22 Apr EVAR in Abdominal Aortic Aneurysm: A Case Study of Small Aorta Management
In today’s lecture, we delve into a unique case of an abdominal aortic aneurysm in a patient with a small aorta. Join me, Dr. Sharath Reddy Annam, as we explore the complexities and intricacies of this procedure, shedding light on the challenges faced and the solutions implemented.
Table of Contents
- Introduction to the Case
- Choosing the Right Graft
- Finalizing the Iliac Extension
- Post-Deployment Assessment
- Balloon Dilation Techniques
- Conclusion and Results
- FAQs
Introduction to the Case
Today, we explore a compelling case that diverges from our usual focus on coronary interventions. This involves a 69-year-old male patient diagnosed with an abdominal aortic aneurysm in a small aorta. The intricacies of managing such a condition, especially in the presence of a small aorta, present unique challenges and learning opportunities.
Patient Background and History
The patient has a history of coronary artery disease, having undergone a PCI to the right coronary artery in 2003. A subsequent bypass surgery included a LIMA to LAD and SVG to RCA. However, by 2017, both grafts had occluded, and he presented with abdominal pain. Further investigations revealed an abdominal aortic aneurysm.
Additional medical conditions include mild LV dysfunction, diabetes, and rheumatoid arthritis, which complicate his surgical options due to increased risks associated with open surgery.
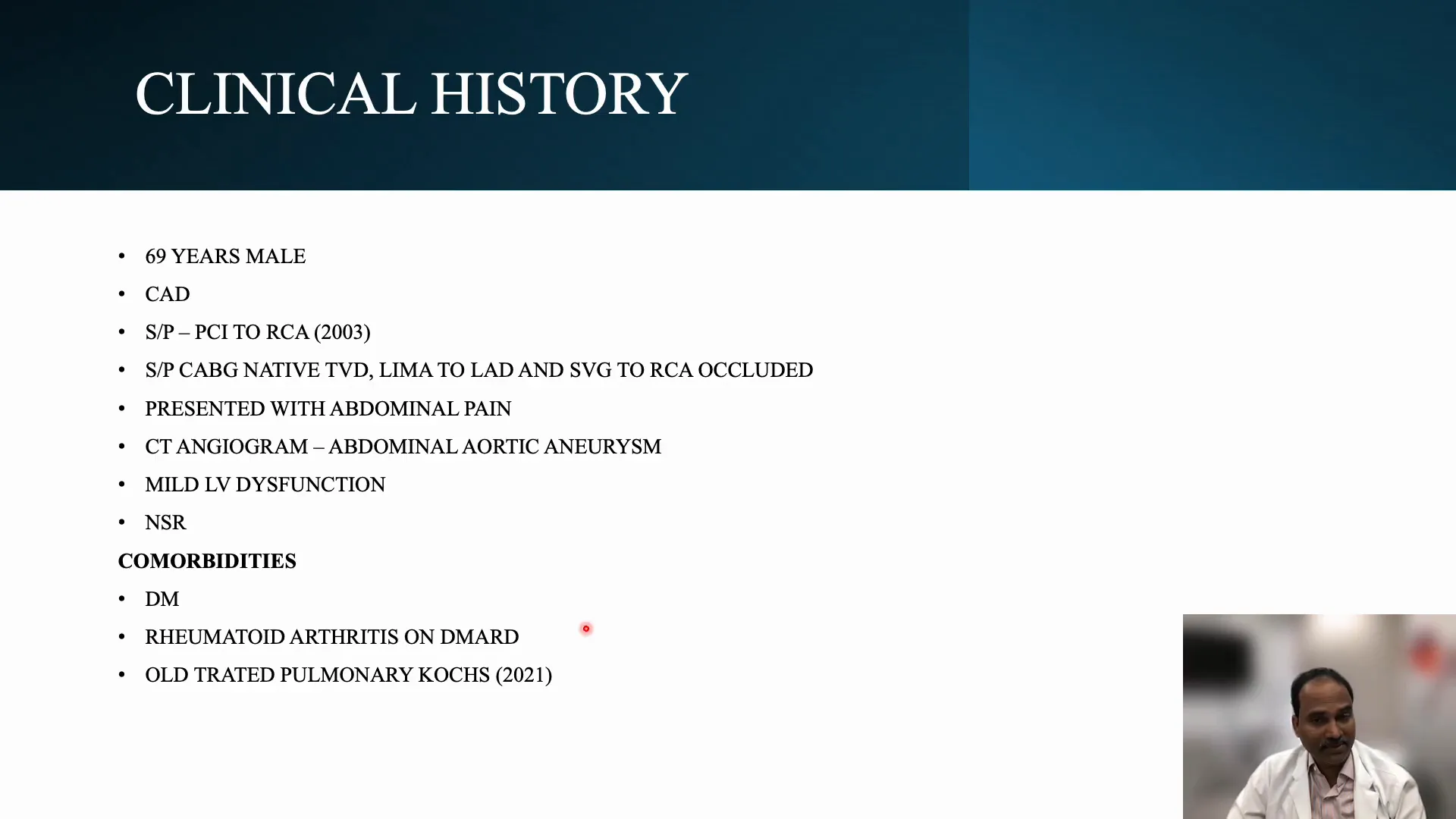
Understanding the Risks
The combination of mild LV dysfunction, failed grafts, and rheumatoid arthritis places the patient at high risk for open surgery. These factors necessitate a careful approach to treatment, emphasizing the need for minimally invasive solutions like EVAR (Endovascular Aneurysm Repair).
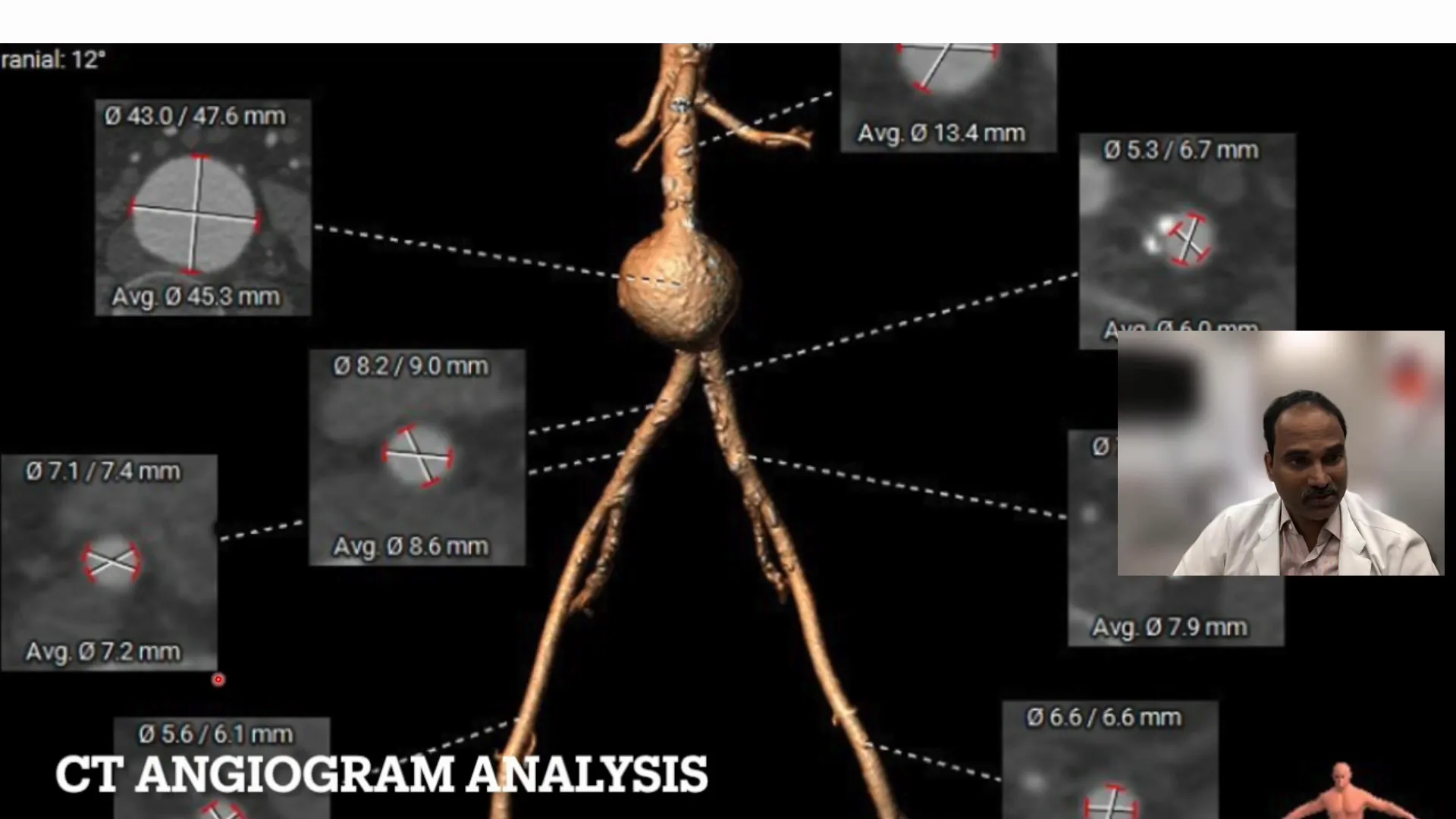
CT Analysis of the Aorta
CT imaging revealed that the abdominal aorta, measured below the renal artery, was around 13.4 mm, classifying it as small. The aneurysm site itself measured 4.5 cm, which is more than three times the size of the aorta. This disproportion necessitates intervention due to the risk of rupture.
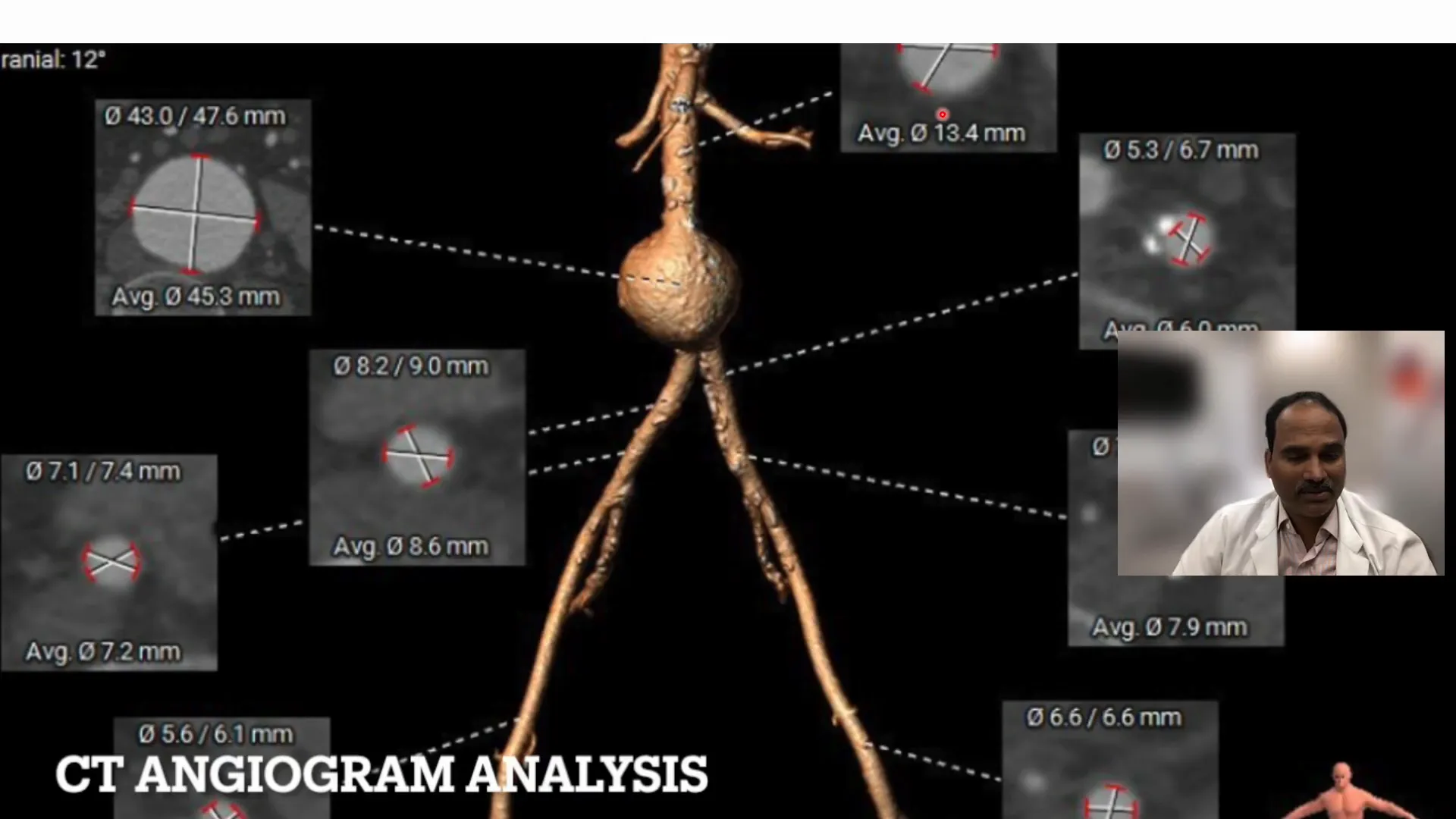
Significance of Aorta Size
A small aorta, defined as less than 18 mm, presents unique challenges in aneurysm repair. The significant size difference between the aneurysm and the aorta demands precise planning to ensure successful intervention without complications.
Iliac Artery Measurements
The iliac arteries were also evaluated, with the right iliac artery measuring 8.6 mm and the smallest segment at 6 mm. The left iliac artery measured 7.9 mm, with the smallest segment at 6.6 mm. The smallest graft available was 23 mm, which influenced the choice of graft size and the decision-making process.
The patient’s complex medical history and unique anatomical features required a tailored approach to aneurysm repair, highlighting the importance of detailed planning and precise execution in interventional cardiology.
Choosing the Right Graft
In our case, selecting the appropriate graft was crucial due to the small size of the aorta. The smallest graft available was 23 mm, which matched the anatomical requirements given the aorta’s size of 14 mm. This choice was pivotal in ensuring proper fit and function.
We evaluated the landing zone and found it to be approximately 3.7 cm, which provided a suitable area for graft deployment. The aneurysm’s extension to the bifurcation was advantageous, allowing for optimal placement of the bifurcated segment of the graft.
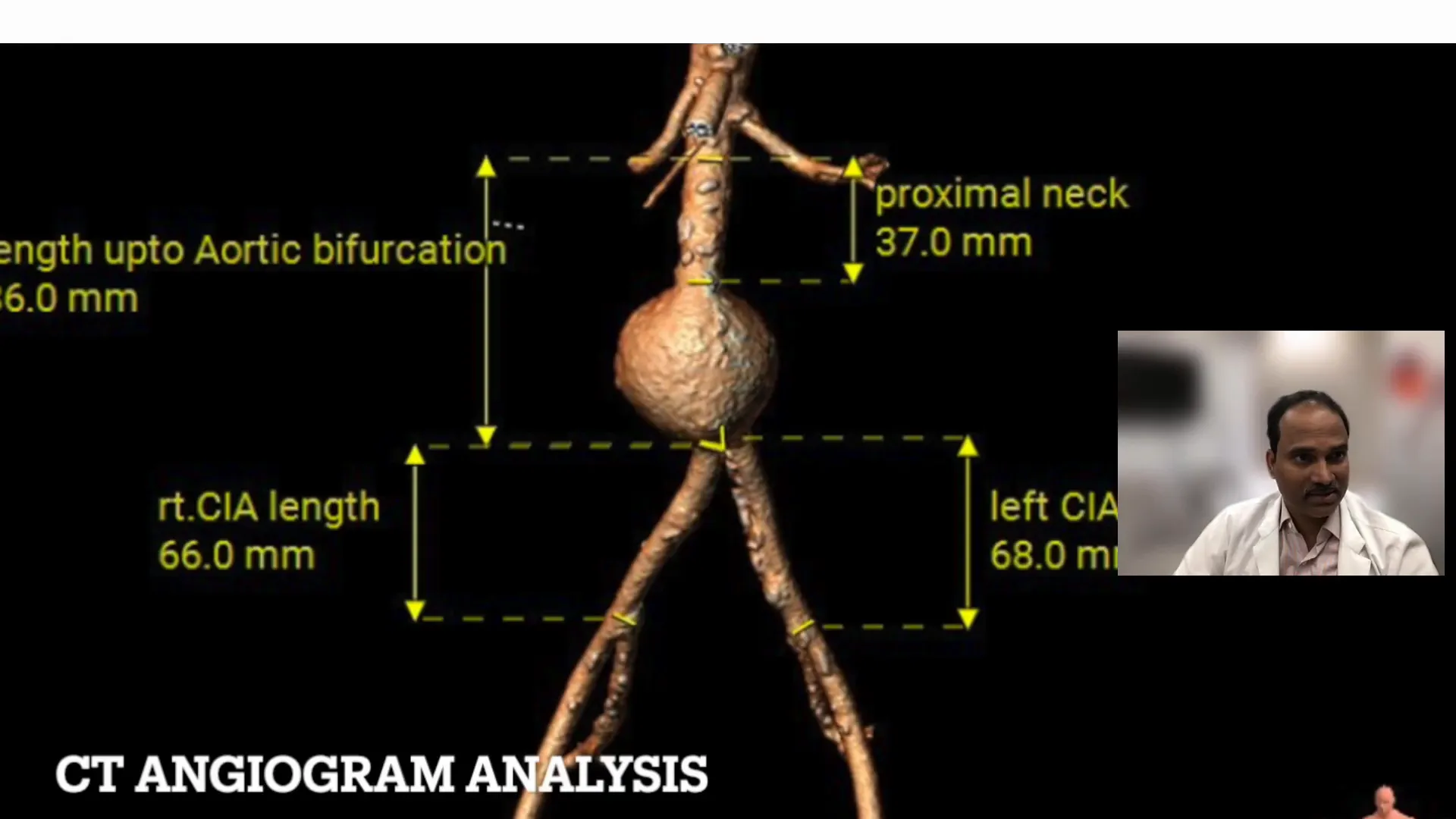
Key Considerations for Deployment
Deploying the graft required meticulous planning, especially considering the aneurysm’s proximity to critical anatomical landmarks. Ensuring that the graft’s bifurcation aligned correctly with the aortic bifurcation was essential to avoid complications.
The graft’s contra gate markers needed to be precisely positioned within the aneurysm to facilitate full expansion of the iliac extensions. This careful positioning was a key factor in the procedure’s success.
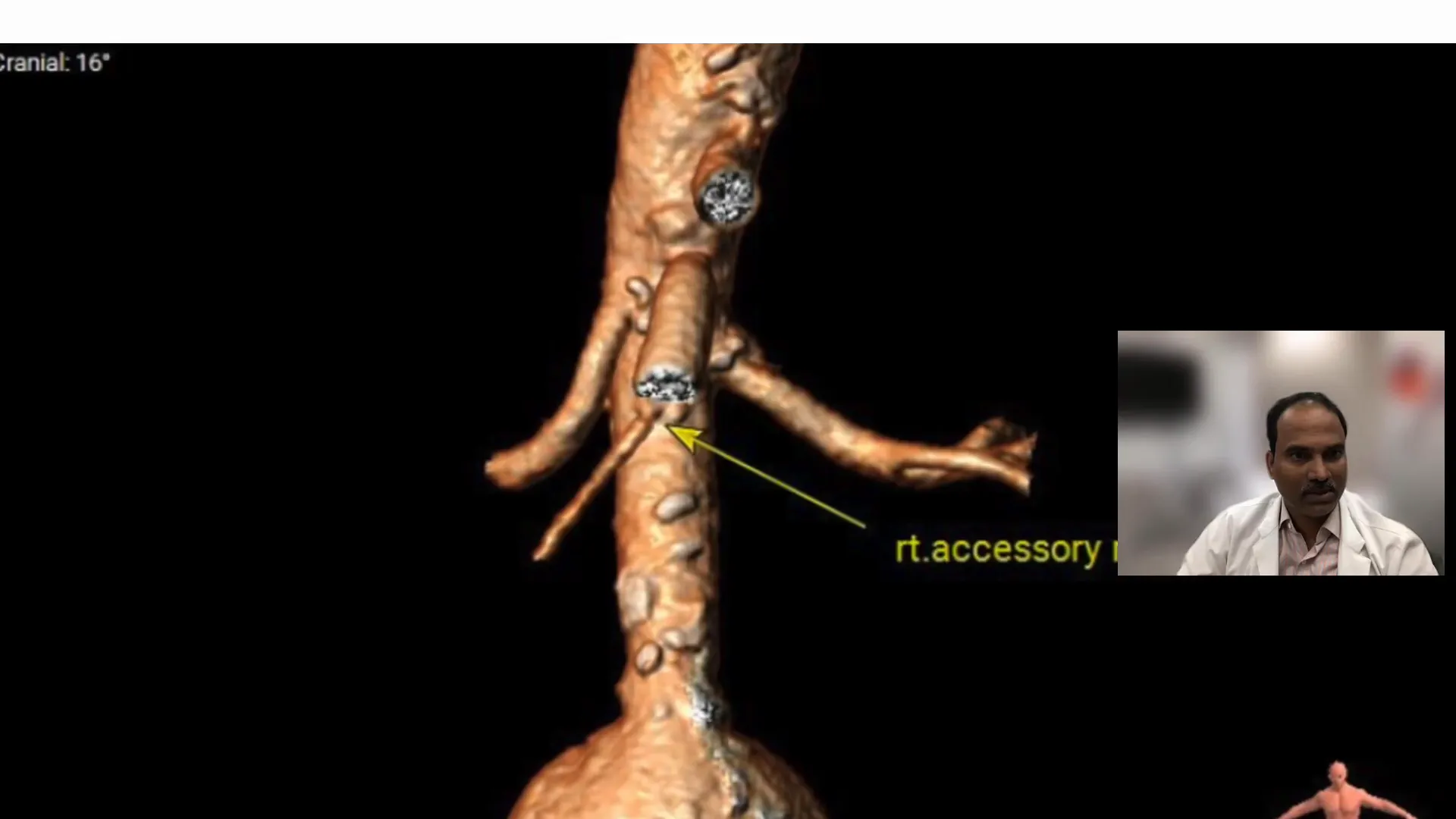
Accessory Renal Artery Analysis
Another critical step was analyzing the accessory renal artery, which was the lowest in this case. Its location served as an important landmark during the procedure. Ensuring that the graft did not obstruct renal artery flow was a priority.
The accessory renal artery’s position informed our strategy, ensuring that the graft’s contra gate opened above the aneurysm, preserving blood flow to the kidneys.
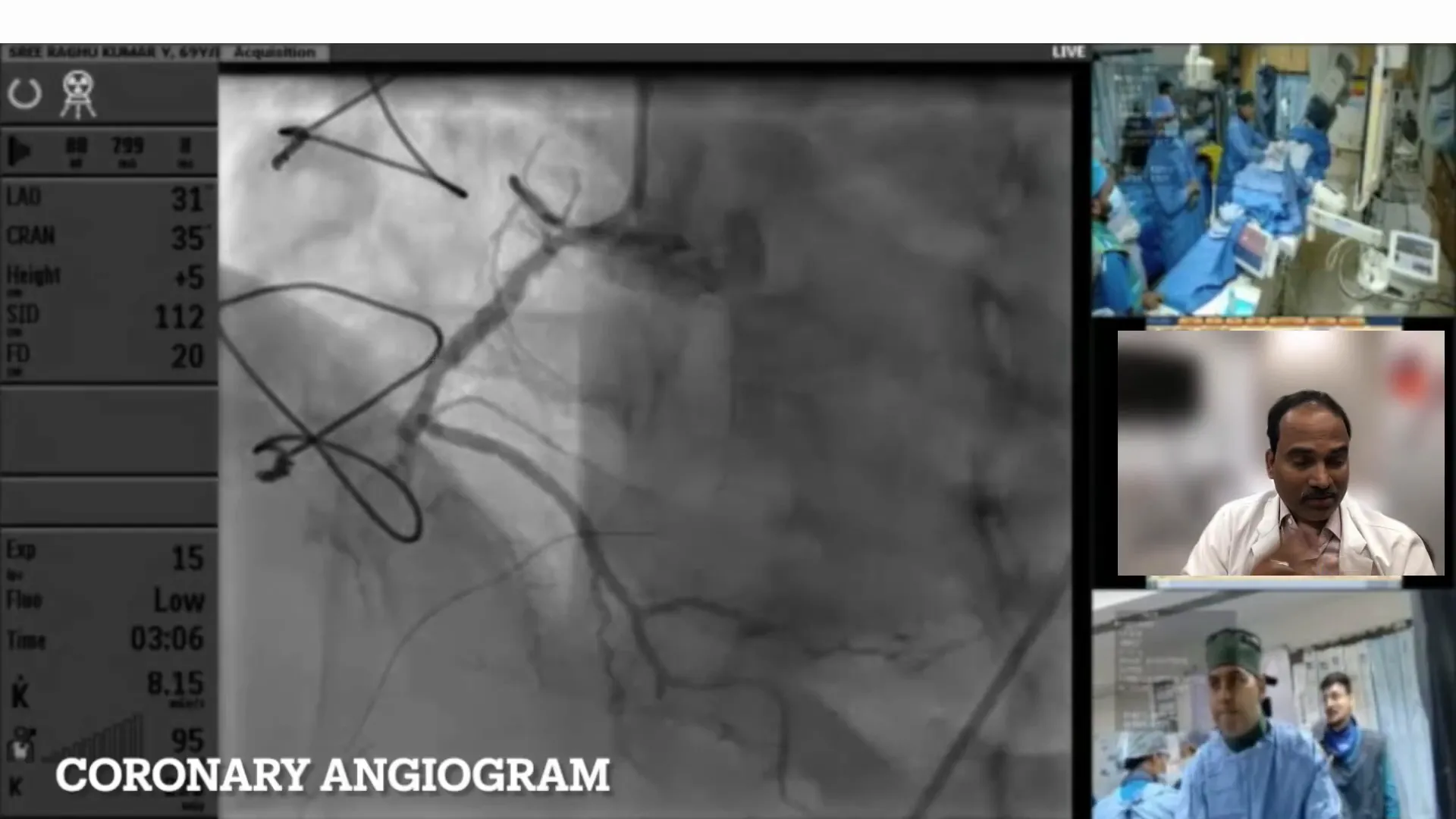
Coronary Angiogram Insights
Prior to the procedure, a coronary angiogram was performed to assess the patient’s coronary status, given his history of coronary artery disease. The right coronary artery was found to be totally occluded, with the distal vessel being small and receiving minimal retrograde filling.
This information was pivotal in confirming that the right coronary territory was nonviable, allowing us to focus on the aneurysm repair without diverting attention to coronary interventions.
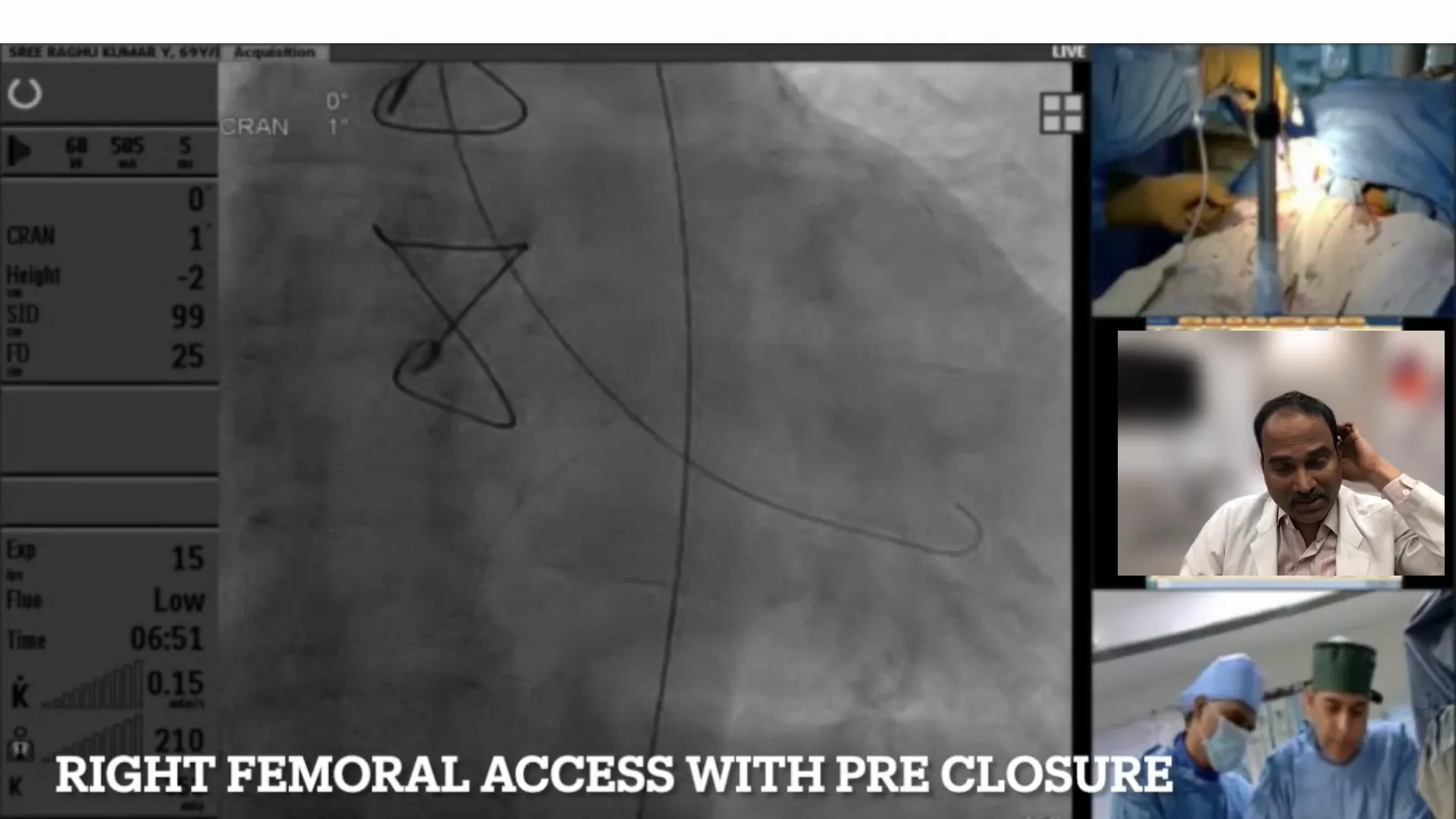
Pre-closure Techniques Employed
Pre-closure of the femoral artery was executed with precision using ProGlide devices. On the right side, two devices were deployed to ensure closure, while the left side required only one due to the smaller French size.
This pre-closure strategy was essential in minimizing post-procedure complications, ensuring hemostasis and reducing the risk of stenosis.
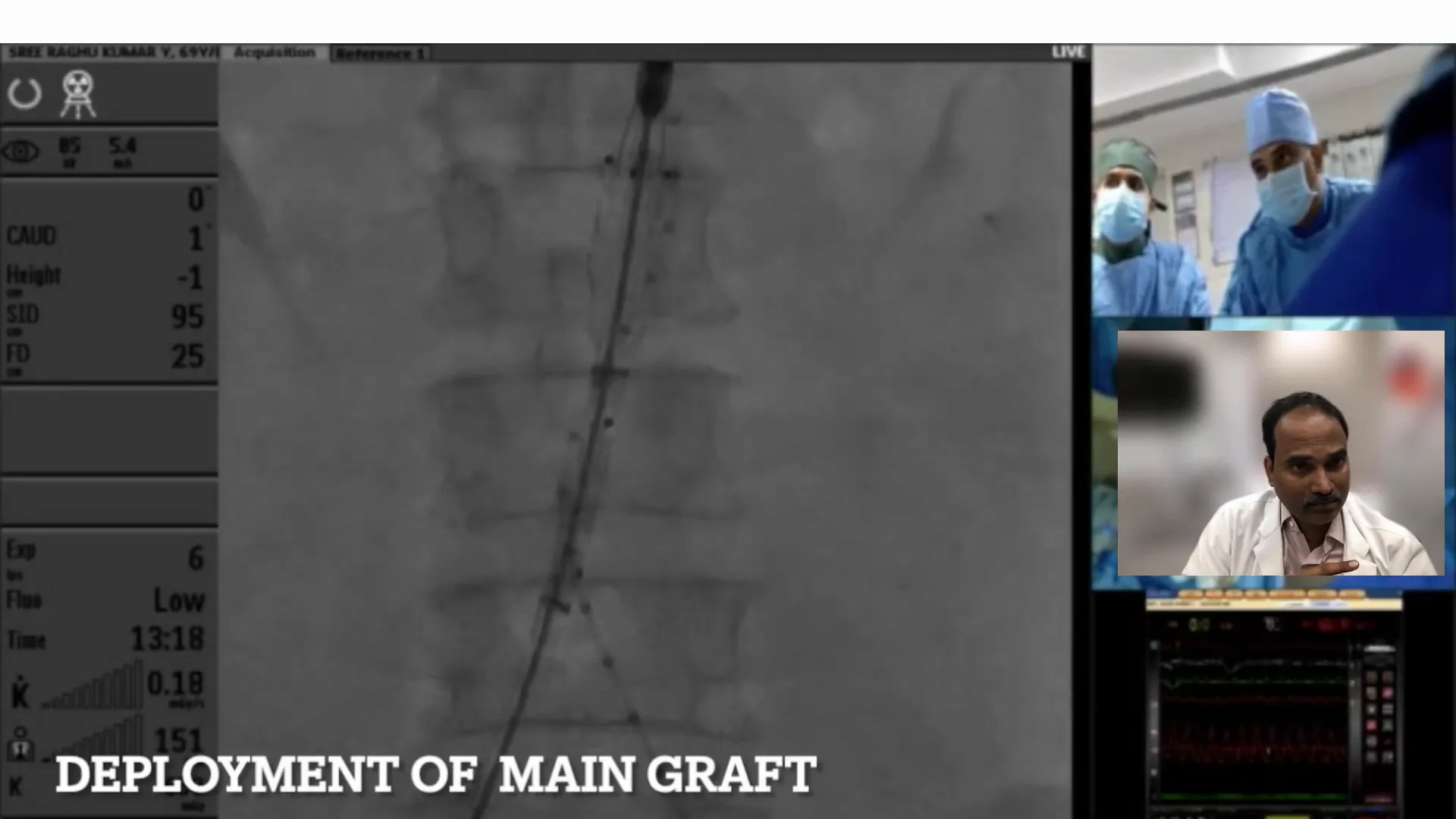
Deployment of the Graft
The deployment of the Endurant graft involved careful navigation and positioning. The left iliac extension was deployed first, followed by the main graft. Ensuring that the contra gate markers were within the aneurysm was crucial for the extension’s success.
Post-deployment, we performed ballooning at both iliac entrances to ensure proper expansion and seating of the graft, crucial for preventing endoleak and ensuring long-term stability.
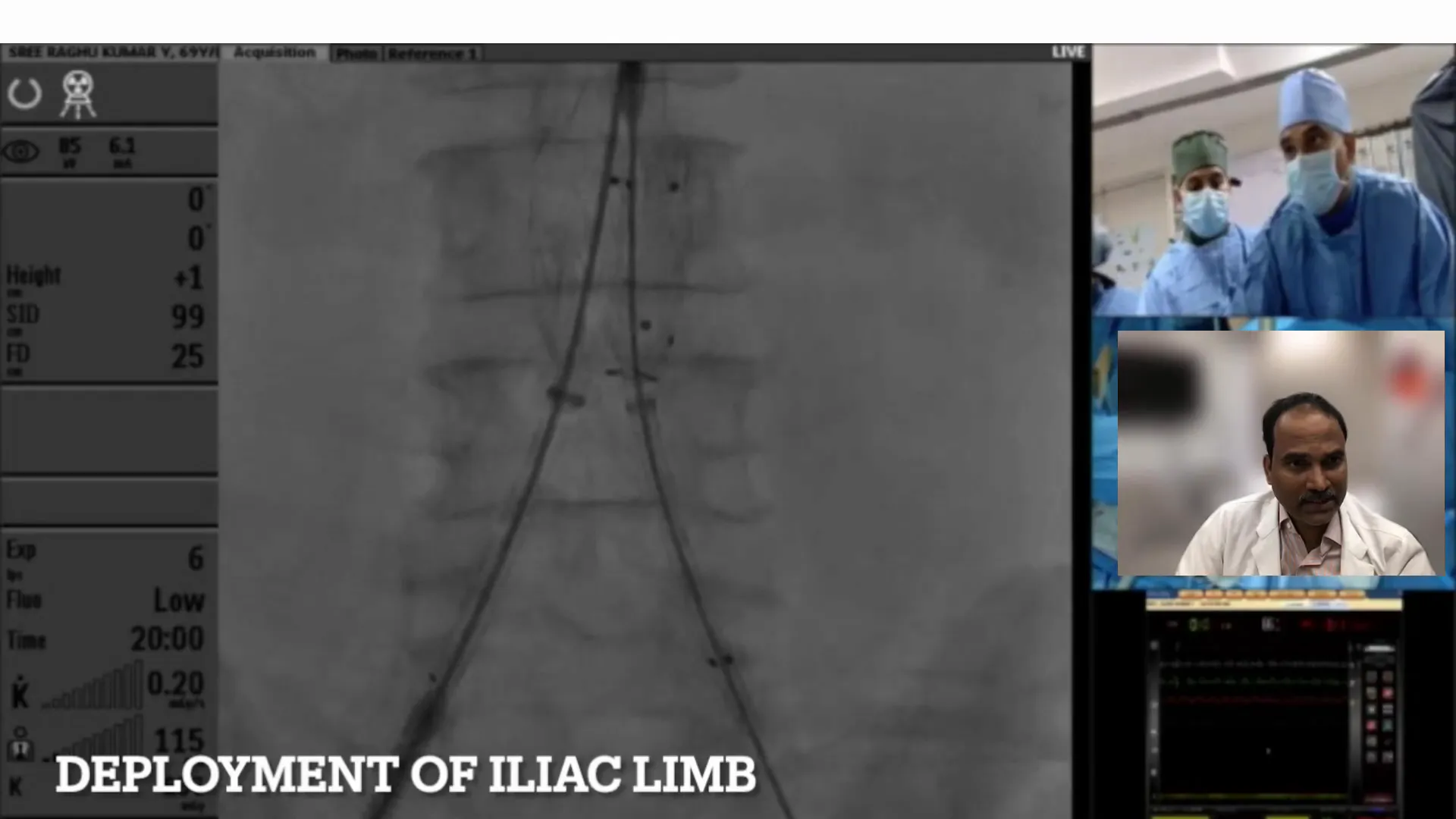
Finalizing the Iliac Extension
After ensuring the graft was accurately positioned within the aneurysm, we proceeded to finalize the iliac extension. This step was crucial to guarantee the stability and function of the entire graft system.
The left iliac extension required careful deployment to align perfectly with the main graft. We used a 90 mm, 16 to 10 tapering device, chosen based on meticulous pre-procedural measurements.
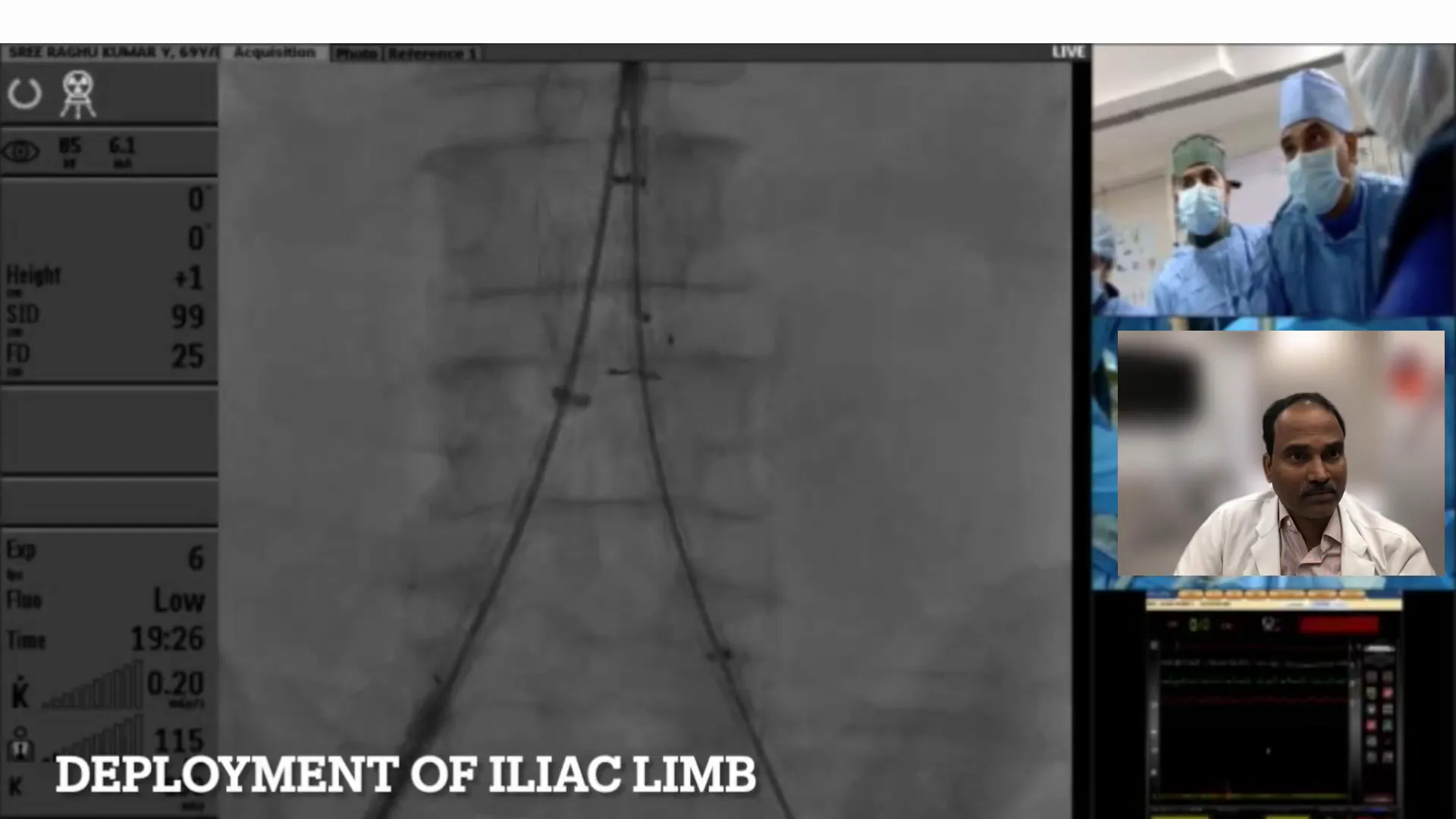
Precision in Deployment
Achieving precise overlap of the markers was essential for the stability of the graft. Once the left extension was secure, we proceeded with the deployment of the right main graft.
This step-by-step approach ensured that each component of the graft was correctly seated, minimizing the risk of endoleaks.
Post-Deployment Assessment
With the graft fully deployed, we conducted a thorough post-deployment assessment. This involved performing an angiogram to check for any type I endoleaks, which could compromise the graft’s effectiveness.
The angiogram revealed a narrowing at the right iliac position, precisely at the bifurcation site. This necessitated immediate intervention to ensure proper blood flow.
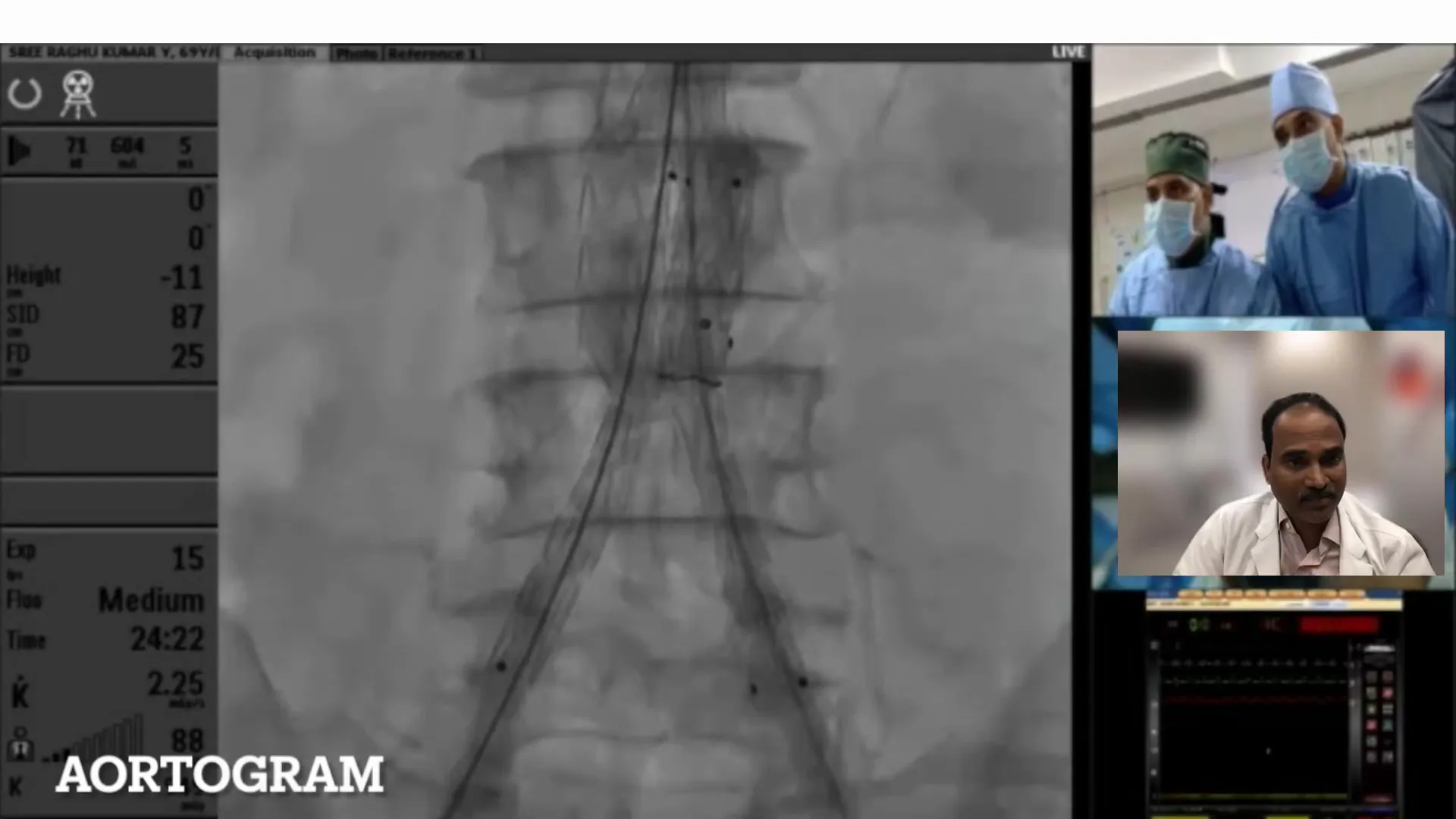
Addressing the Narrowing
To address the detected narrowing, we employed balloon dilation. Two 10 mm peripheral balloons were deployed simultaneously at both iliac entrances, ensuring the graft expanded fully and effectively.
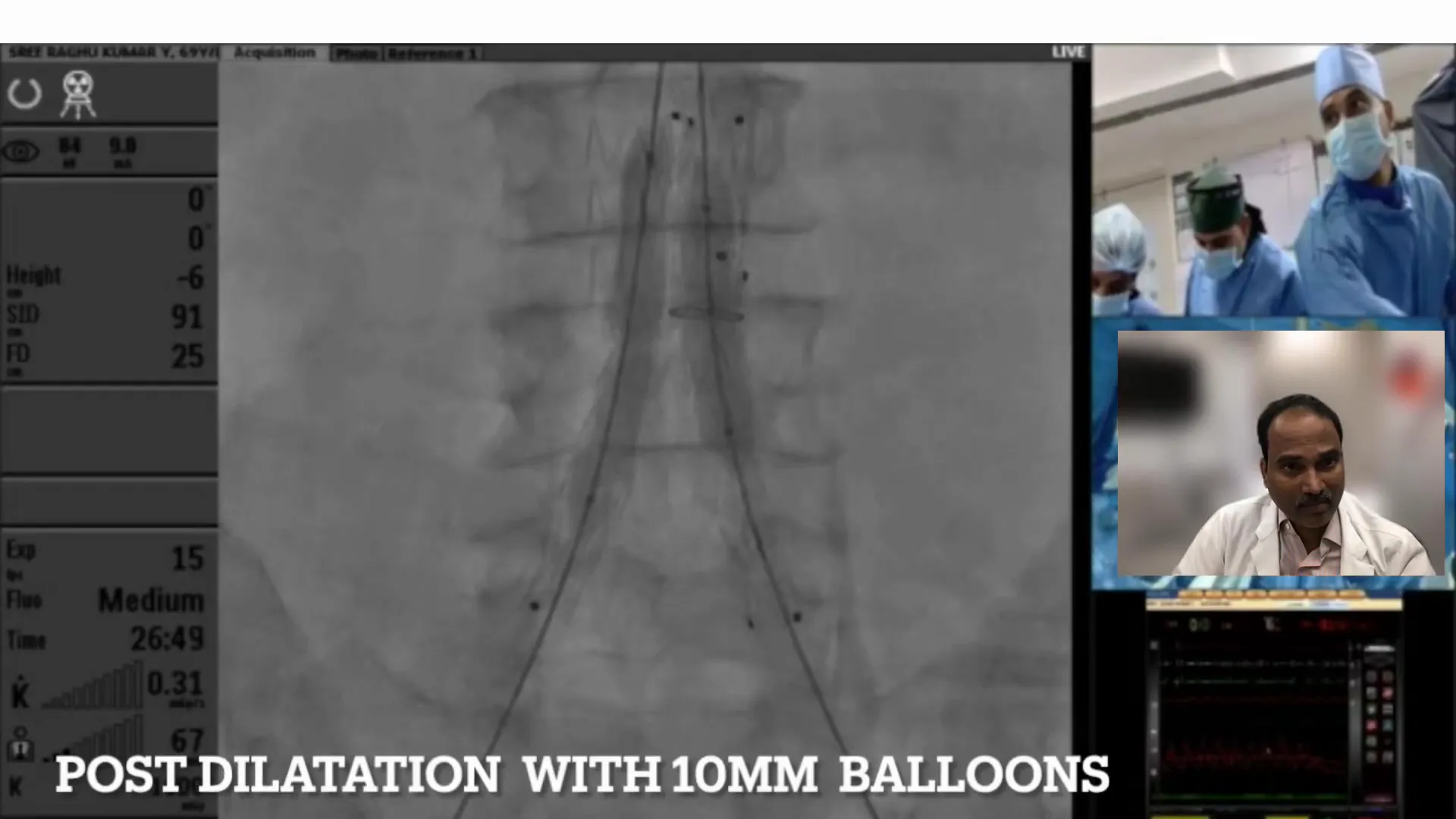
Balloon Dilation Techniques
Balloon dilation was a critical step to ensure the graft’s integration and functionality. By carefully controlling the dilation process, we minimized the risk of rupture and ensured the graft’s secure placement.
We monitored for potential complications such as dissections, but the procedure proceeded smoothly, confirming the success of our intervention.
Ensuring Optimal Results
Post-dilation, we conducted another angiogram to confirm the absence of endoleaks and assess the graft’s integrity. The results were promising, with no signs of complications.

Conclusion and Results
The procedure concluded with excellent results. The carefully planned and executed steps ensured that the graft was securely positioned, and blood flow was restored without complications.
Our approach highlighted the importance of precision and adaptability in managing complex cases involving small aortas and aneurysms.
Key Takeaways
- Thorough pre-procedural planning is crucial in managing small aortic aneurysms.
- Accurate deployment and post-deployment assessments are vital for successful outcomes.
- Balloon dilation techniques can effectively address graft narrowing and ensure optimal results.
FAQs
What challenges arise with small aorta aneurysms?
Small aorta aneurysms present unique challenges due to limited space for graft deployment and increased risk of complications.
How do you ensure accurate graft placement?
Precise measurements and imaging guide graft placement, ensuring alignment and reducing the risk of endoleaks.
What role does balloon dilation play in this procedure?
Balloon dilation helps in expanding the graft to fit the vessel precisely, preventing narrowing and ensuring effective blood flow.
What are the risks associated with this procedure?
Potential risks include endoleaks, graft migration, and vessel rupture, but careful planning minimizes these risks.
How do post-procedural assessments contribute to success?
They provide real-time feedback on graft placement and function, allowing for immediate corrections if necessary.


No Comments