24 Dec Decoding Complex PCI: Rota Through Guide Extension Explained
In this comprehensive blog, we delve into the intricacies of performing Rota through guide extension in complex percutaneous coronary interventions (PCI). Dr. Sharath Annam shares valuable insights through case studies, highlighting techniques, challenges, and solutions in treating tandem lesions in the right coronary artery.
Table of Contents
- Introduction to Rota Through Guide Extension
- Case Study Overview: Patient Profile
- Initial PCI Attempt and Challenges
- Anatomy of the Right Coronary Artery
- Utilizing Guide Extension for Support
- Sequential Ablation Process Explained
- Grenado Plasty Technique and Observations
- The Role of Guide Extension in Rotablation
- Managing the Guide Extension During Procedures
- Final Results of the First Case
- Challenges in Anomalous Right Coronary Artery Cases
- Optimizing Guide Extension Usage
- Best Practices for Rotablation and Guide Extensions
- Conclusion and Key Takeaways
- FAQ: Common Questions About Rota Through Guide Extension
Introduction to Rota Through Guide Extension
The Rota Through Guide Extension technique is a pivotal advancement in the field of interventional cardiology, particularly for complex percutaneous coronary interventions (PCI). This methodology enhances support and navigational capability during the treatment of challenging lesions, especially in anatomically complex cases. By utilizing a guide extension, operators can achieve better control and minimize complications associated with difficult coronary anatomy.
Understanding the Mechanism
Guide extensions are designed to provide additional support to the guide catheter, facilitating the advancement of devices like balloons and rotablation systems across challenging lesions. This is particularly crucial in cases where the anatomy presents significant bends or tortuosity, which can hinder traditional approaches.
Case Study Overview: Patient Profile
In this case study, we analyze a 68-year-old male patient with a history of coronary artery bypass grafting (CABG) who presented with acute coronary syndrome (ACS). His medical history revealed diabetes and hypertension, with a syntax score of 20 indicating significant coronary artery disease.
The patient had undergone CABG in 2019, with a left internal mammary artery (LIMA) to left anterior descending (LAD) artery graft, which remained patent. However, he now faced challenges due to tandem lesions within the right coronary artery (RCA), complicating his treatment options.
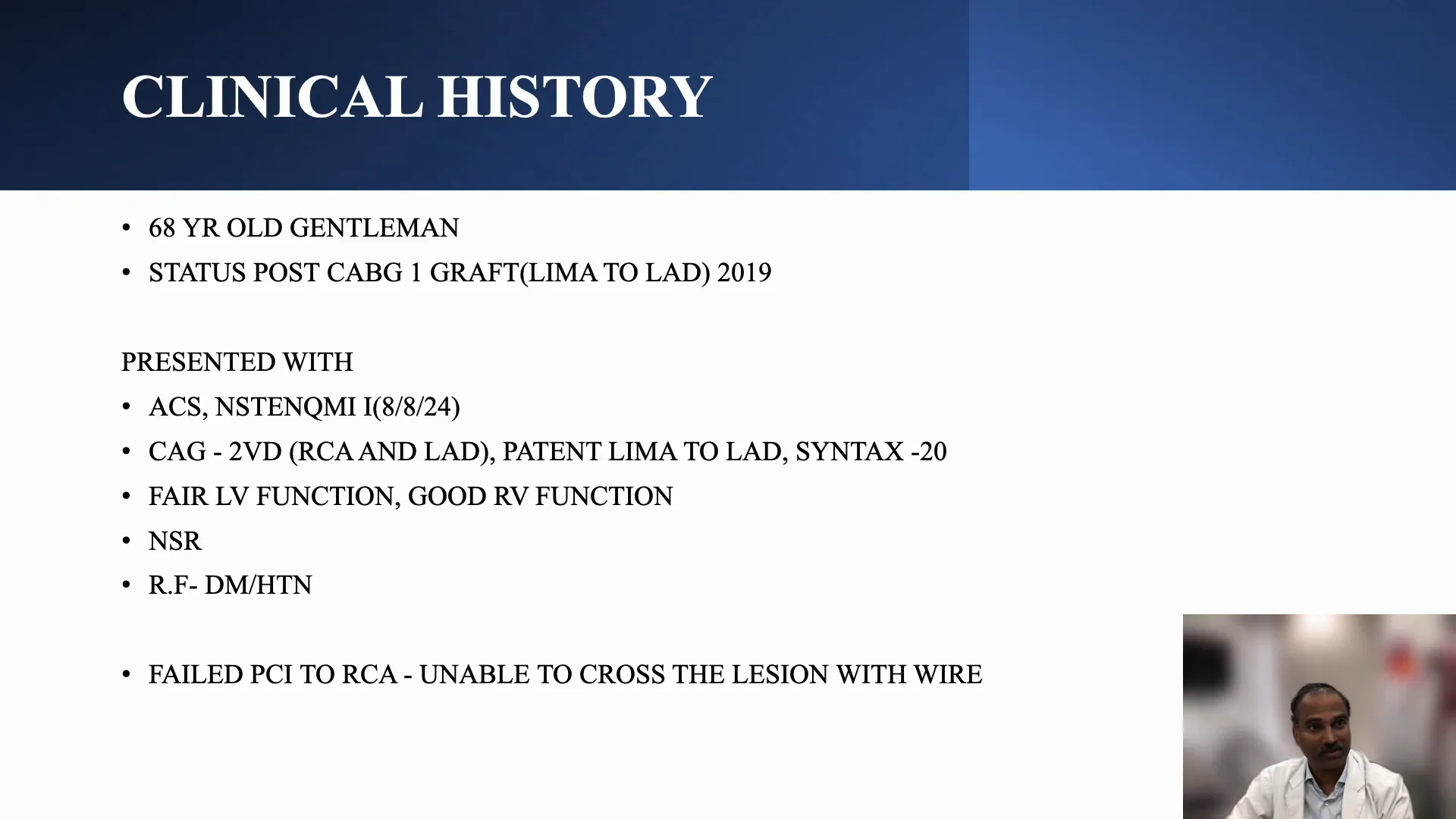
Initial PCI Attempt and Challenges
The first PCI attempt was conducted outside the facility but resulted in failure due to an inability to cross the lesion. The operators encountered significant resistance, primarily attributed to a calcium nodule in the proximal RCA, which obstructed access to the distal lesions.
During this attempt, the guide catheter’s support was inadequate, leading to difficulties in advancing the microcatheter beyond the obstruction. This experience underscores the importance of selecting the appropriate tools and techniques for complex cases.
Anatomy of the Right Coronary Artery
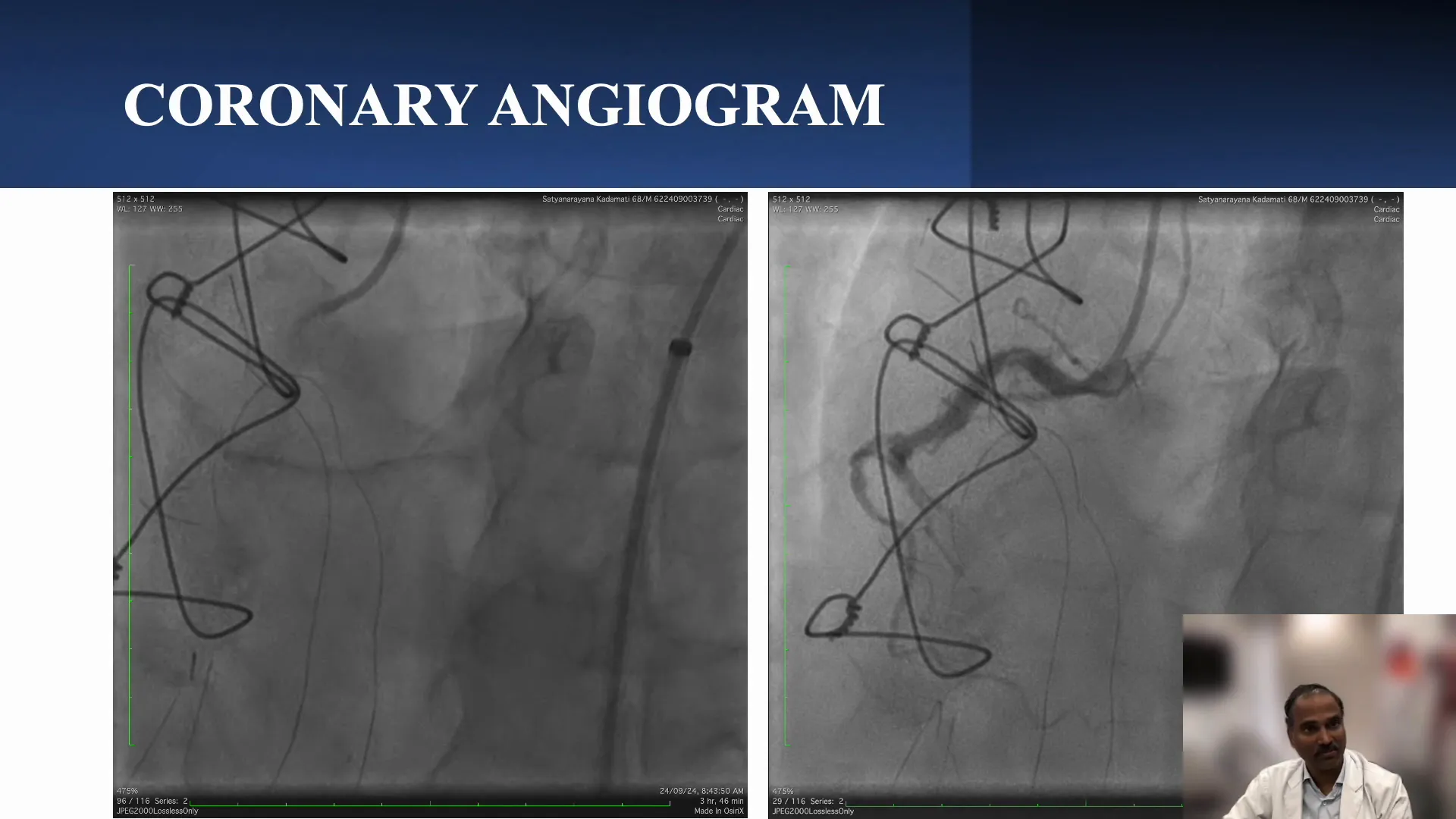
The RCA anatomy can pose unique challenges, particularly in cases with total occlusions and significant calcium deposits. In this patient, a detailed anatomical assessment revealed a loopy RCA with a total occlusion yet some preserved antegrade flow.
Visualizing the anatomy accurately is critical for planning interventions. The presence of multiple bends and a calcium nodule necessitates a careful approach to avoid complications such as perforation during device advancement.
Utilizing Guide Extension for Support
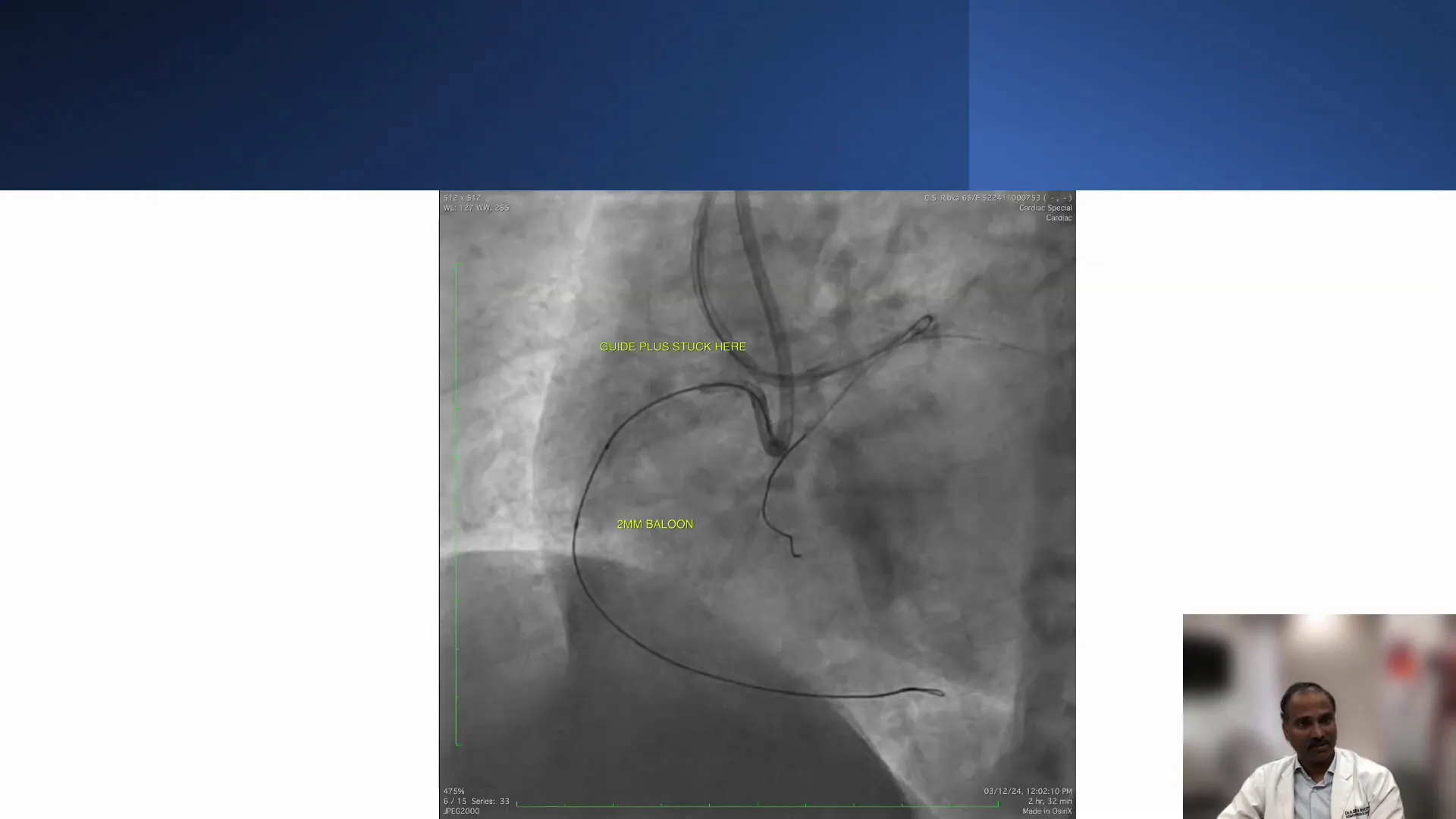
In the subsequent procedure, a guide extension catheter was employed to enhance support and facilitate the crossing of the lesion. This technique allowed for improved engagement with the lesion, providing the necessary backup to advance devices successfully.
The guide extension’s role was crucial, particularly as the initial attempts with conventional catheters had failed. By providing a stable platform, the guide extension enabled the advancement of the fine cross catheter through the proximal lesion.
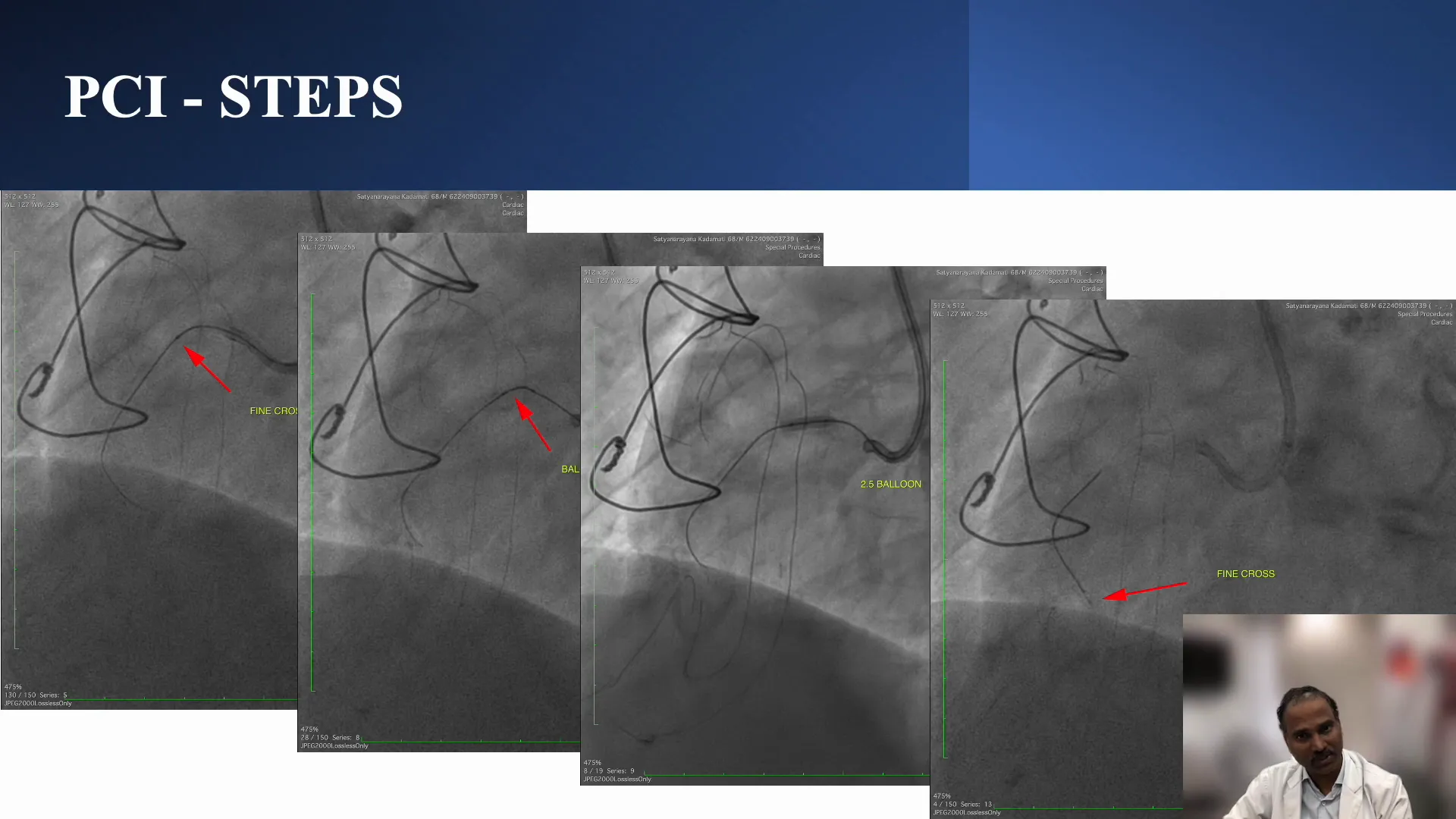
Overcoming Resistance
Despite the advantages of the guide extension, operators still faced resistance at the proximal lesion. This led to a decision to perform sequential ablation, starting with the proximal lesion to create space for further interventions.
This sequential approach allowed for effective lesion management, enabling the team to progressively tackle the more distal lesions following adequate ablation of the proximal obstruction.

Sequential Ablation Process Explained
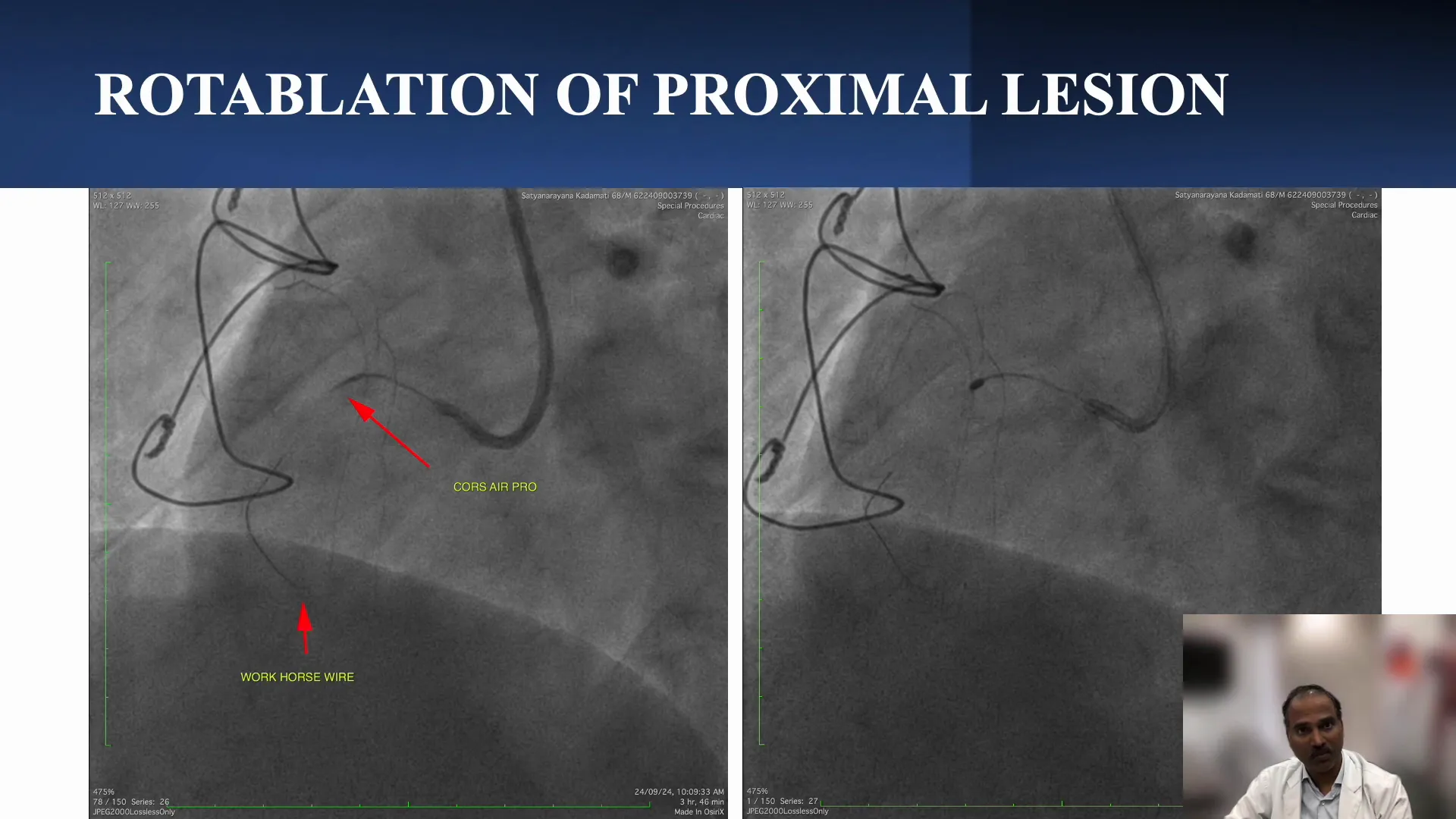
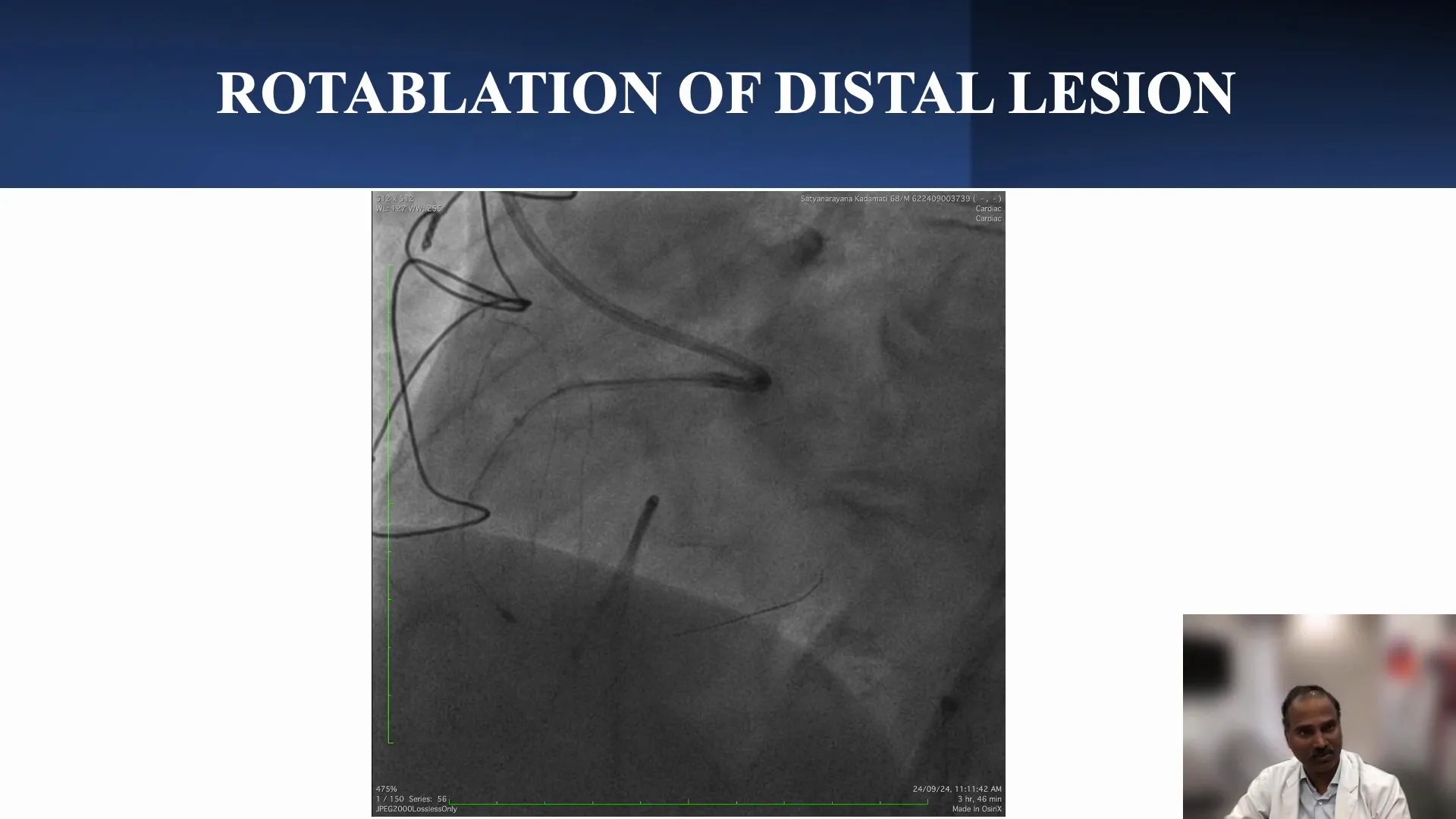
The sequential ablation process involves targeting lesions in a stepwise manner, which can improve outcomes in complex cases. In this instance, the proximal lesion was ablated first using a rotablator with a 1.5 mm burr, effectively addressing the significant calcium nodule.
Post-ablation, operators were able to advance the guide extension further down the artery, facilitating the crossing of the distal lesion. This methodical approach is essential in ensuring a thorough and safe intervention.
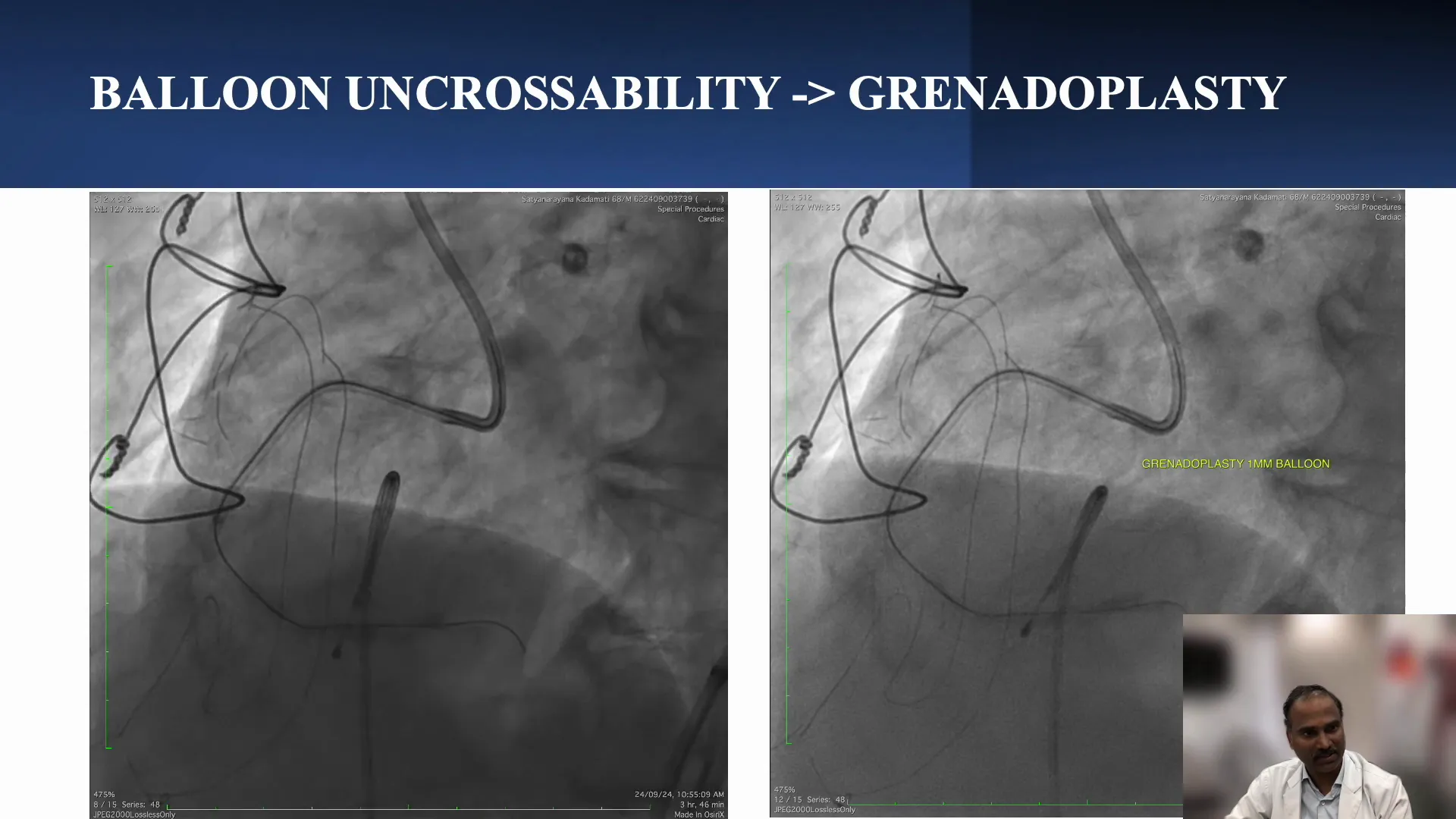
Grenado Plasty Technique and Observations
The Grenado plasty technique was employed as a part of the intervention strategy. A 1 mm balloon was utilized, which ruptured at 20 to 24 atmospheres, demonstrating effective dilation of the lesion and contrast extravasation into the surrounding tissues.
This technique proved beneficial in creating space for the subsequent advancement of the rotablation wire, showcasing the importance of flexibility in interventional strategies based on real-time observations during procedures.
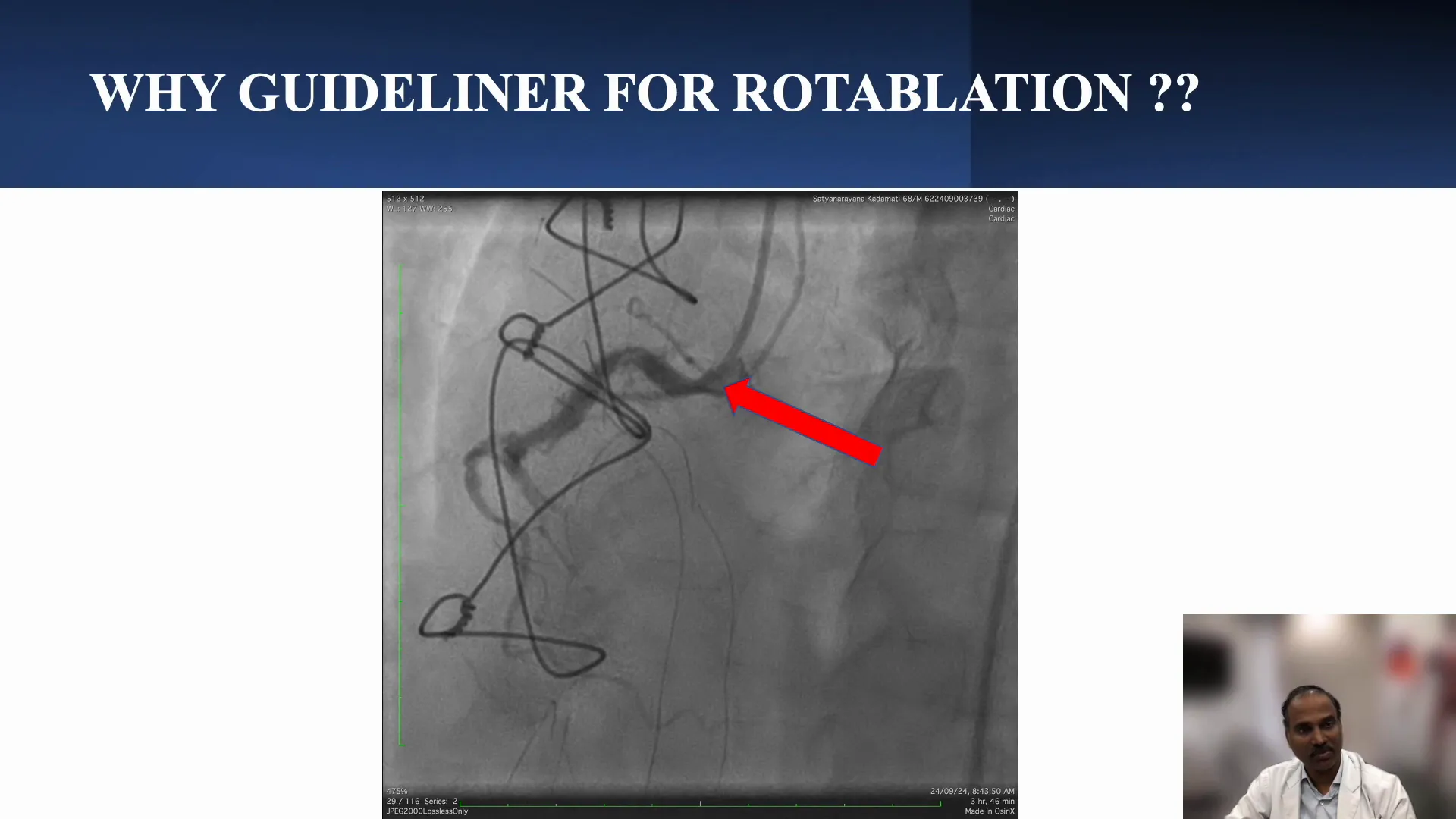
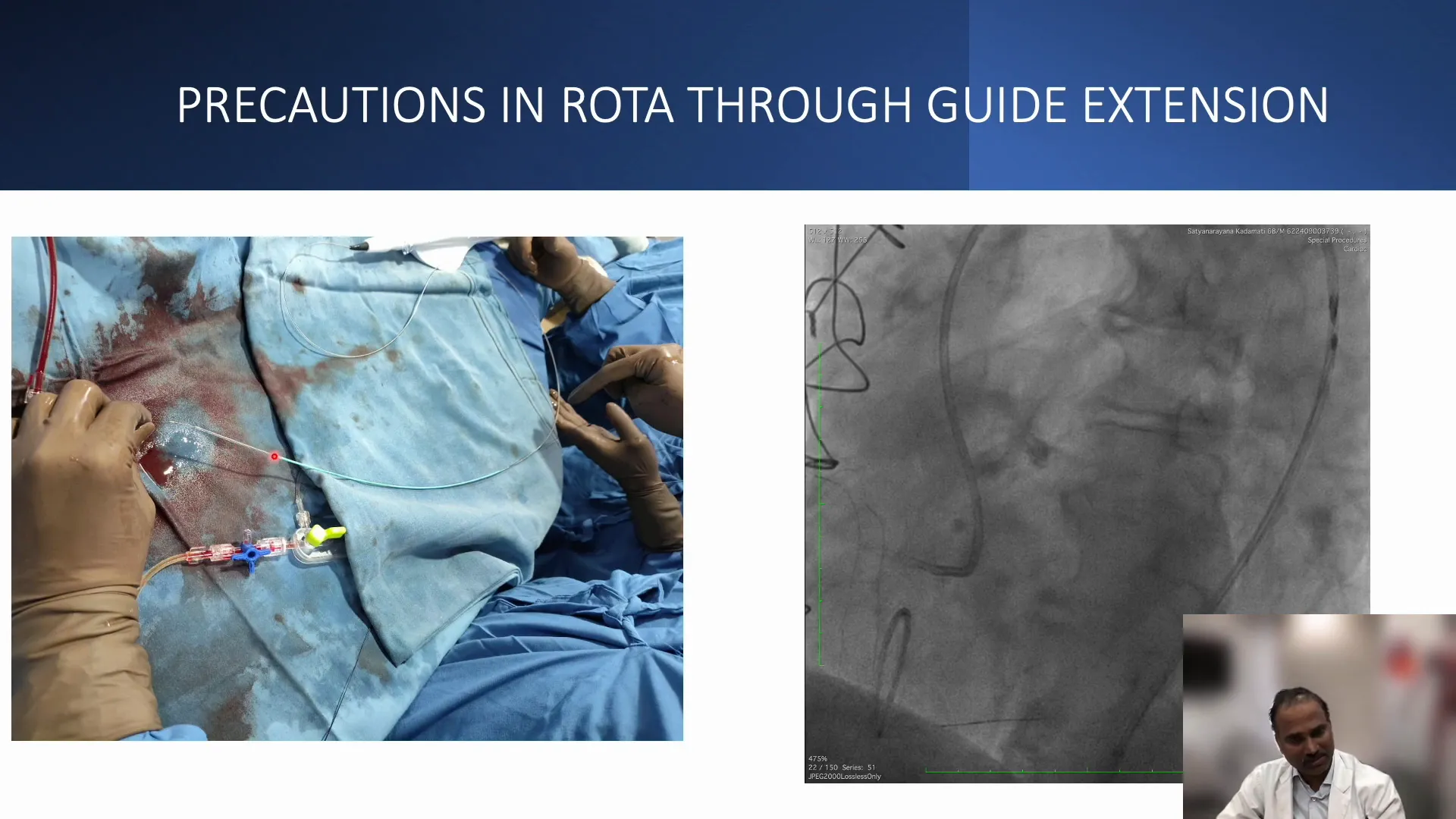
The Role of Guide Extension in Rotablation
The guide extension played a vital role during the rotablation phase. It provided the necessary support to navigate through bends and ensure coaxial alignment with the target lesions, which is essential for successful rotablation.
By minimizing the risk of the “Ferris wheel effect,” where the guide catheter can become non-coaxial, the guide extension enhances the safety and efficacy of the rotablation procedure.
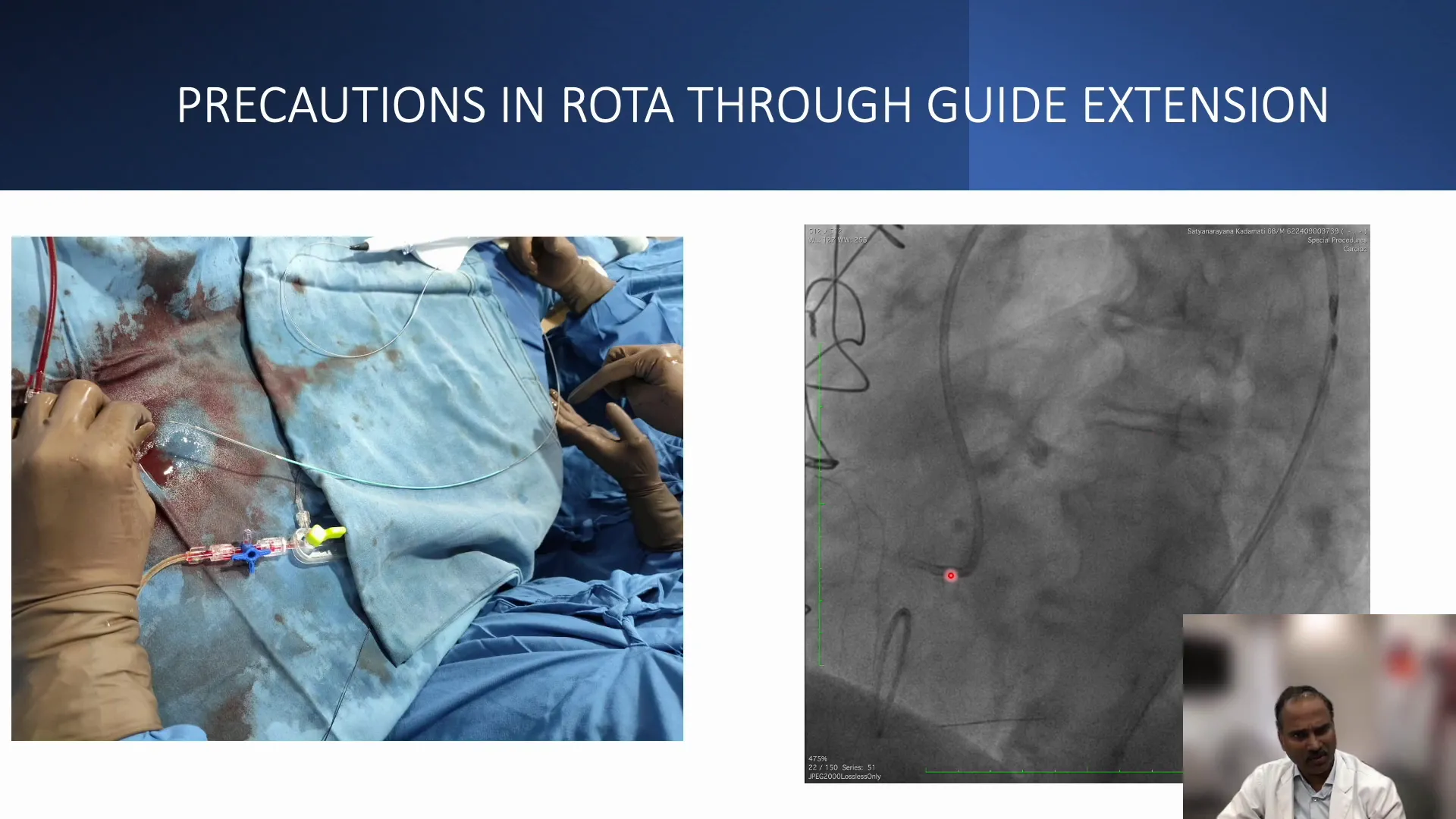
Loading Rota to Guide Extension
Loading the rotablation burr into the guide extension requires careful technique. There are two main methods: one involves loading the burr after the guide extension is already in place, while the other allows for loading onto the rota wire before advancing the guide extension.
Both techniques must be executed with precision to avoid damaging the guide extension or burr. Manual advancement is recommended over automated methods to ensure optimal performance and safety.
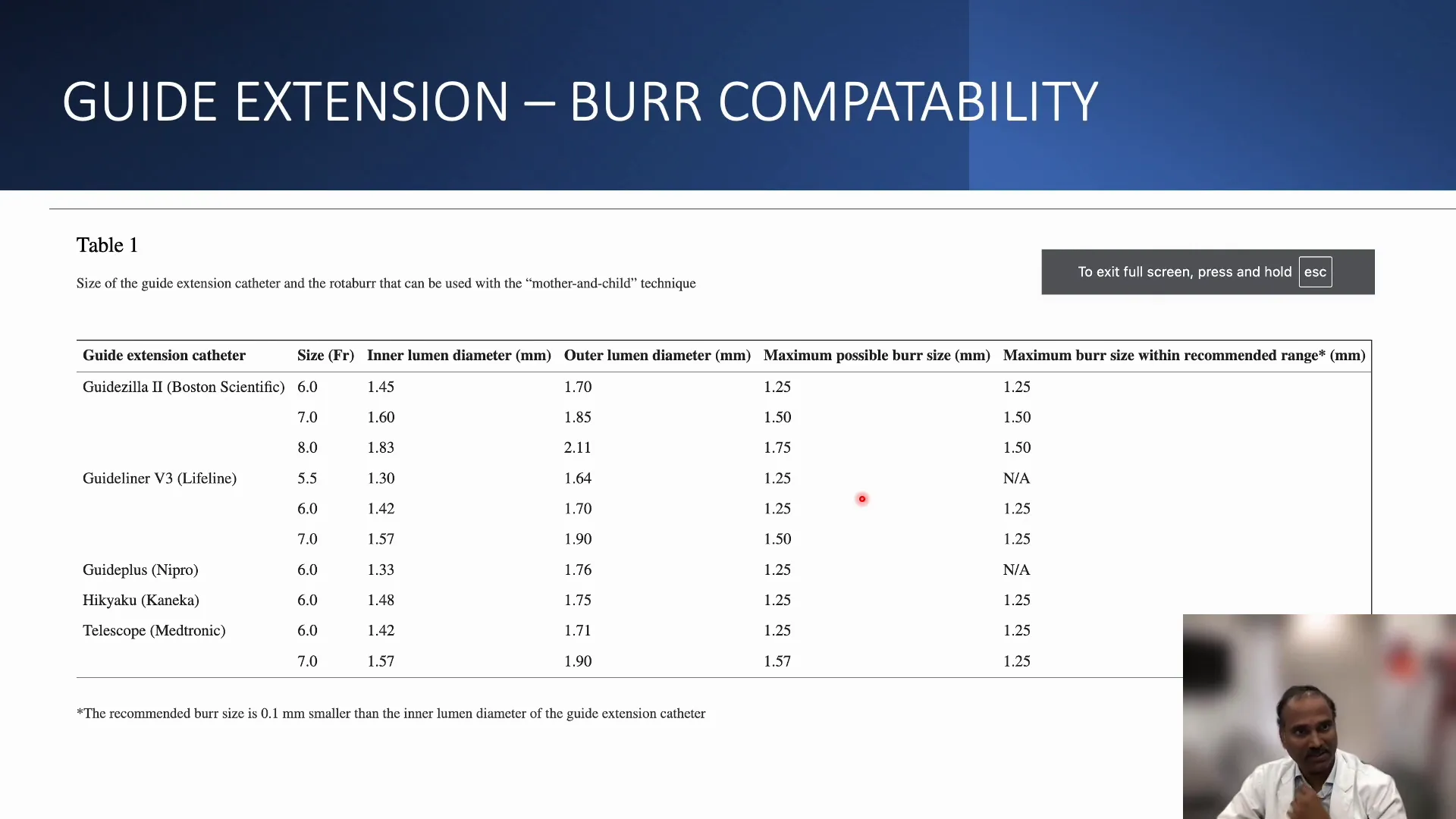
Compatibility of Guide Extension and Burr
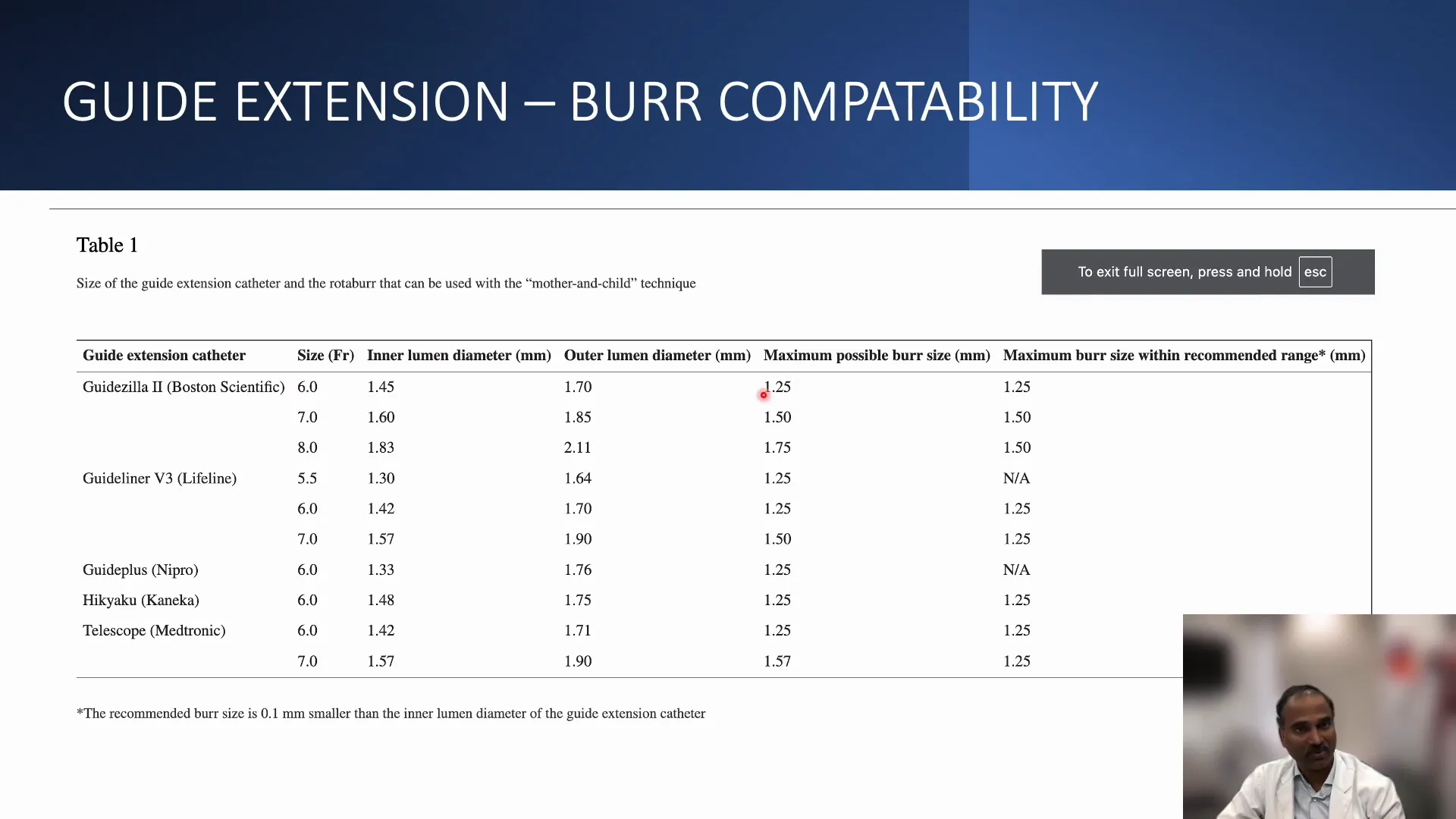
Understanding the compatibility of the guide extension with various burr sizes is crucial. It is recommended to use a burr that is at least 1.1 mm smaller than the inner lumen of the guide extension to maximize efficiency and minimize resistance.
For instance, a 6 French guide extension can accommodate a 1.25 mm burr, while a 7 French can accept a 1.5 mm burr. This compatibility ensures smoother operations during complex interventions.
Managing the Guide Extension During Procedures
Effectively managing the guide extension during procedures is crucial for successful outcomes in complex PCI cases. The guide extension offers enhanced support, but it requires careful handling to ensure optimal performance. Operators need to be mindful of the guide’s positioning and the potential for non-coaxial alignment, especially when navigating through challenging anatomy.
When advancing the guide extension, it is essential to maintain coaxial alignment with the target vessel. If resistance is encountered, pulling back the guide extension slightly can help realign it. This approach minimizes the risk of damaging the guide or the vessel, ensuring a smoother advancement of devices.
Key Considerations
- Coaxial Alignment: Always ensure that the guide extension maintains coaxial alignment with the coronary artery to avoid complications.
- Resistance Management: If resistance occurs, consider pulling back the guide extension rather than forcing advancement.
- Sequential Approach: In cases of multiple lesions, a sequential approach to ablation can create space for further interventions.
Final Results of the First Case
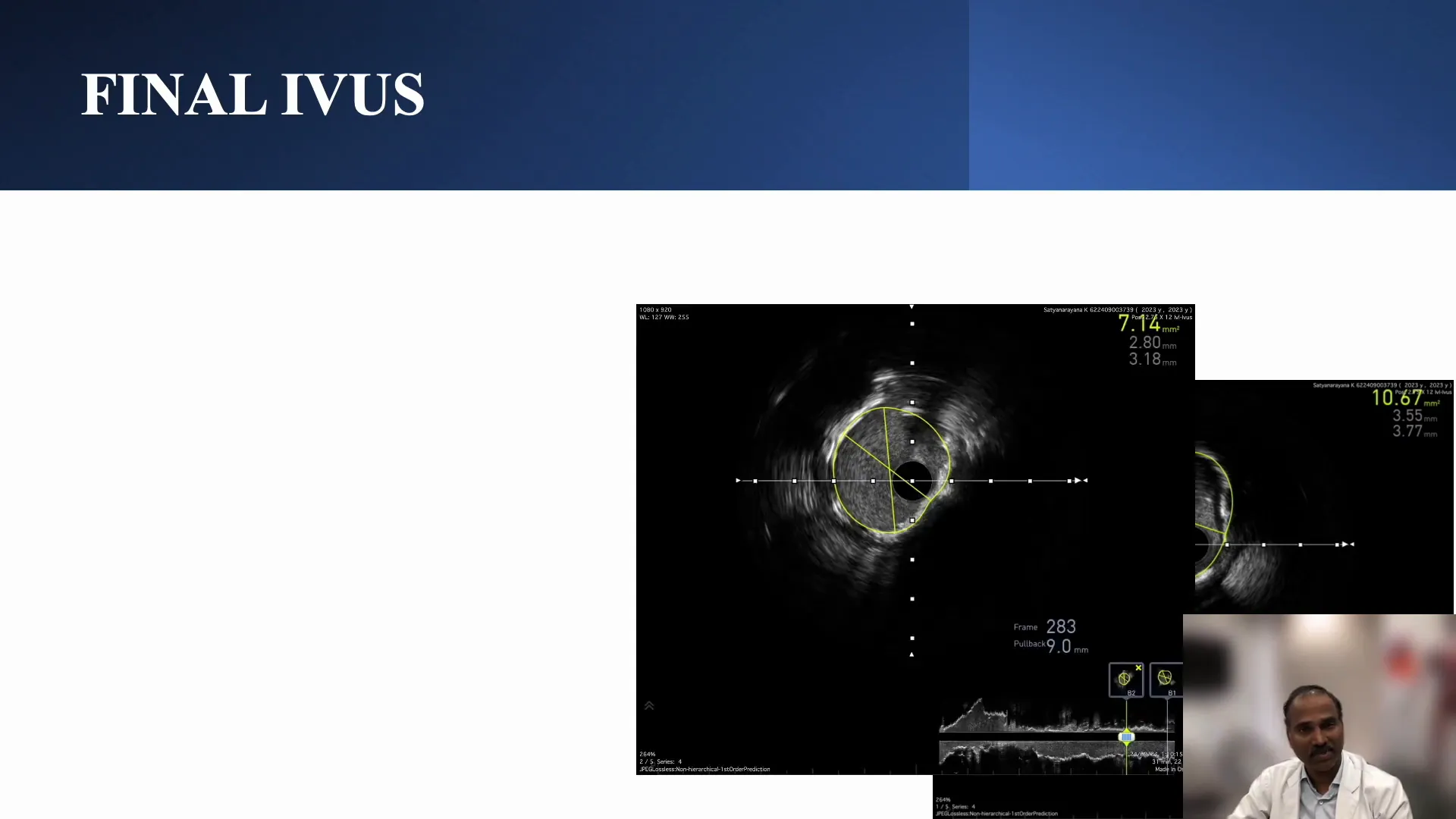
The final results of the procedure demonstrated significant improvements in the patient’s condition. After effective rotablation and careful use of the guide extension, the team achieved a minimum lumen area of 7.2 mm² in the distal lesion, indicating successful treatment of the tandem lesions within the RCA.
Post-procedure imaging revealed good flow through the previously obstructed segments, with only minor residual slow flow. This outcome highlights the effectiveness of using the guide extension in conjunction with rotablation, especially in complex cases involving significant calcification.
Challenges in Anomalous Right Coronary Artery Cases
Anomalous right coronary artery cases present unique challenges during PCI procedures. These anomalies can lead to difficulties in achieving coaxial alignment and navigating through the coronary system. Operators must be prepared to adapt their techniques to accommodate these anatomical variations.
In such cases, the guide extension becomes invaluable. It provides the necessary support and helps mitigate the risk of perforation due to the bends and loops present in the anomalous vessels. Understanding the specific anatomy of the anomalous RCA is critical for planning and executing the intervention successfully.
Strategies for Success
- Thorough Imaging: Utilize advanced imaging techniques to assess the anatomy before the procedure.
- Adapt Techniques: Be prepared to modify standard techniques to accommodate the unique challenges posed by anomalous vessels.
- Utilize Guide Extensions: Leverage guide extensions for enhanced support and stability during interventions.
Optimizing Guide Extension Usage
To optimize the use of guide extensions, operators should focus on compatibility with various devices and the specific requirements of the case at hand. Selecting the appropriate guide extension size is crucial to ensure efficient device delivery and minimize resistance.
Additionally, understanding the loading techniques for rotablation devices is essential. Manual advancement should be prioritized to prevent damage to the guide extension and the devices being used. Operators must be vigilant about the inner diameter of the guide extension to ensure compatibility with the burr size.
Best Practices
- Choose the Right Size: Always select a guide extension that is compatible with the devices being used, considering the inner diameter.
- Manual Advancement: Avoid automated methods for advancing devices through the guide extension; opt for manual techniques to ensure safety.
- Monitor for Resistance: Be aware of any resistance during advancement and adjust techniques accordingly.
Best Practices for Rotablation and Guide Extensions
Incorporating best practices for rotablation and guide extensions can significantly enhance procedural outcomes. Operators should focus on the following key aspects:
- Preparation: Ensure that all devices, including the guide extension, are ready and compatible before starting the procedure.
- Real-time Monitoring: Continuously assess the guide’s position and alignment during the procedure to avoid complications.
- Effective Communication: Foster a collaborative environment among team members to share insights and make quick decisions as needed.
Conclusion and Key Takeaways
The use of guide extensions in complex PCI cases, particularly those involving rotablation, has proven to be a game-changer. By providing enhanced support and stability, guide extensions facilitate the successful navigation of challenging anatomies, ultimately leading to better patient outcomes.
Key takeaways from this discussion include:
- The importance of maintaining coaxial alignment to prevent complications.
- Utilizing sequential approaches to manage multiple lesions effectively.
- The necessity of adapting techniques for anomalous coronary anatomies.
FAQ: Common Questions About Rota Through Guide Extension
What is the primary benefit of using a guide extension during PCI?
The primary benefit of using a guide extension is to provide enhanced support and stability, allowing for better navigation through complex coronary anatomies, particularly in cases with significant bends or resistance.
How do I ensure compatibility between the guide extension and rotablation devices?
To ensure compatibility, always select a burr that is at least 1.1 mm smaller than the inner lumen of the guide extension. This minimizes resistance and facilitates smoother device advancement.
What should I do if I encounter resistance while advancing the guide extension?
If resistance occurs, consider pulling back the guide extension slightly to realign it rather than forcing it forward. This approach helps prevent damage to both the guide extension and the vessel.
Are there specific techniques for loading rotablation devices into the guide extension?
Yes, there are two main techniques: loading the burr after the guide extension is in place or loading it onto the rota wire before advancing the guide extension. Manual advancement is recommended in both cases to avoid complications.


No Comments