24 Sep Coronary PCI with an Indegenous IVL: Lithotripsy and Luminal Insight
Coronary PCI with an Indegenous IVL is becoming an essential strategy for tackling heavily calcified coronary lesions. In this article I, representing Interventional Strategies, describe our practical experience, device characteristics, imaging-guided decision making, and case-based outcomes using a locally produced intravascular lithotripsy (IVL) catheter. This piece synthesizes procedural detail, imaging findings, tips on sizing and activation, and real-world clinical vignettes to help operators incorporate this tool into their calcified lesion toolkit.
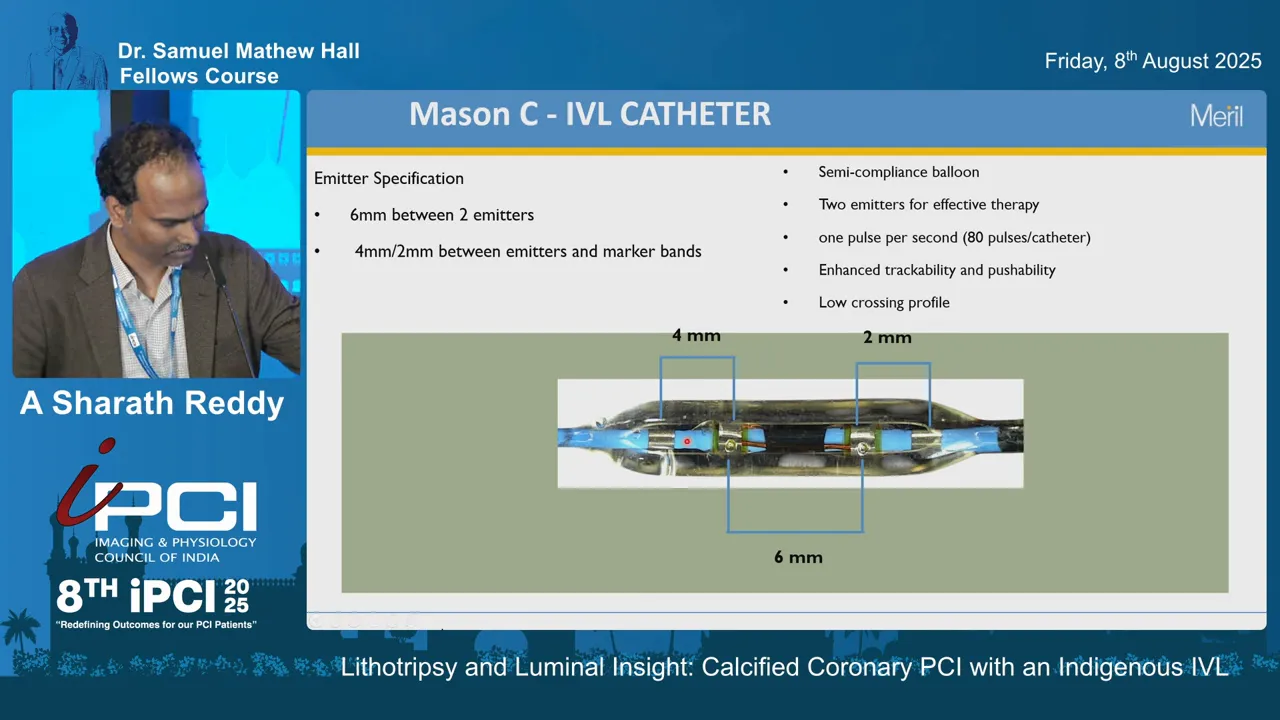
Table of Contents
- Outline
- Introduction: Why Coronary PCI with an Indegenous IVL?
- Device Description and Key Specifications
- Mechanism of Action: Sonic Pressure Waves and Calcium Fracture
- Procedure Setup: Practical Steps for Coronary PCI with an Indegenous IVL
- Case Examples and Imaging-Guided Outcomes
- Device Sizing: Principles and Practical Tips
- When to Combine IVL with Atherectomy
- Role of Imaging: How IVUS/OCT Fine-Tunes Decisions
- Limitations, Logistics, and Availability
- Conclusion and Practical Takeaways
- FAQ: Frequently Asked Questions about Coronary PCI with an Indegenous IVL
- Final Words
Outline
- Introduction and rationale for IVL in calcified coronary lesions
- Device description and specifications
- Mechanism of action: how intravascular lithotripsy works
- Procedure setup and activation protocol
- Case series and imaging examples
- Device sizing and practical tips
- When to use IVL alone or in combination with atherectomy
- Limitations, logistics, and availability
- Conclusion and takeaways
- FAQ: common questions about Coronary PCI with an Indegenous IVL
Introduction: Why Coronary PCI with an Indegenous IVL?
Calcified coronary lesions remain one of the toughest challenges in percutaneous coronary intervention (PCI). Underexpanded stents, suboptimal luminal gain, and higher rates of restenosis and thrombosis are all linked to inadequate modification of calcified plaque. That is why Coronary PCI with an Indegenous IVL has gained interest: it offers a different, less traumatic way to modify calcium using sonic pressure waves rather than high-speed rotational or orbital devices alone.
In our hands at Interventional Strategies we evaluated an indigenously produced IVL catheter designed to mirror established devices but with local manufacturing advantages. We focused on device mechanics, crossing profile, pulse count, sizing nuances — including unique quarter sizes — and how intravascular imaging guided our choice and assessed outcomes.
Device Description and Key Specifications
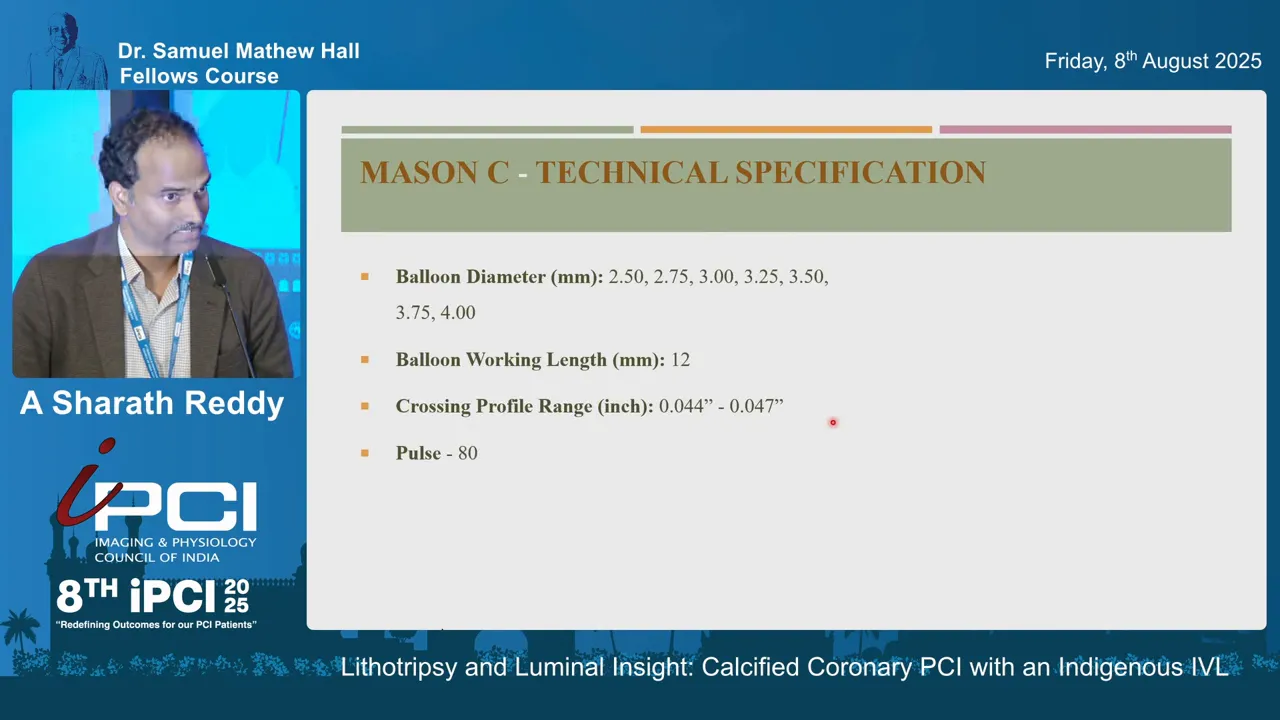
The indigenously manufactured IVL catheter we used is conceptually similar to international IVL balloons. Key physical and operational features are:
- Two emitters positioned within a semicompliant balloon. The distal emitter lies approximately 4 mm from the distal radiopaque marker and the proximal emitter is ~2 mm from the marker, with a 6 mm separation between emitters.
- Overall balloon working length around 12 mm (active segment where emitters are located).
- Semicompliant balloon material allowing for some conformity to vessel shape during inflation.
- Available pulse settings: standard units deliver 80 pulses; some models (Pro C) offer up to 120 pulses for extended treatment.
- Crossing profile details: up to 3.0 mm balloons have a profile compatible with 0.044″ guidewire lumen; balloons beyond 3.0 mm have slightly larger crossing profile comparative to 0.047″.
- Compatibility: designed to be used via 6 French guide catheters and with guide catheter extensions exceeding 5.5 French.
- Availability of quarter-size balloons (e.g., 2.25, 2.75 mm increments). These quarter sizes aid precise sizing in borderline vessels, though initial access to quarter sizes may be limited in some settings.
The manufacturer has also provided an updated generator and activator setup. Instead of hand-held activation, the system uses a connector coupled to a generator with a foot-pedal activator. This change improves operator ergonomics and allows hands-free initiation of pulse sequences during balloon inflation.
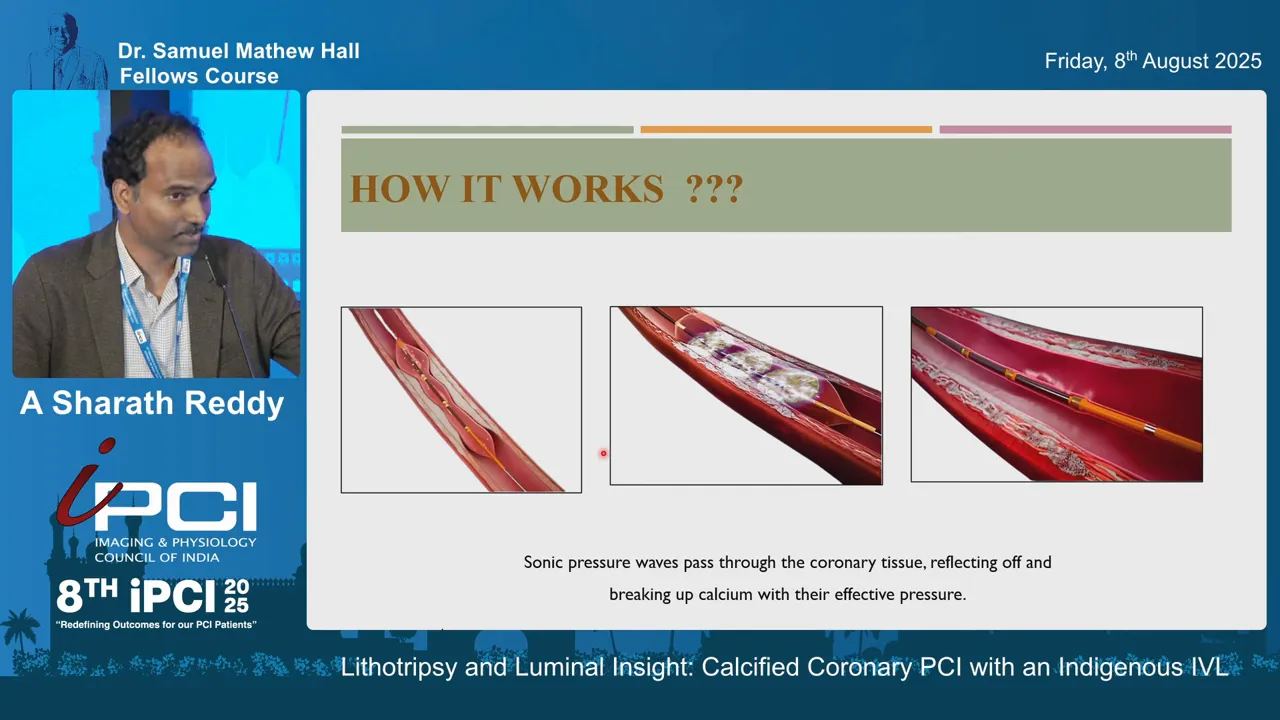
Mechanism of Action: Sonic Pressure Waves and Calcium Fracture
Intravascular lithotripsy does not ablate tissue mechanically like atherectomy. Instead, it generates localized sonic pressure waves within the balloon-fluid interface. These pressure waves propagate through the vessel wall and are transmitted more effectively through incompressible calcified plaque than through soft tissue. The resulting stress leads to microfractures in intimal and medial calcium, increasing vessel compliance and facilitating subsequent balloon expansion and stent deployment.
Practically, the effective impact resembles delivering a transient local pressure equivalent to approximately 50 atmospheres at the level of the calcified plaque — not to be confused with the actual balloon inflation pressure. Operators typically inflate the balloon to a low working pressure (around 4 atmospheres) to ensure balloon apposition while minimizing barotrauma, activate pulses, and may transiently increase to 6 atmospheres during activation cycles before deflating.
Typical Activation Parameters
- Initial inflation: around 4 atmospheres to appose the balloon to the vessel wall without over-stretching.
- Pulse cycles: activated in runs (e.g., up to 80 pulses; Pro C offers 120 pulses if needed).
- Transient pressure increment: operators may raise inflation to 6 atmospheres during activation, then return to baseline.
- Rated burst pressure (RBP): the balloon RBP is approximately 10 atmospheres for the devices we used; operators must not exceed RBP.
Procedure Setup: Practical Steps for Coronary PCI with an Indegenous IVL
Here is the practical workflow we use when planning and performing Coronary PCI with an Indegenous IVL:
- Pre-procedure assessment: collect angiographic views and, where possible, intravascular imaging (IVUS or OCT) and CT if available to determine calcium distribution, thickness, and circumferential extent.
- Guide and access selection: choose a 6 French or larger guiding catheter when possible to support device delivery. Ensure guide extension compatibility if planned.
- Lesion crossing: pass a workhorse wire or dedicated support wire. If lesion is uncrossable, consider upfront atherectomy (rotational or orbital) to create an initial channel.
- Device selection: choose IVL balloon diameter based on minimal lumen diameter (MLD) and target vessel size; we frequently size the IVL 0.25–0.5 mm smaller than the reference vessel diameter to target the minimal lumen in eccentric lesions and to avoid excessive trauma.
- Inflation and activation: inflate to ~4 atmospheres, activate in pulse sequences, consider transient increases to 6 atmospheres, complete 80–120 pulses as required, then deflate.
- Post-IVL assessment: perform angiography and intravascular imaging to visualize calcium fractures and reassess luminal gain; proceed with predilatation and stent implantation as indicated.
Using this workflow allows safe, staged plaque modification. In several of our cases we used IVL after initial rotablation to further modify deep or circumferential calcium that remained noncompliant following atherectomy.
Case Examples and Imaging-Guided Outcomes
The best way to appreciate the value of Coronary PCI with an Indegenous IVL is through case-based examples. Below I present three representative cases highlighting decision-making, imaging findings, and final results.
Case 1: 360° Proximal LAD Calcification with Small Vessel
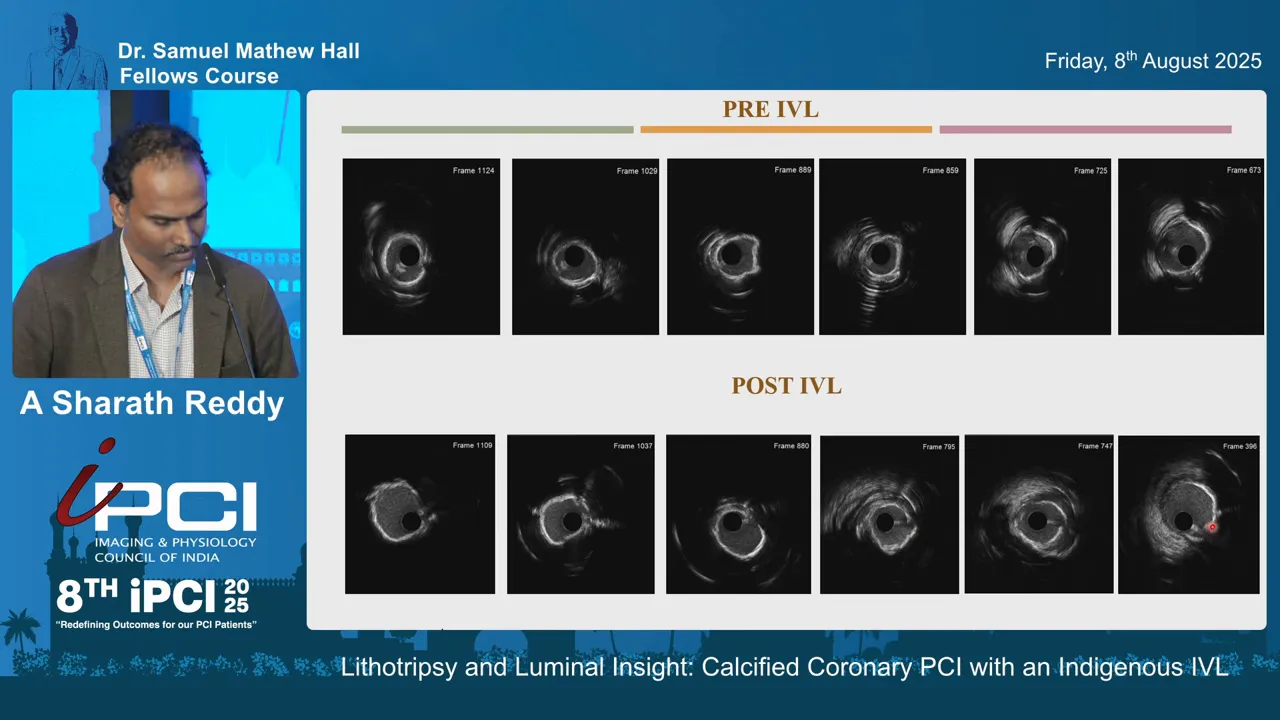
Clinical scenario: heavily calcified proximal LAD with severe concentric (360°) calcification confirmed on CT and IVUS. The lesion did not permit easy crossing initially, so we performed initial rotablation with a 1.5 mm burr to create a channel.
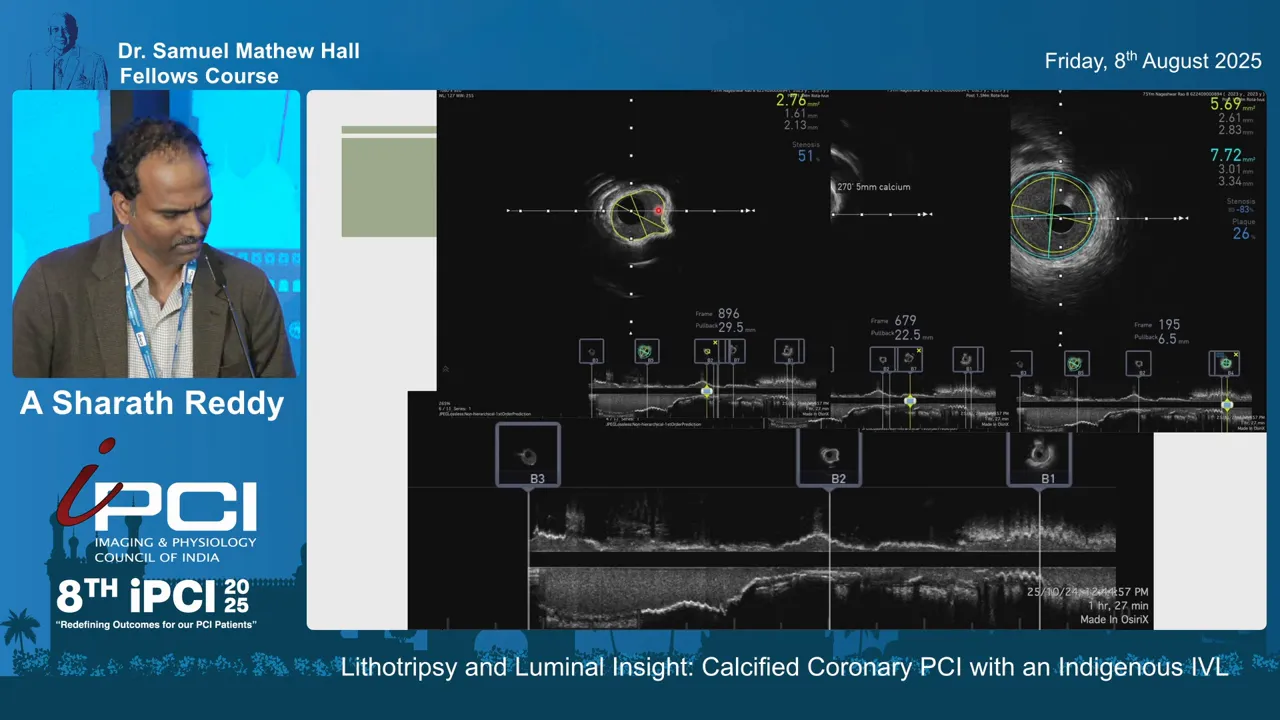
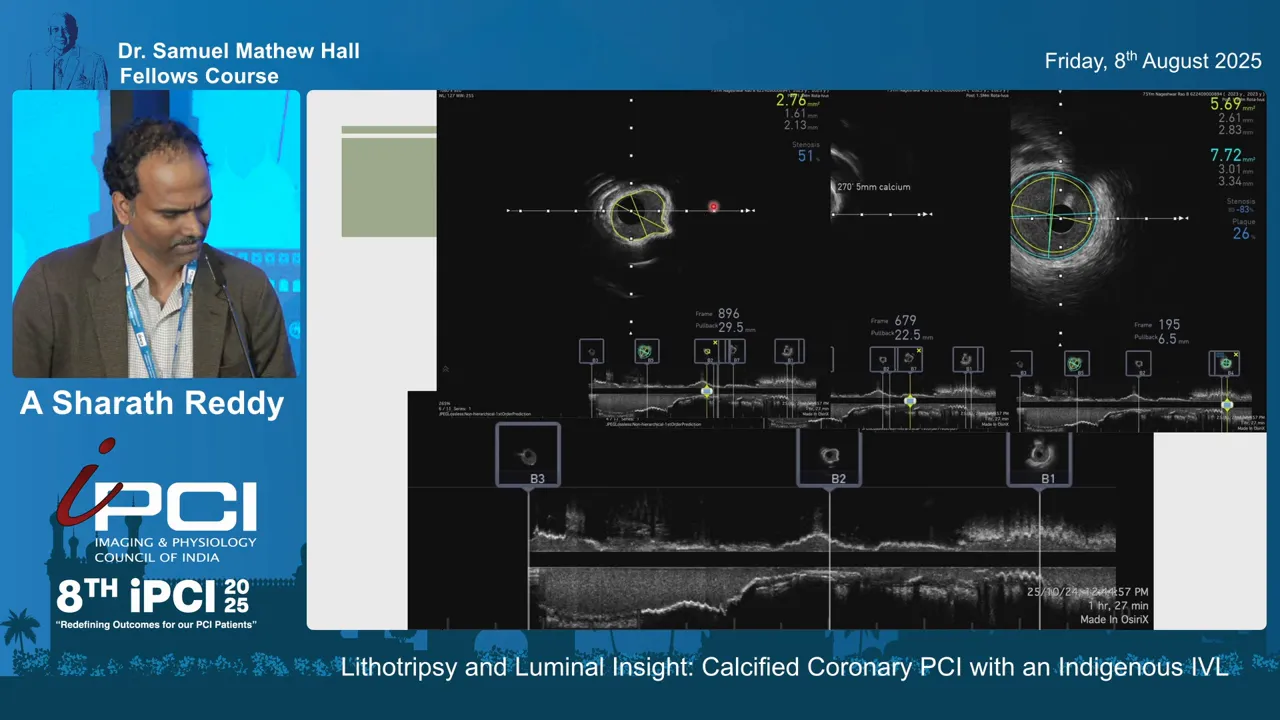
Findings after rotablation: despite the burr, IVUS showed persistent 360° calcium with a minimal lumen area (MLA) of approximately 2.76 mm² and a vessel diameter in the region around 3.1 mm. Calcification length and circumferential involvement corresponded to a high calcium score (score of 3 in our grading system).
IVL strategy: we chose a 2.75 mm IVL balloon for a vessel that measured 3.2 mm by reference. Note our sizing philosophy: we preferred an IVL slightly smaller (about 0.5 mm less) than the external reference to target the minimal lumen rather than over-dilating against rigid calcium.
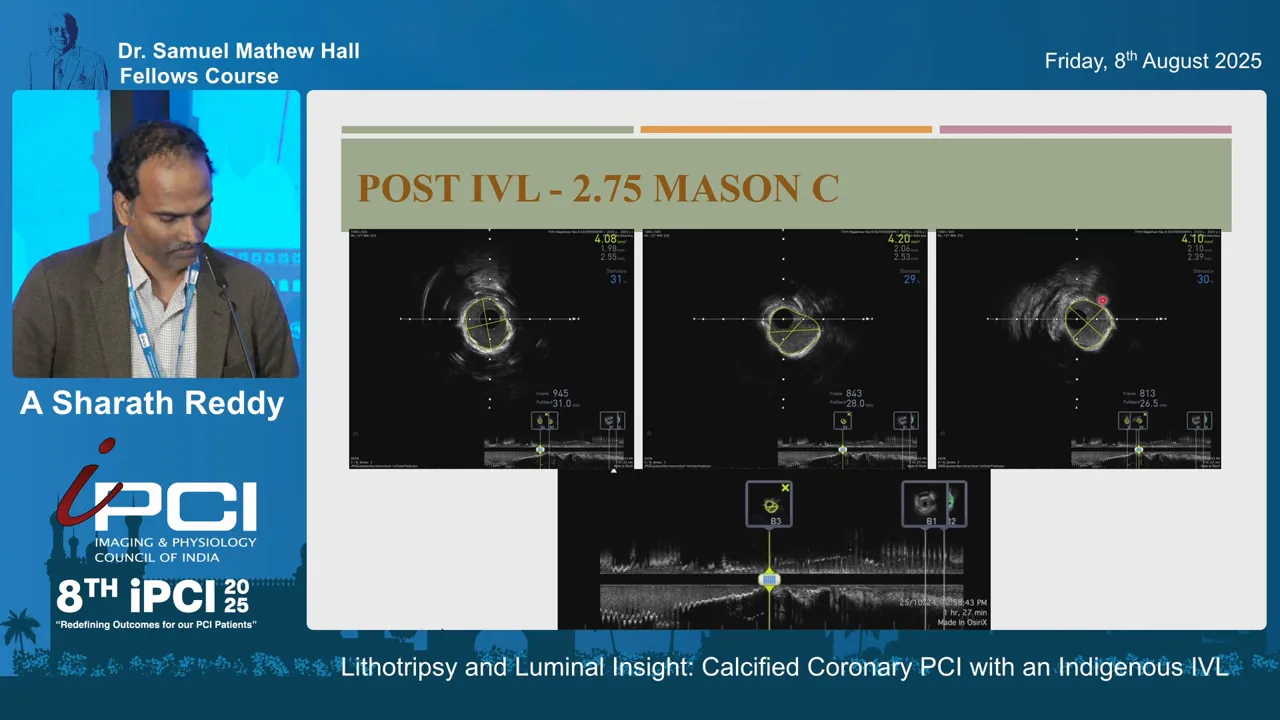
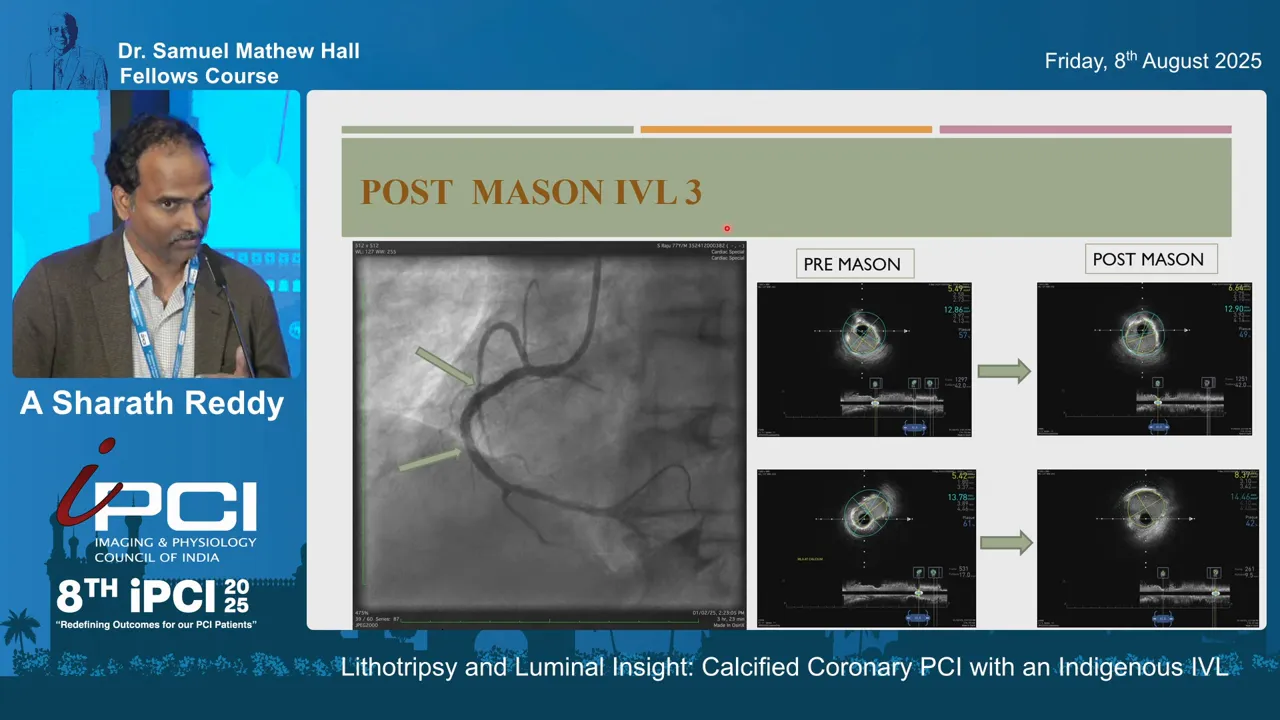
Result: IVUS after IVL showed clear evidence of calcium fractures and almost a doubling of the lumen area — MLA increased from roughly 2.76 mm² to over 4.2 mm² in segments evaluated. After stenting and post-dilation, MSAs were greater than 100% of the distal reference (values like 6.9, 6.3, and 7.5 reported for segments), translating into an excellent angiographic and intravascular appearance.
Case 2: Long, Concentric Calcified Segment in Large Vessel
Clinical scenario: a long segment of 360° calcification in proximal vessel with vessel diameter near 3.5 mm. IVUS confirmed extensive circumferential calcium across a long segment.
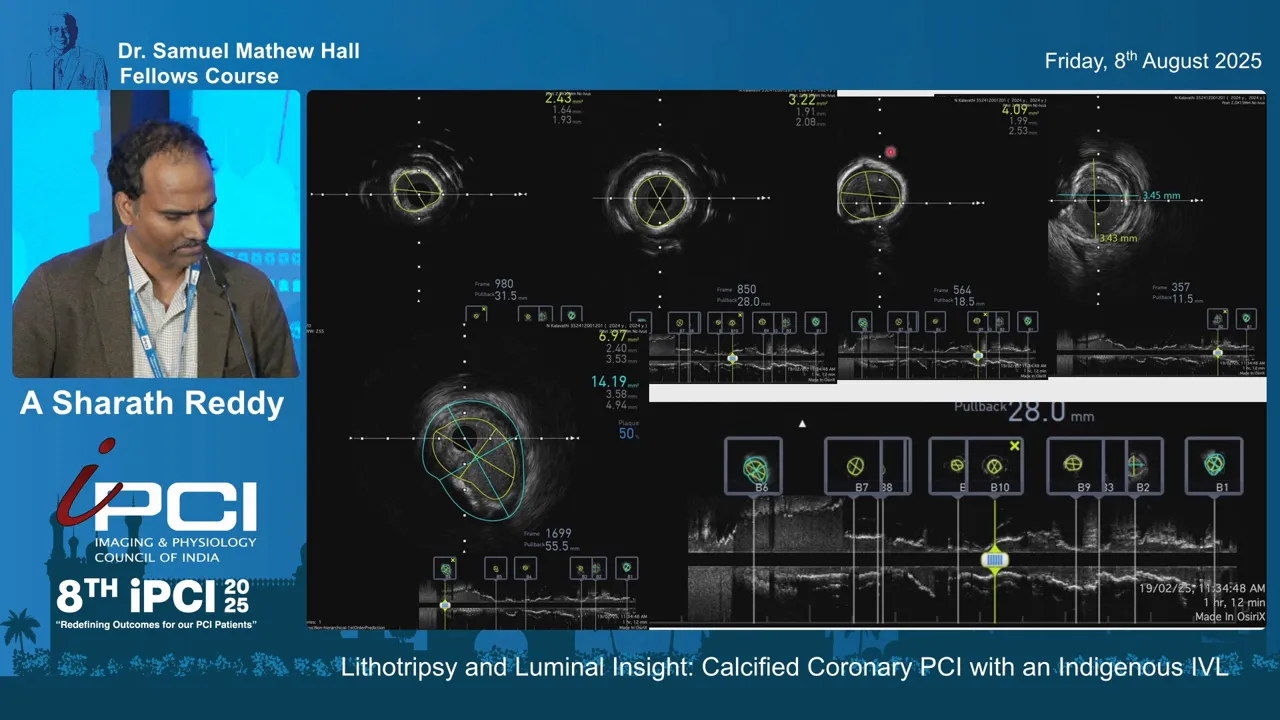
IVL strategy: selected a 3.0 mm IVL balloon (chosen because the external measurement was 3.5 mm). We delivered the IVL pulses across the long segment — multiple frames demonstrated fractures in at least two to three locations per segment following treatment.
Result: IVUS documented multiple calcium fractures and a significant increase in luminal area. After stenting, the final expansion measurements indicated satisfactory stent apposition and luminal gain. The case reinforced the utility of IVL for long, concentric lesions where atherectomy alone might not produce fractures deep in medial calcium.
Case 3: Underexpanded Stent in Right Coronary Artery (77-year-old patient)
Clinical scenario: prior stent deployment in RCA that appeared acceptable angiographically but was underexpanded when assessed by intravascular imaging. Distal reference lumen measurements and points within the stent showed MSAs around 5.4–5.6 mm² in parts and a proximal stent area near 7.7 mm², indicating heterogeneity and an eccentric/oval stent shape.
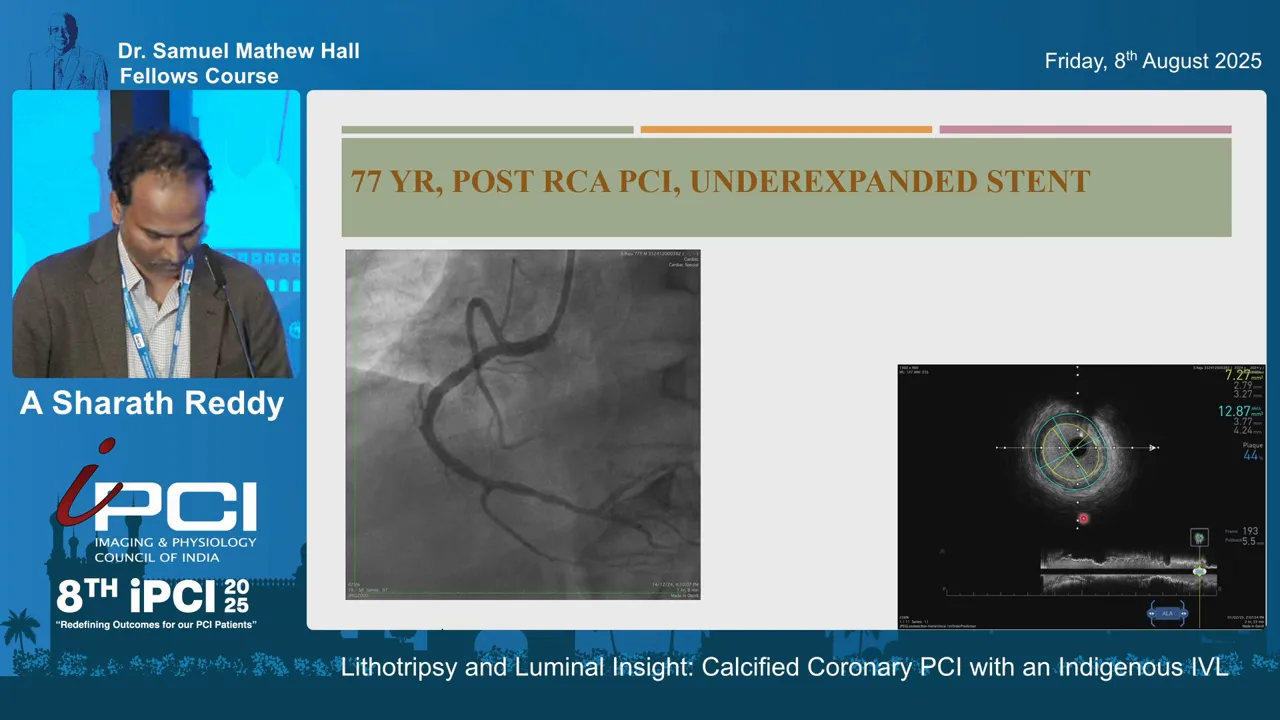
IVL strategy: instead of sizing to the maximum stent diameter or the external reference, we selected a 3.5 mm IVL balloon sizing to target maximal expansion of the minimal lumen area. The principle is to address the underexpanded portions — we aim for maximal minimal area improvement, not oversizing against a rigid stent frame.
Result: after IVL, the stent MSA at the previously minimal site increased from 5.4 mm² to 8.3 mm² — roughly a 1.5-fold increase. The stent shape became more circular and expansion was substantially improved. This case underscores how imaging-guided IVL can rescue an underexpanded stent safely without aggressive high-pressure ballooning alone.
Device Sizing: Principles and Practical Tips
Sizing is one of the most important determinants of success in Coronary PCI with an Indegenous IVL. Here are the principles we follow:
- Target the minimal lumen diameter/area in eccentric lesions: select an IVL balloon that is roughly 0.25–0.5 mm smaller than the reference vessel diameter. This helps focus the sonic energy where it is most needed and reduces the risk of over-pressurizing against rigid calcified segments.
- In concentric 360° calcification, an IVL balloon closer to the reference diameter can be selected because the entire circumference will be treated, but still avoid oversizing beyond RBP limits.
- Use quarter sizes when available for precise matching. The indigenous device’s quarter sizes (e.g., 2.25, 2.75 mm) are advantageous for borderline vessels. Though availability may be limited initially, expect wider access to these sizes over time.
- If an underexpanded stent is present, size to address the minimum stent area rather than the maximum stent diameter — aim to open the tightest segment first.
Practical tip: always confirm your sizing plan with intravascular imaging if available — IVUS and OCT provide the most direct measure of calcium distribution, thickness, and luminal dimensions.
When to Combine IVL with Atherectomy
IVL and atherectomy are complementary, not mutually exclusive. Key scenarios where combination therapy is reasonable:
- Uncrossable lesions: if you cannot deliver an IVL balloon due to severe stenosis, perform rotational or orbital atherectomy first to create a channel.
- Heavily concentric, thick calcium: atherectomy can remove superficial calcium to improve deliverability; IVL can then create deeper medial fractures to increase compliance.
- Post-atherectomy residual rigidity: if a burr achieves luminal gain but intravascular imaging still shows persistent circumferential calcium or insufficient plaque modification, IVL may add incremental benefit.
In our practice, in the first presented case we used a 1.5 mm burr for initial lesion debulking and then applied IVL to achieve deeper fracture and luminal expansion. This staged and tailored approach maximized safety while achieving substantial gains in lumen area.
Role of Imaging: How IVUS/OCT Fine-Tunes Decisions
Intravascular imaging is central to modern calcified-lesion PCI and is especially valuable when planning Coronary PCI with an Indegenous IVL. Imaging helps in several ways:
- Assess calcific distribution: determine whether calcium is focal vs long, eccentric vs concentric, and measure thickness and arc (e.g., >180° or 360°).
- Calculate calcium score: imaging-derived scores help predict the need for plaque modification.
- Guide device sizing: choose IVL balloon diameter and determine whether atherectomy is required first.
- Assess treatment adequacy: post-IVL imaging demonstrates calcium fractures, quantifies luminal gain, and assists in final stent sizing and post-dilation decisions.
We routinely perform pre- and post-IVL imaging to visualize fracture lines and document MSAs. Imaging-driven workflows consistently produce better expansion and reduce the risk of underexpanded stents.
Limitations, Logistics, and Availability
While Coronary PCI with an Indegenous IVL offers compelling advantages, operators should be aware of limitations:
- Deliverability: although the crossing profile is reasonable, severely stenotic uncrossable lesions may still require atherectomy or high-support wires for initial passage.
- Pulses and time: delivering up to 80–120 pulses takes time and repeated inflation cycles; plan procedural time accordingly.
- Availability of quarter sizes: these are valuable for precise sizing, but initial distribution of quarter-size balloons may be limited in some settings.
- Cost and inventory considerations: as with any specialized device, balance clinical benefit and institutional budget when integrating IVL into your practice.
Logistics of the indigenously produced system: it uses a generator and foot-pedal activator which many operators find ergonomic. The system’s compatibility with 6 French guides and guide extension catheters (≥5.5 F) is helpful for transradial approaches, which are increasingly preferred for coronary procedures.
Conclusion and Practical Takeaways
Calcified lesions require thoughtful plaque modification to avoid stent underexpansion and its consequences. Coronary PCI with an Indegenous IVL is a practical, imaging-friendly addition to the calcium modification armamentarium. Key takeaways from our experience:
- IVL produces sonic pressure waves that create calcium fractures and increase vessel compliance, often doubling or substantially improving minimal lumen area when used appropriately.
- Sizing matters: target the minimal lumen and use quarter sizes when necessary; typically choose an IVL balloon mildly undersized relative to the reference diameter.
- Combine IVL with atherectomy when needed — e.g., uncrossable lesions or when superficial debulking is required for deliverability.
- Intravascular imaging (IVUS/OCT) optimizes decision-making pre- and post-IVL and documents calcium fracture and stent expansion.
- The indigenous IVL system we used is comparable to established devices in pressures, crossing profile, and clinical effect, with additional local manufacturing advantages and quarter-size options.
Calcium modification is the key to preventing stent underexpansion and the downstream clinical consequences. Imaging fine-tunes decision making for both lesion assessment and selection/sizing of devices. Coronary PCI with an Indegenous IVL is another valuable tool in the interventionalist’s toolkit and, in our experience, is particularly useful when combined with careful imaging guidance.
FAQ: Frequently Asked Questions about Coronary PCI with an Indegenous IVL
Q: What is the principal advantage of IVL over high-pressure ballooning?
A: IVL delivers sonic pressure waves that create microfractures in calcified plaque, increasing vessel compliance without subjecting the vessel to excessive focal mechanical stress. High-pressure ballooning alone may risk dissection, perforation, or fail to fracture deep calcium.
Q: When should I choose IVL vs atherectomy?
A: Use IVL when the balloon can be delivered to the lesion and when imaging shows deep or concentric calcium that would benefit from fracture rather than superficial ablation alone. If the lesion is uncrossable or severely superficial calcified plaque blocks device passage, consider atherectomy first, then IVL for deeper fracture.
Q: How do I size the IVL balloon?
A: Size generally 0.25–0.5 mm smaller than the vessel reference to target the minimal lumen, especially in eccentric lesions. Use quarter sizes for fine matching if available. For underexpanded stents, target the minimal stent area rather than the maximum.
Q: How many pulses should I deliver?
A: Most devices offer 80 pulses as a standard treatment bundle. Some models provide up to 120 pulses for extended treatments. Deliver pulses in cycles with inflation at ~4 atmospheres, transient increases to 6 atmospheres during activation if necessary, and do not exceed rated burst pressure (typically ~10 atm).
Q: Can IVL be used via radial access?
A: Yes. The indigenous IVL system is compatible with 6 French guiding catheters and guide extension catheters >5.5 F, making radial access feasible in most cases.
Q: Does IVL cause vessel injury or dissections?
A: IVL primarily fractures calcium and is associated with a favorable safety profile compared with aggressive high-pressure dilation. Standard precautions apply — perform careful imaging and avoid exceeding rated balloon pressures.
Q: Are the quarter sizes essential?
A: Quarter sizes provide greater precision for borderline vessels and reduce the risk of oversizing. They are particularly helpful when managing small vessels or when the difference between two standard sizes is clinically meaningful.
Q: Is IVL a replacement for atherectomy?
A: No. IVL and atherectomy are complementary strategies. Atherectomy removes superficial calcific bulk and helps device delivery, while IVL creates fractures deeper within calcium to increase vessel compliance. The two modalities are often used together for optimal results.
Q: How should I confirm the efficacy of IVL?
A: Use intravascular imaging (IVUS or OCT) to document calcium fractures and measure luminal gain. Imaging helps determine whether additional pulses, adjunctive atherectomy, or further balloon expansion is needed prior to stenting.
Q: What are the main limitations of the indigenous IVL device?
A: Limitations include deliverability in totally occlusive or extremely tight stenoses, availability of quarter sizes in some centers, time required for pulse delivery, and institutional cost/logistics. However, the generator and foot-pedal activation, plus compatibility with 6F guides, make it practical for many labs.


No Comments