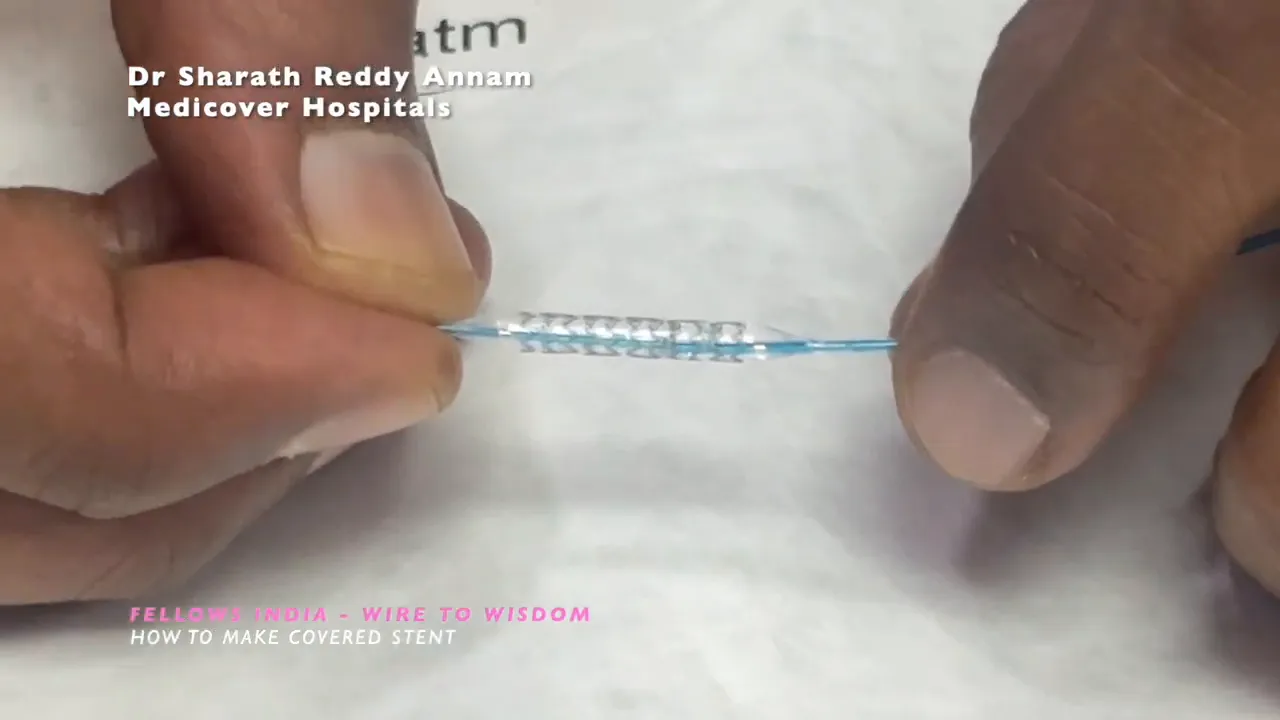
2. Prepare the balloon covering
Fully inflate the balloon under the outer stent to expose and stretch the balloon material that sits beneath the stent frame. This balloon film will act as the covered layer once trimmed and retained under the outer stent.
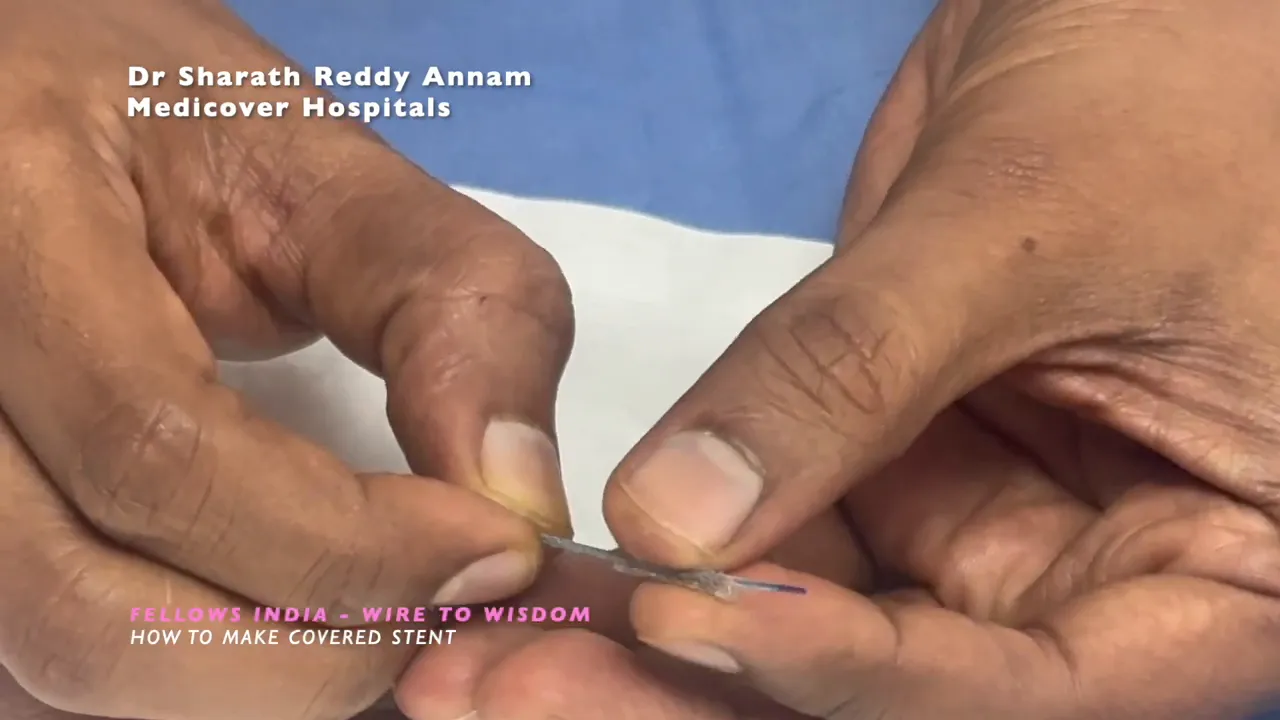
3. Trim the balloon material
Using fine scissors, carefully cut the balloon material on either side of the stent. The goal is to remove the central lumen of the balloon while leaving the balloon sheath attached to the stent frame. Do this under sterile conditions and good lighting.
4. Remove the central balloon lumen
After cutting, remove the central portion of the balloon lumen so you are left with the balloon film adhered beneath the stent frame. This film functions as the covered layer when the stent is deployed.
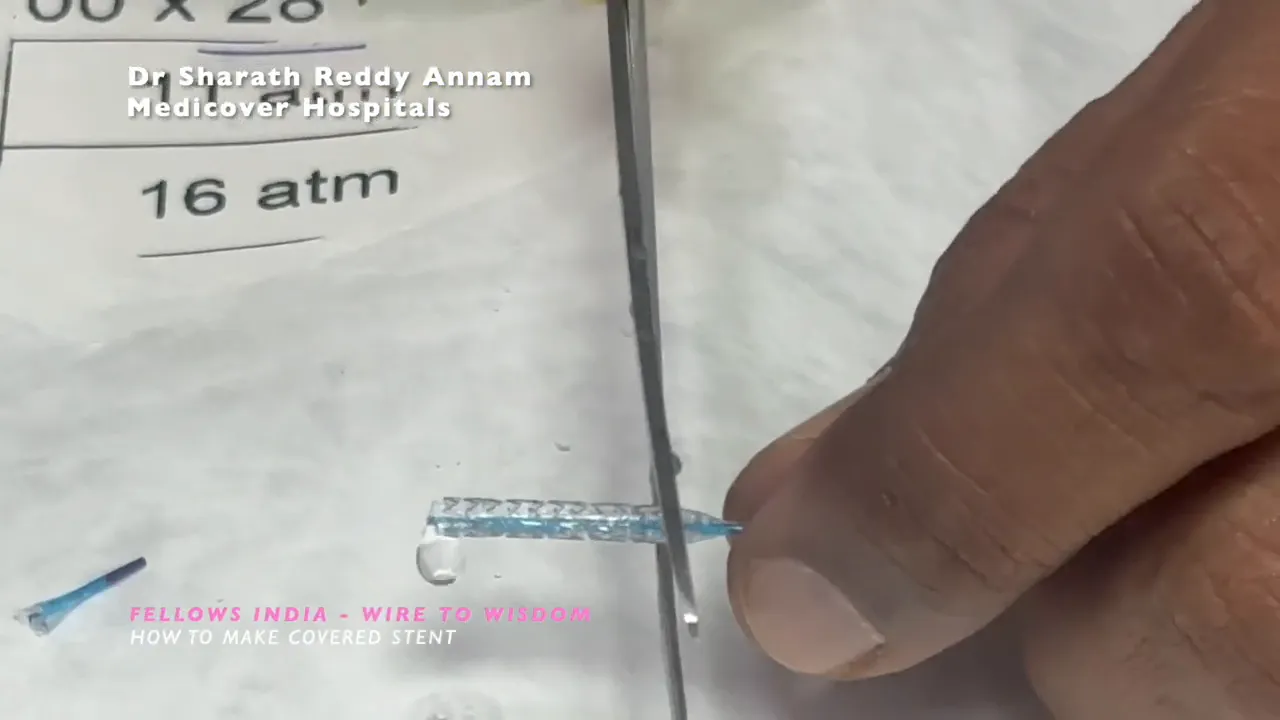
5. Mount the inner (longer) stent
Now take the longer stent (the inner support, for example 28 mm) and slide it over the prepared short covered stent assembly. The longer stent should be introduced so it becomes the inner scaffold and the shorter stent with its balloon film remains the outer covered element.
6. Crimp the outer stent onto the inner stent
Crimp the shorter outer stent securely onto the longer inner stent. The aim is to produce a single delivery unit where the outer stent—with its balloon film—remains the only covered portion. Confirm that the covered region of the assembled stent corresponds to the intended target (the perforation zone).
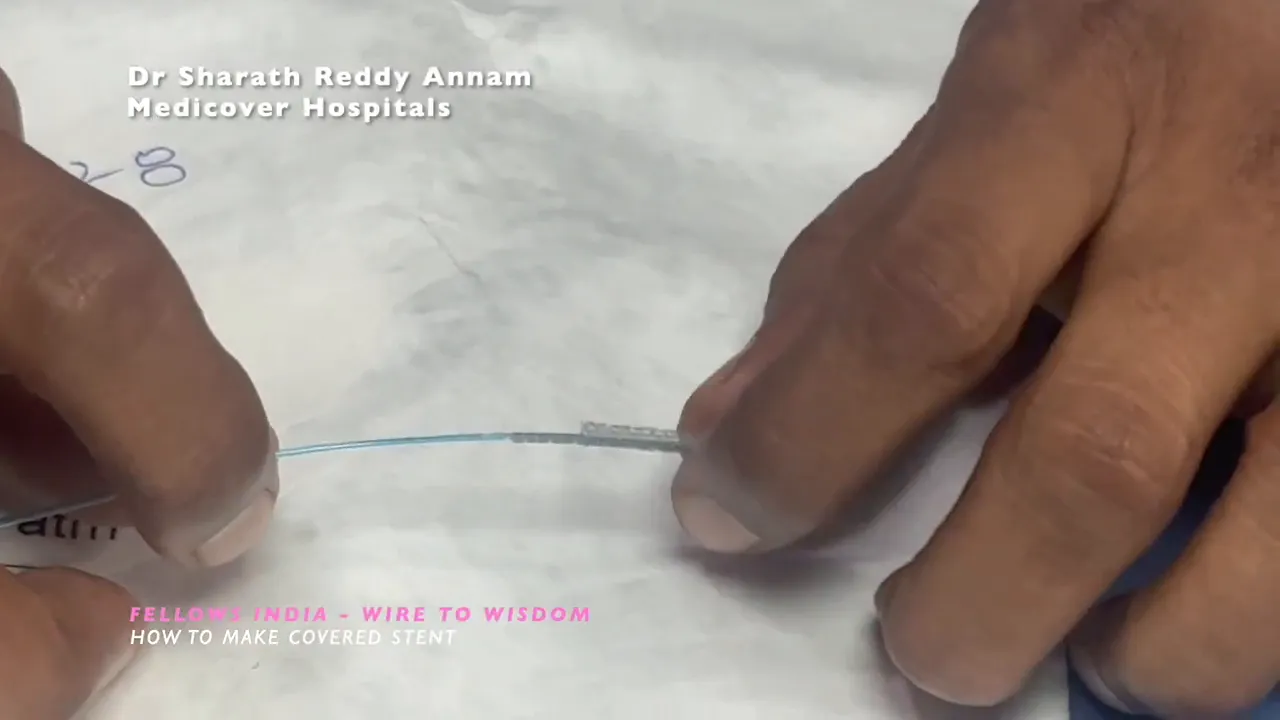
7. Deliver to the target lesion
Advance the assembled stent on your PTCA wire to the site of perforation. Position carefully so the shorter outer covered portion fully overlaps the perforation. Remember that the covered portion is only the outer stent—size and length selection must ensure complete coverage of the breach.
8. Deploy and confirm
Deploy the stent as you would normally. Once released, deflate the balloon and withdraw equipment. Confirm sealing of the perforation angiographically and by hemodynamic assessment. In the demonstration the covered area was clearly sealing the perforation after deployment.
Practical tips and pearls
- Plan sizing carefully. The shorter outer stent must fully cover the perforation; the inner stent must be long enough to provide radial support and allow delivery through tortuous anatomy.
- Work cleanly. Maintain strict sterility when modifying devices. Cutting and manipulation outside normal use is off-label and must be done with caution.
- Confirm coverage before deployment. Re-check alignment so the covered portion sits squarely over the tear.
- Have backup strategies ready. Prepare for prolonged procedural time, potential need for pericardiocentesis, reversal of anticoagulation, or transfer for surgery if needed.
Contraindications and cautions
This is an emergency bailout measure. Modifying devices is off-label and carries risks, including device failure, embolization of components, or incomplete sealing. Use only when the clinical situation justifies improvisation and when no immediately available covered stent exists. Team communication and informed judgement are essential.
Troubleshooting
- If the assembled unit cannot be delivered because of bulk, consider upsizing the guide or adjusting the access route.
- If the covered layer does not deploy cleanly, do not overdilate aggressively—evaluate the risk of propagation of rupture and consider alternative management.
- If angiographic sealing is incomplete, consider additional balloon tamponade, further stenting, or urgent surgical consultation.
FAQ
What exactly is the Live Bailout Technique?
The Live Bailout Technique is an improvised method to create a covered stent by combining two conventional stents and the balloon material beneath one stent to produce a covered segment. It is used as an emergency solution to seal coronary perforations when a premanufactured covered stent is not available.
Which stent sizes work best?
Stent diameter should match the artery—commonly 3 mm in many epicardial coronaries. Use a shorter outer stent to act as the covered segment (for example 16 mm) and a longer inner stent (for example 28 mm) for delivery and support. Exact sizes depend on the vessel and the perforation location.
Is this technique safe and approved?
Modifying devices is off-label and not a substitute for purpose-built covered stents. The technique carries additional risks and should be reserved for emergency bailout situations where the benefits outweigh the risks and no approved covered stent is immediately available.
What are the most common complications?
Potential complications include incomplete sealing, device failure, embolization of modified components, and further vessel injury. Always prepare for pericardial drainage and surgical backup if required.


No Comments