06 Sep Impella Assisted PCI by Dr. Sharath Reddy
In this detailed case study, Dr. Sharath Reddy explores the complexities of a 71-year-old male patient undergoing a Chip CTO PCI with the Impella system. The blog delves into the clinical history, procedural strategies, challenges faced, and the implications of hemodynamic support in interventional cardiology.
Table of Contents
- Introduction to the Case
- LMCA Bifurcation PCI – Mini Crush Technique
- RCA CTO PCI – Dual Injection Strategy
- Post Procedure Hemodynamics Assessment
- Take Home Messages from the Case
- Frequently Asked Questions (FAQ)
Introduction to the Case
This case study focuses on a 71-year-old male patient with a complex cardiac history, including diabetes and recurrent episodes of acute coronary syndrome. His medical history includes a previous chronic total occlusion (CTO) in the right coronary artery (RCA) and stenting of the left anterior descending artery (LAD) and ramus intermedius. The patient presented with decompensated heart failure, leading to multiple hospital admissions within a short span.
Patient Clinical History
The patient is a known diabetic with a history of moderate left ventricular (LV) dysfunction. He has been a drug defaulter, which likely contributed to his deteriorating condition. Upon admission, he exhibited severe mitral regurgitation (MR) and high blood pressure, indicative of significant cardiac strain.
His echocardiogram revealed dynamic MR that worsened with exertion, leading to increased breathing difficulties. The coronary angiogram confirmed the presence of a total occlusion in the RCA and significant disease in the osteo left circumflex artery (LCX).
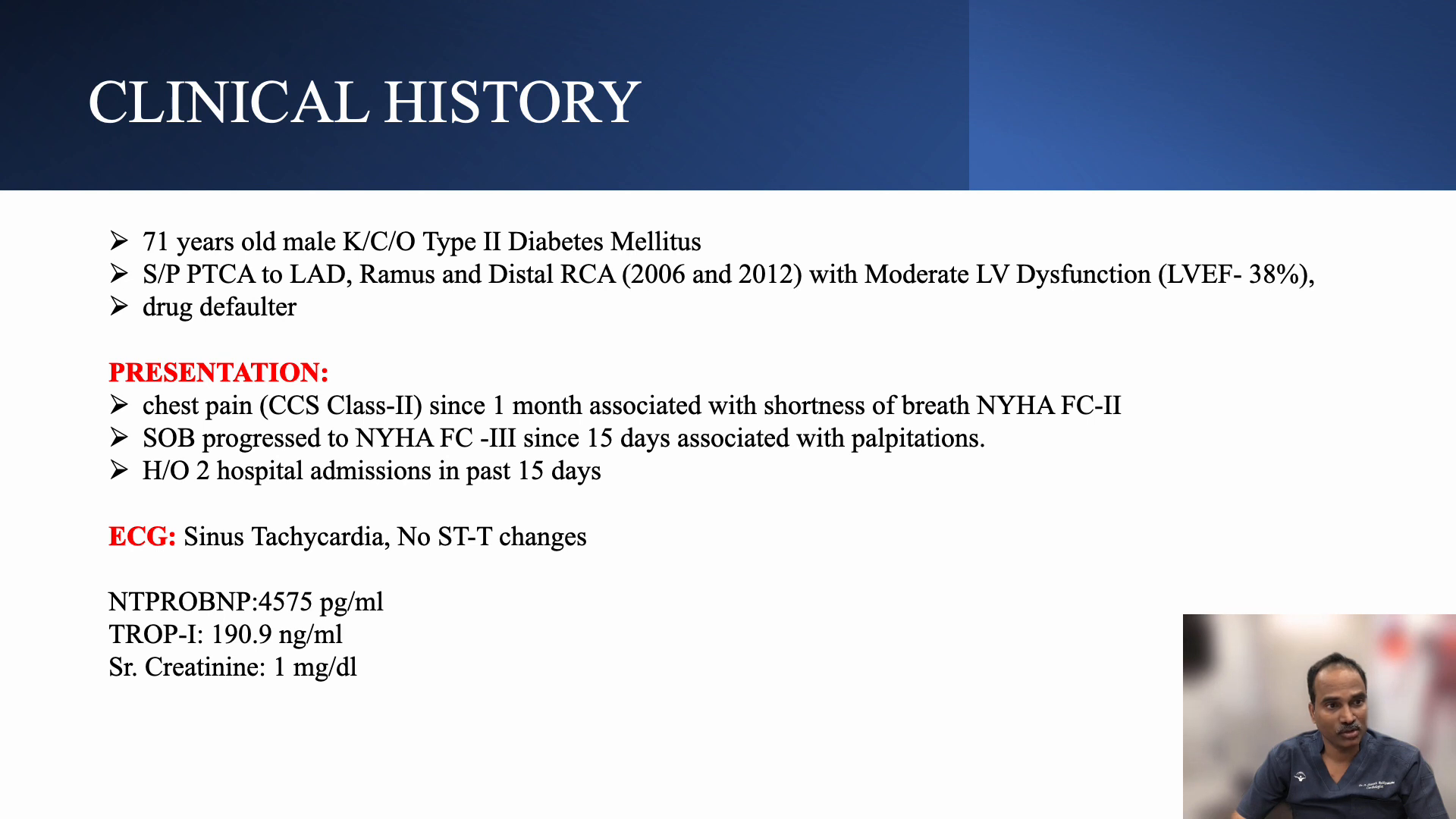
Initial 2D Echo Findings
At the time of admission, the echocardiogram indicated severe MR, compounded by hypertension. Notably, the patient’s blood pressure was recorded at 78/88 mmHg, highlighting the hemodynamic instability. The MR was dynamic; while it reduced with rest and medication, it escalated during exertion, leading to further complications.
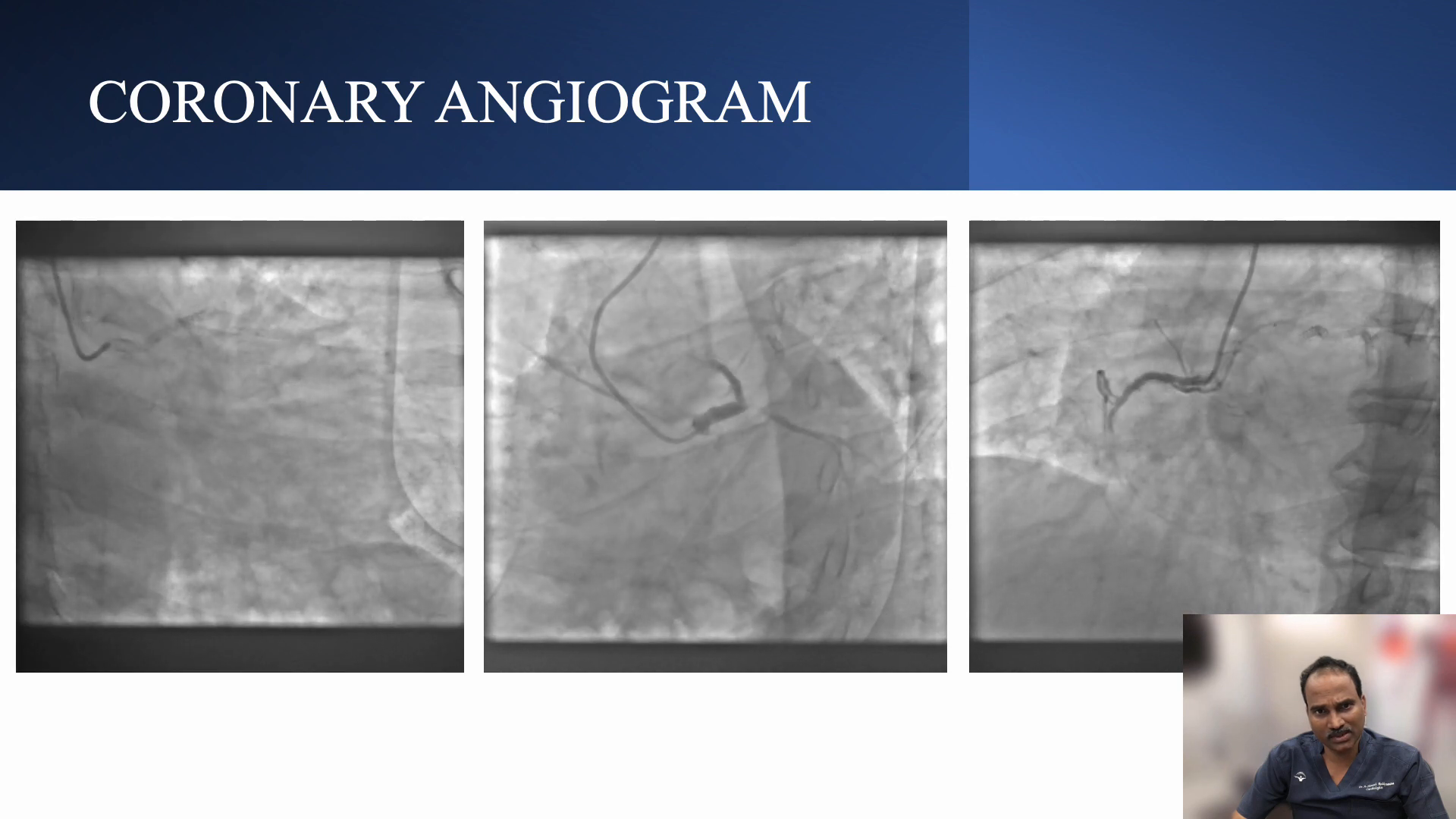
Coronary Angiogram Analysis
The angiogram revealed a patent stent in the LED, a completely occluded ramus, and a total occlusion in the RCA. The osteo LCX was severely stenosed at nearly 99%. These findings indicated a high-risk scenario, necessitating careful planning for percutaneous coronary intervention (PCI).
Assessing Risk Scores
Risk assessment tools indicated a high SYNTAX score and a high EuroSCORE, emphasizing the complexity of the case. The CHIP score of 10 further supported the need for a protected PCI approach due to the patient’s age, comorbidities, and significant hemodynamic instability.
Given the challenging anatomy, including a calcified and lengthy CTO, several strategies were considered, including potential retrograde access and the use of guide extensions.
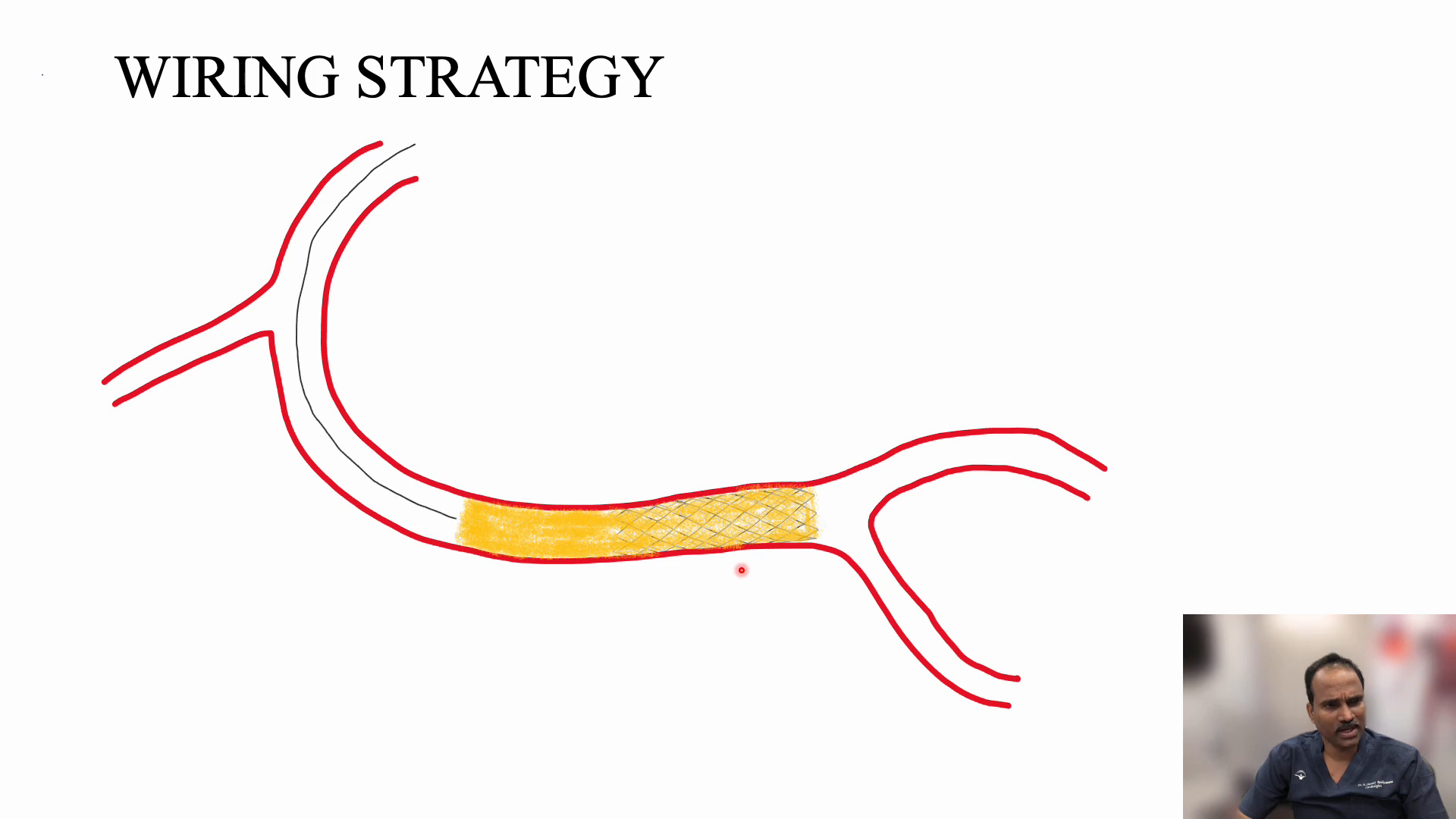
Wiring Strategy Overview
The collateral circulation to the PDA through the septal branches provided a potential route for retrograde access. The presence of a stent in the distal segment of the CTO acted as a marker, simplifying the wiring process. The strategy involved parking a microcatheter proximal to the cap and using a directable wire to navigate through the CTO.
Challenges and Solutions During the Procedure
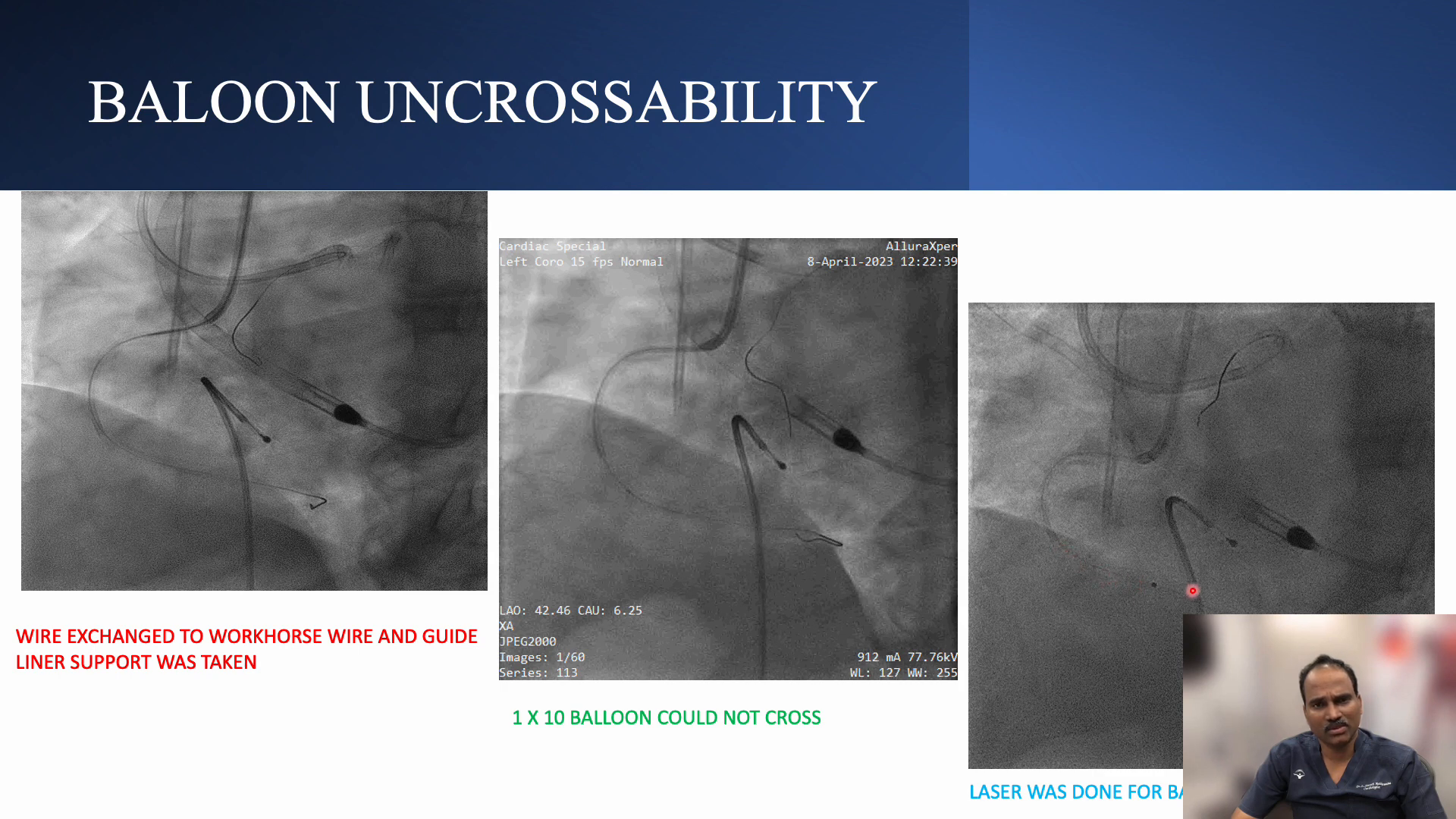
During the procedure, two significant challenges arose: managing hemodynamics under Impella support and navigating the RCA with suboptimal guide catheter support. The Impella device provided critical hemodynamic support, but the use of a guide extension and anchor balloon was necessary to facilitate the PCI.
Despite initial difficulties in crossing the lesion with a balloon, the use of laser atherectomy proved effective in modifying the plaque and enhancing the chances of successful balloon dilation.
PA Catheterization Insights
The procedure was complicated by an episode of severe hypertension, likely due to the prolonged guide extension in a hemodynamically unstable environment. Monitoring revealed loss of contractility, prompting a fluid bolus to stabilize the patient’s condition.
Post-procedure, the hemodynamics improved significantly, with stable pressures and improved LV function noted. The final angiographic results showed successful revascularization with no residual MR, illustrating the efficacy of the intervention.
LMCA Bifurcation PCI – Mini Crush Technique
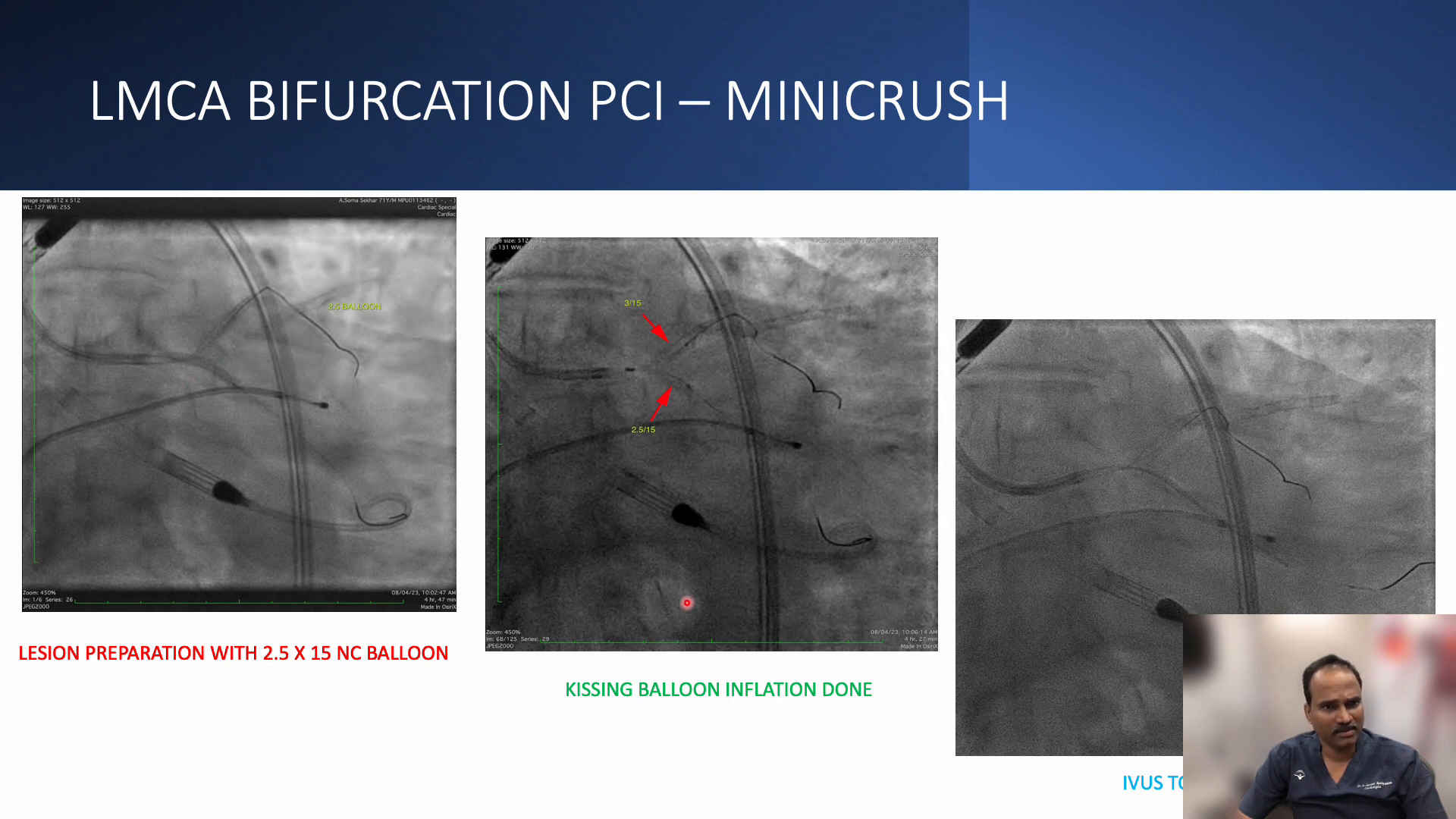
The Mini Crush technique is a well-established method for treating bifurcation lesions, particularly in the left main coronary artery (LMCA). This technique involves stenting both branches of the bifurcation while minimizing the risk of stent thrombosis and restenosis. In this case, the Mini Crush approach was utilized due to the complex anatomy and the presence of severe calcification.
During the procedure, after preparing the lesion, a stent was deployed in the left circumflex artery (LCX) first. Subsequently, a kissing balloon technique was employed to optimize the results, ensuring that both branches were adequately dilated. This dual approach not only improves flow dynamics but also enhances the overall stability of the stents placed.
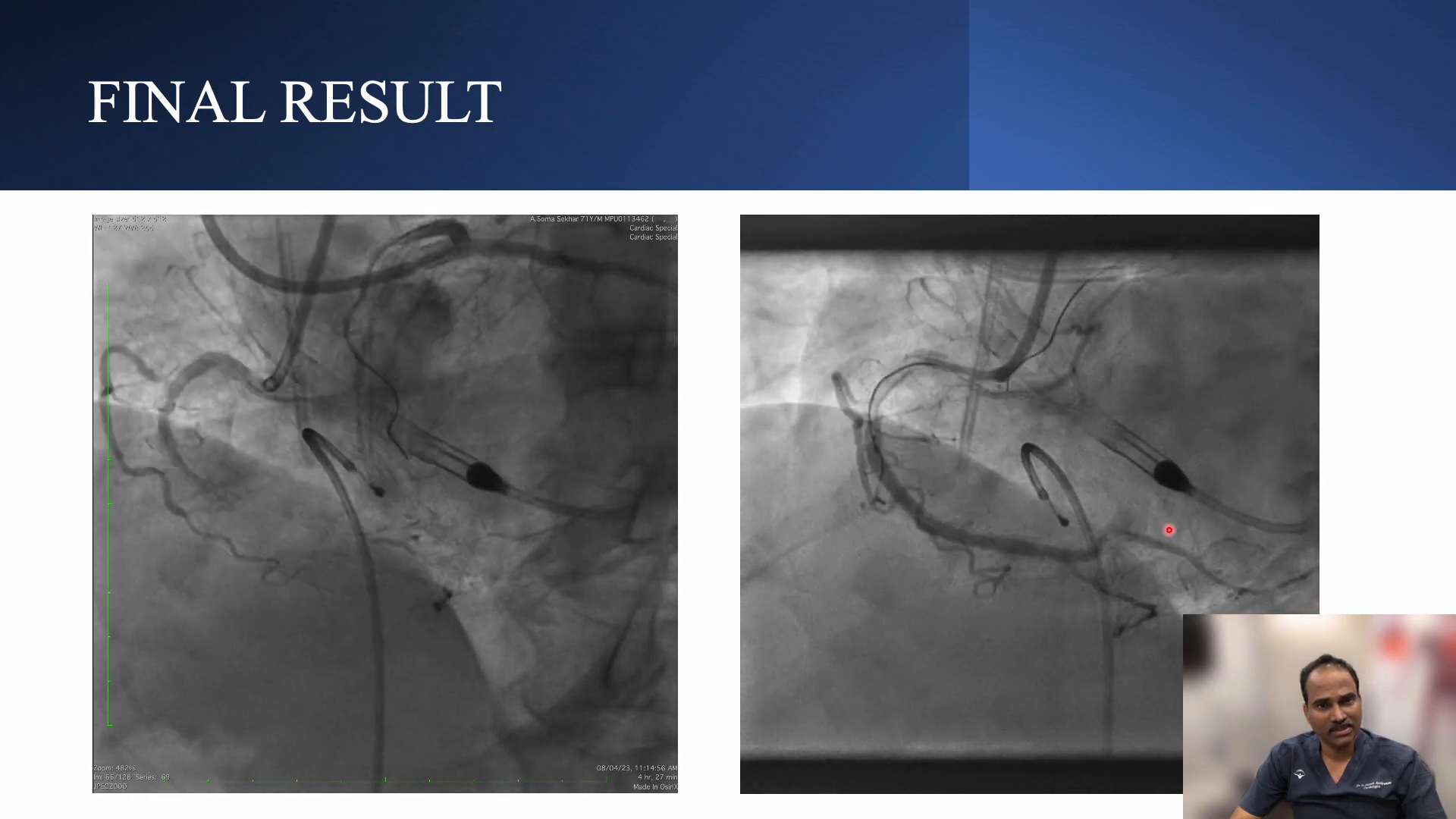
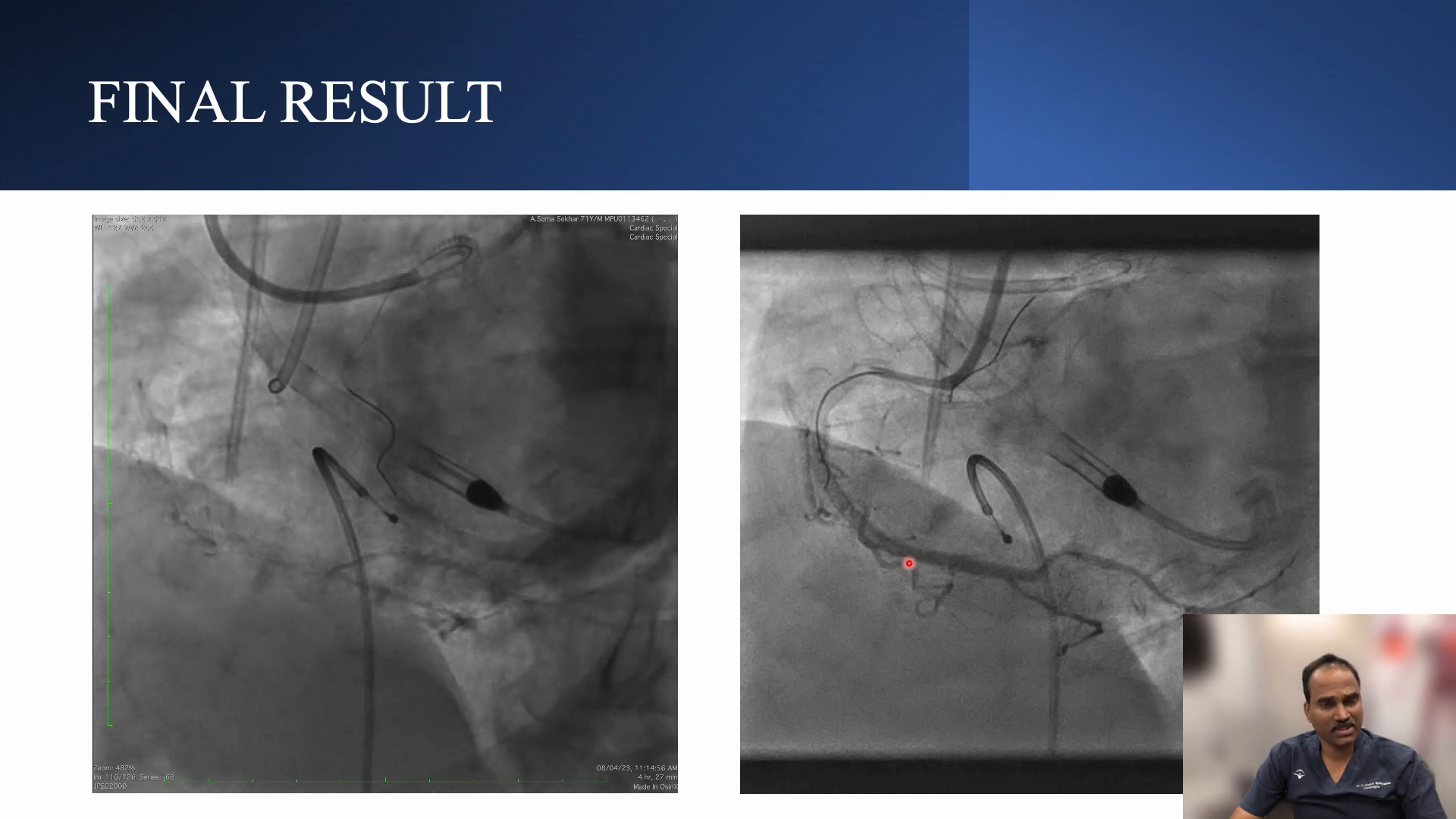
Final Results After Mini Crush, POT, Kissing & Repot
After employing the Mini Crush technique, the final angiographic results were promising. The stents were well-positioned, and there was no evidence of residual stenosis. Post-intervention, pressure measurements indicated improved hemodynamics, confirming the effectiveness of the procedure.
Additionally, a post-dilation with a non-compliant balloon was performed to ensure optimal stent expansion. The use of intravascular ultrasound (IVUS) further confirmed adequate stent apposition and expansion, which is critical for long-term success.
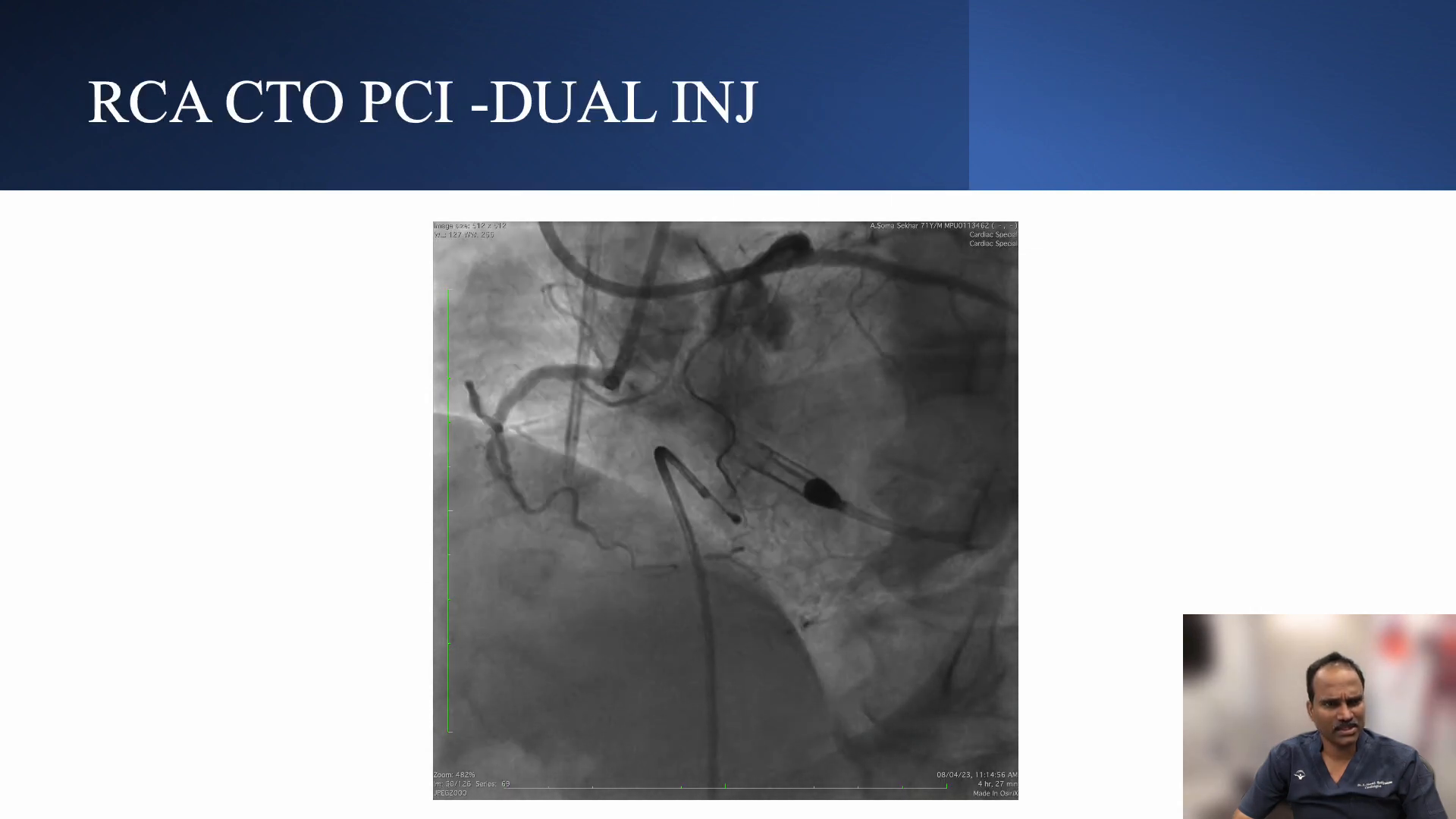
RCA CTO PCI – Dual Injection Strategy
For chronic total occlusions (CTOs) in the right coronary artery (RCA), a dual injection strategy can enhance visualization of the lesion and guide wire navigation. This technique involves using two different catheters to inject contrast simultaneously, providing a comprehensive view of the anatomy and the occlusion.
In this case, a JR catheter was utilized to facilitate the dual injection. The simultaneous contrast injection allowed for better delineation of the RCA and identification of the CTO segment, which is crucial for planning the crossing strategy.
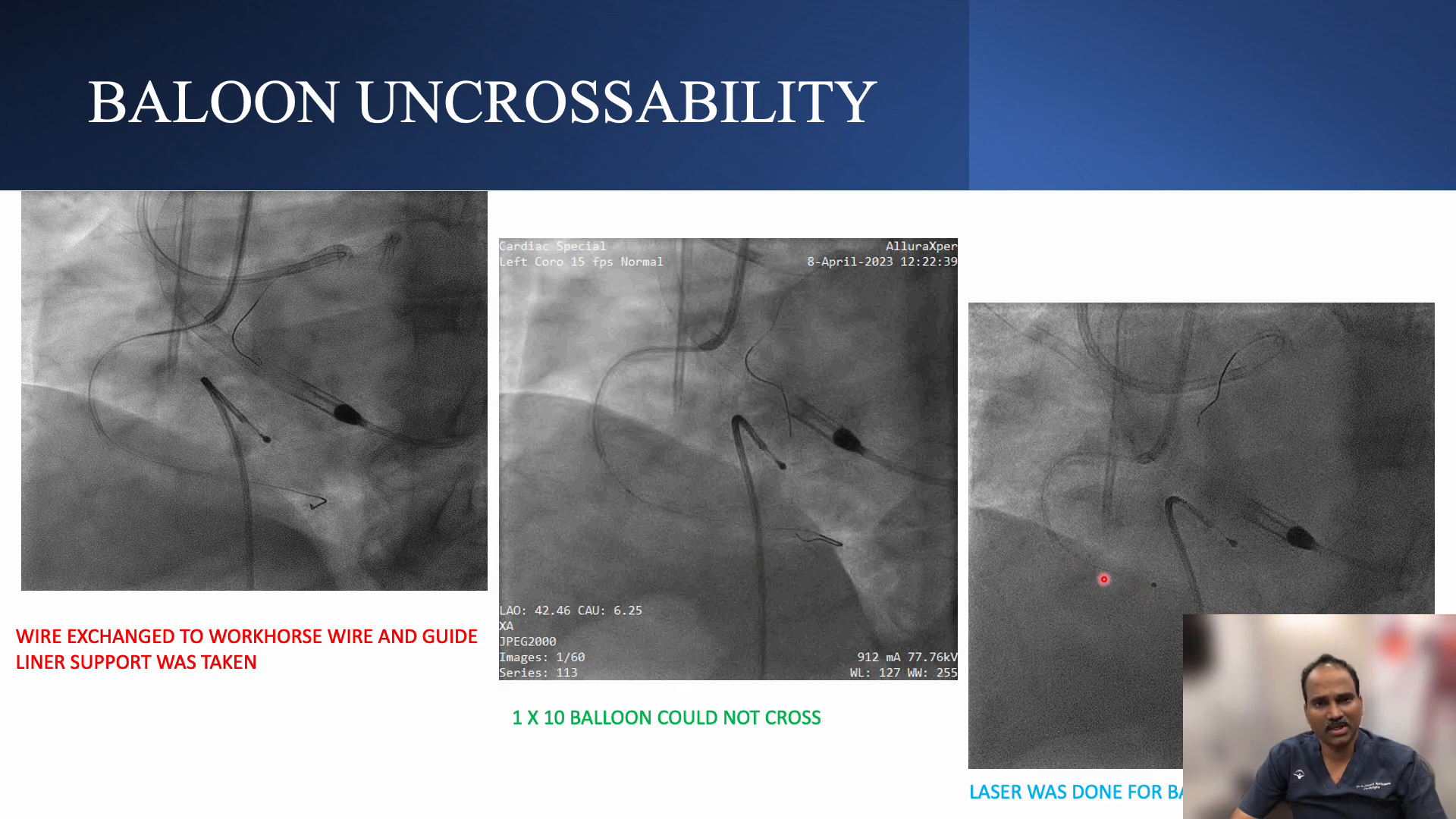
Challenges with Balloon Uncrossability
During the procedure, one of the significant challenges encountered was balloon uncrossability. This is a common issue in complex CTOs, particularly when dealing with heavily calcified lesions. In such cases, alternative strategies must be employed to ensure successful crossing of the occlusion.
Laser atherectomy was utilized as a rescue strategy to modify the plaque morphology, facilitating subsequent balloon dilation. The laser not only helps in crossing the lesion but also prepares the vessel for stenting by creating a more favorable environment for balloon expansion.
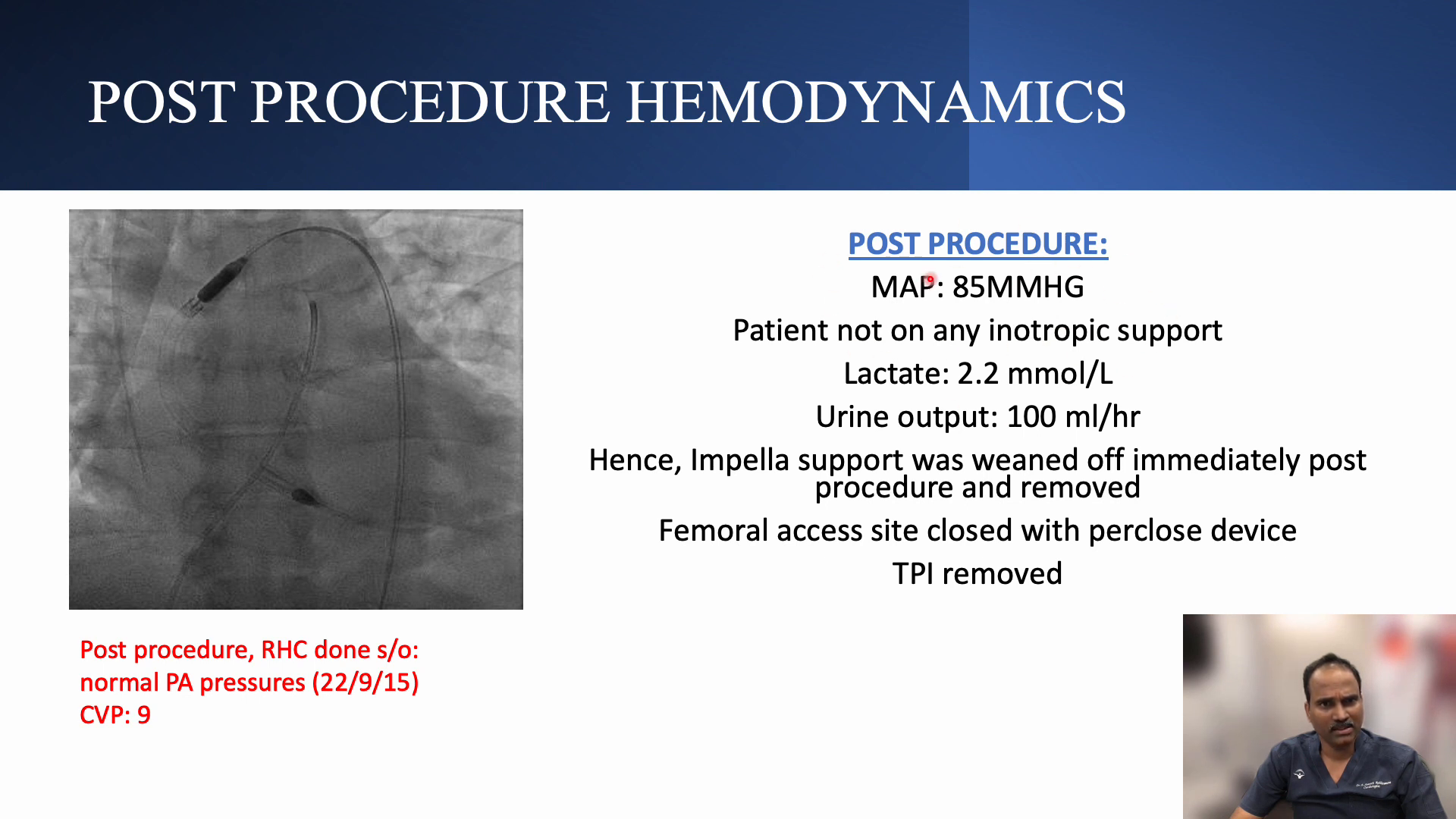
Post Procedure Hemodynamics Assessment
Post-procedure, hemodynamic assessment is crucial to evaluate the success of the intervention. In this case, measurements showed that the mean arterial pressure stabilized, and there was a marked improvement in cardiac output. These results are indicative of successful revascularization and effective management of the patient’s condition.
Monitoring the central venous pressure (CVP) and other hemodynamic parameters post-PCI is essential for ensuring that the patient remains stable and that any potential complications are promptly addressed.
Take Home Messages from the Case
- Importance of Hemodynamic Support: The use of Impella provided critical support in managing the patient’s hemodynamics during the complex PCI.
- Wiring Strategy: Utilizing the stent as a marker significantly simplified the wiring process, enhancing procedural efficiency.
- Balloon Uncrossability Solutions: Laser atherectomy can serve as an effective alternative when encountering challenges with balloon uncrossability.
- Continuous Monitoring: Post-procedure hemodynamic assessments are vital for ensuring patient stability and procedural success.
Frequently Asked Questions (FAQ)
What is the Mini Crush Technique?
The Mini Crush Technique is a method used in bifurcation stenting that involves deploying a stent in one branch, followed by a balloon inflation in the other, to optimize flow and minimize complications.
Why is dual injection used in RCA CTO PCI?
Dual injection enhances visualization of the RCA anatomy and the CTO segment, allowing for more precise wire navigation and treatment planning.
How does laser atherectomy help with balloon uncrossability?
Laser atherectomy helps modify the plaque and calcification, making it easier for the balloon to cross the lesion and achieve optimal dilation.
What are the key takeaways for managing complex PCI cases?
Key takeaways include the importance of hemodynamic support, effective wiring strategies, and the necessity for continuous monitoring post-procedure to ensure patient safety and procedural success.

No Comments